Tissue response represents an important feature in biocompatibility in implant procedures. This review article highlights the fundamental characteristics of tissue response after the implant procedure. This article also highlights the tissue response in compromised osseous conditions. Understanding the histologic events after dental implants in normal and abnormal bone reinforces the concept of case selection in dental implants.
Key points
- •
Tissue (cellular and extracellular) responses following an implant surgery have greater influence over the better prognosis.
- •
Osseointegration is considered to be one of the important tissue responses that are expected following the dental implant surgery.
- •
Patient selection and critical evaluation of tissues need to be done in prior for the patients with compromised bone disorders.
- •
Following the proper guidelines in patients with compromised osseous tissue may help in better prognosis.
Introduction
Dental implants are one of the golden landmarks of modern dentistry. The treatment outcome of dental implants is determined by the degree and type of the tissue responses. The local and systemic responses of the tissue represent a feature of biocompatibility. The function and success of the dental implant rely on the tissue response. It is, therefore, essential to understand the fundamental characteristics of the tissue response to dental implants. This article reviews the tissue response to biomaterials and dental implants, specifically in compromised osseous tissues.
Introduction
Dental implants are one of the golden landmarks of modern dentistry. The treatment outcome of dental implants is determined by the degree and type of the tissue responses. The local and systemic responses of the tissue represent a feature of biocompatibility. The function and success of the dental implant rely on the tissue response. It is, therefore, essential to understand the fundamental characteristics of the tissue response to dental implants. This article reviews the tissue response to biomaterials and dental implants, specifically in compromised osseous tissues.
Tissue response to biomaterials
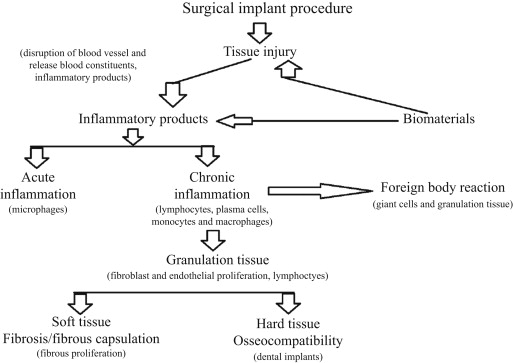
Biomaterials are the biological or synthetic materials that are used to restore a part of a living system and/or to maintain contact with living tissue. The local and systemic responses of the tissue represent an important feature of biocompatibility. Anderson described the term, biocompatibility , as the ability of a biomaterial, prosthesis, or medical device to perform with an appropriate host response in a specific application (i.e., the evaluation of biological responses is a measure of the magnitude and duration of the adverse alterations in homeostatic mechanisms that determine the host response). The fundamental characteristics of tissue response after implantation of the biomaterials are injury, blood material interactions, provisional matrix formation, acute and chronic inflammation, granulation tissue formation, foreign body reaction, and fibrous capsule development ( Fig. 1 ).
An injury begins from the surgical intervention process of implantation and continues postoperatively. Tissue injury predisposes blood vessel disruption with concomitant release of blood constituents. Immediately after the injury, the alterations in the vascular flow and permeability occur, thus initiating the inflammatory response by the escape of blood cells, fluids, and proteins from the vascular component. The injury and perturbation of homeostatic mechanism lead to the cellular cascades of the healing process. The initial acute inflammatory response is activated by injury to the vascular component of the tissue and the blood material interactions.
Provisional matrix formation at the implant site is formed immediately after the injury of vascularized tissue. The provisional matrix is composed of inflammatory cells, fibrin, and endothelial cells. The mitogens, chemokines, cytokines, and growth factors are released in the provisional matrix and influence wound healing process. The components of the provisional matrix initiate the resolution, reorganization, and repair processes. During the process of acute inflammation, the major function of the neutrophils/microphages is to phagocytose microbes and foreign materials. The engulfment and degradation of biomaterial may or may not occur and is greatly dependent on the property of the biomaterial. Generally, biomaterials are not engulfed by microphages/macrophages because of the size disparity. In certain biomaterials, phagocytosis may occur in which they are coated by natural substances, such as serum factors, known as opsonins. These opsonins are recognized by the host tissue and provoke degradation. Furthermore, this degradation process does not involve engulfment of the biomaterial but results in the extracellular release of leukocyte products in an attempt to degrade the biomaterial. The neutrophils release enzymes, the amount of which depends on the size of the biomaterial particle, thus suggesting that activation of inflammatory response in the tissue depends on the size of the implant and the material of the implant, which is phagocytosable or nonphagocytosable. Persistent inflammation at the tissue injury of the implanted site results in chronic inflammation. The presence of lymphocytes, plasma cells, monocytes, and macrophages in the implant site designates the chronic inflammation. The physical and chemical properties of the biomaterial and movement of the implant material predispose the chronic inflammation process. The macrophages are important cells in chronic inflammation, because the macrophages process and present the antigen to the immunocompetent cells, thus initiating the immune reactions.
The formation of the granulation tissue is considered a hallmark of the healing inflammation process. The initiation of granulation tissue formation depends on the site and size of the tissue injury, the formation of which can be anticipated in 3 to 5 days of the implantation. Foreign body reaction is characterized by foreign body giant cells and granulation tissue components. The physical and chemical properties of the biomaterial used, however, determine the composition of the foreign body reaction. Anderson mentions that foreign body reaction in the implant site might be controlled by the surface properties of the biomaterial, form of the implant, and relationship between the surface area of the biomaterial and the volume of the implant. Foreign body reaction with granulation tissue development is considered a normal wound healing response to the implanted biomaterials. Recent studies on oral implants report that osseointegration is a foreign body response to the implant and is a chronic inflammatory response characterized by bone embedding or separation of the implant from the host tissue.
The end stage in the healing response to biomaterials is either fibrosis or fibrous encapsulation. The repair after the implant procedure usually involves 2 processes: regeneration and replacement of connective tissue that comprises the fibrous capsule. The Processes are controlled by the proliferative capacity of cells and persistence of tissue framework of the implant site. The dental implants have a better compatibility with osseous tissue than with soft tissue. The bone bonding strength of the dental implants is high, but the bonding properties with soft tissue are poor and result in the fibrous encapsulation.
Tissue response to dental implants
The tissue involved in the implanted area shows a cascade of cellular and extracellular response at the bone–implant interface until the implant surface is covered with a newly formed bone. The host response after the implantation procedure is modified by the physical and chemical properties of the implant material, stability of the fixation, heat injury, or death of osteocytes during implant procedure. The blood is the first tissue component to come in contact with the implant surface. The blood cells and inflammatory cells from the severed vascular tissue migrate into the tissue around the implant. The platelets are initiated and are responsible for forming a clot in the implant–tissue interface area. The fibrin matrix of the blood clot acts as a scaffold for osteoconduction, and migration of osteogenic cells takes place. Osteogenetic process, which is activated, is similar to bone healing process and is regulated by various growth factors that are released by the blood cells at the bone–implant interface. The mesenchymal tissue formation begins and the osteogenetic process is characterized by (1) woven formation through an intramembranous pathway and (2) lamellar bone formation on the spicules of woven bone.
The blood cells at the implant–tissue interface are activated, resulting in the release of growth factors, cytokines. On initiation and activation of osteogenic cells, eventual differentiation results in osteoinduction at the tissue front, leading to the healing cascade. The newly formed osteoid tissues eventually come in direct contact with the implant surface and result in the osseointegration. The active osteogenic cells’ and mesenchymal cells’ migration to the implant surface starts after 24 hours of the implantation. The cytokines liberated help in the signaling of the cell migration, cell adhesion, and cell proliferation. The signaling process leads to the bone proteins’ deposition over the implant surface, thus creating a noncollagenous matrix scaffold over the implant surface and this regulates the cell adhesion and binds with the minerals. The matrix formed is poorly mineralized bone tissue, and continuous apposition of calcium and phosphorus results in the integration of the implant with adjacent host tissue.
Tissue response in compromised osseous tissues
There is a new paradigm for dental implants in patients seeking oral rehabilitation needs. Dental implants in modern dentistry have gained a significant positive response from the partially or completely edentulous patients. The host response has a significant role in the successfulness of the implant treatment. The perturbance in physiologic conditions may have an impact on the treatment outcome and prognosis. Existing systemic diseases or systemic pharmacologic therapies can influence dental implant treatment outcome. Thus, a preexisting systemic disease or systemic therapy may influence and complicate or contraindicate implant procedures in dental patients. Lesions (discussed later) are characterized according to the disease origin, such as developmental, metabolic, infection, and neoplastic. The recommendations for various osseous lesions for dental implant placement are represented in Table 1 .
| Osseous Lesion | Recommendations for Dental Implant Placement |
|---|---|
| Osteogenesis imperfecta | Dental implant placement is not contraindicated; however, special attention needs to taken to evaluate bone fragility and wound healing properties. |
| Hyperparathyroidism | Dental implant placement is contraindicated in the areas of active bony lesions. In skeletal depletion, it more commonly affects the alveolar bone in comparison with rib, vertebrae, and long bones. |
| Osteoporosis | Dental implant placement is not contraindicated; however, special consideration is recommended in pre-, intra-, and postoperative periods. |
| Osteomyelitis | Dental implant placement is usually contraindicated due to the compromised vascular supply to the affected area of the bone. Dental implants may be placed, however, after the restoration of vascularity in the affected bone. |
| Fibrous dysplasia | Dental implant placement is contraindicated in the region of disorder. The dental implants may be placed after the completion of growth to avoid submerged implants and revision of prosthesis in young patients. |
| Cemento-osseous dysplasia | Dental implant placement is usually not contraindicated; however, a thorough radiographic evaluation is advised. |
| BP therapy | Dental implant may be placed, following the guidelines provided by the American Association of Oral and Maxillofacial Surgeons. |
| Paget disease | Dental implant placement is a relative contraindication due to the diminished bone quality and it interferes with osseointegration. |
| Multiple myeloma | Dental implant placement is a relative contraindication due to the severity of the disease and severe destruction of the bone. |
| Irradiated bone | Because of the higher incidence of dental implant failure, special caution needs to be taken with irradiated patients and a thorough evaluation is required with radiation exposure, type and total cumulative dose and timing, region of implant installation, quality of bone, implant length, and design prior to the implant procedure. |
Osteogenesis Imperfecta
Osteogenesis imperfecta is characterized by impairment of collage maturation and enhanced bone fragility. Higher frequency of bone fractures are noted in type II osteogenesis imperfecta. The wound healing is poor and fracture healing may be associated with exuberant callus formation. Cases have been reported of placement of osseointegrated dental implants in osteogenesis imperfecta that has been successful. Prabhu and colleagues, reported a successful case of 9 years’ follow-up; and Binger and colleagues, reported a successful case of follow-up of 4 years. These data suggest that dental implants are not absolutely contraindicated in patients with osteogenesis imperfecta. Before placement of the dental implants, however, caution is needed regarding bone fragility and wound healing properties.
Hyperparathyroidism
Hyperparathyroidism is characterized by the excessive production of parathyroid hormone. Severe cases of hyperparathyroidism cause bone, renal, and gastric disturbances. In skeletal depletion, it affects alveolar bone before rib, vertebrae, or long bones. The implant placement is contraindicated in the areas of active bony lesions. Implants may be placed after the successful treatment of hyperparathyroidism. Cases have been reported of successful treatment of dental implants in patients with controlled and treated hyperparathyroidism.
Osteoporosis
Osteoporosis is a metabolic bone disorder characterized by reduced mineral density of normally mineralized bone. The concern in this disorder for dental implants is due to the assumption that impaired bone metabolism may influence the osseointegration of implants. Heersche and colleagues, in 1998, discuss that bone remodeling is a nonuniform process; it varies between cortical and trabecular and from site to site. The studies on osteoporotic fractures suggested that, the healing are usually in better fashion which denotes a satisfactory healing and repair response. The study results denotes that the bone remodeling process in osteoporotic patients is not different from those of healthy individuals. Holahan and colleagues, in 2008, suggest that diagnosis of osteoporosis and osteopenia has not contributed to implant failure. Several case reports have indicated that successful placement of dental implants is possible in osteoporosis and steroid-induced osteoporosis, glucocorticoid dependent. Reduced success rate was observed in patients who underwent maxillary sinus augmentation and in female patients without estrogen supplementation. The bone density influences the treatment plan, surgical approach, length of healing, and progressive loading. Implant design needs to be considered with a greater width, and the surface conditions of the implant material need to be designed to increase bone contact and density.
Beikler and Flemmings, discuss the pre-, intra-, and postoperative special considerations for dental implant therapy in patients with bone metabolic disease. The 2 considerations for pre- and intraoperative considerations are (1) thorough examination and evaluation of the causative factors for bone disease and treatment and (2) necessary bone augmentation procedures. The 3 postoperative considerations are (1) physiologic doses of vitamin D (400–800 IU/d) and calcium (1500 mg/d) in the postoperative period; (2) the healing period is increased by 2 to 8 months in maxillae and 6 months in mandible; and (3) careful occlusal adjustments and observation for the occlusal overload are required.
Osteomyelitis
Osteomyelitis is inflammation in the medullary spaces or cortical surfaces of bone, histologically characterized by the sequestrum and involucrum. Based on the duration, it can be an acute- or chronic-type osteomyelitis is usually contraindicated for placement of dental implants after the restoration of vascularity in the affected bone.
Fibrous Dysplasia
Fibrous dysplasia is a developmental tumor-like condition affecting jaw bones, which is histologically characterized by replacement of normal osseous tissue by an excessive proliferation of fibrocellular connective tissue stroma intermixed with irregular-appearing bony trabeculae. Lack of osseous tissue and increased amount fibrous tissue in these lesions predispose to decreased rigid fixation of the dental implant. The reduced fixation increases the chance of local infection and spread of the infection further complicates the dental implant treatment outcome. On successful completion of treatment of fibrous dysplasias, patients may receive the implants. Case reports have shown successful dental implants in treated fibrous dysplasia and McCune-Albright syndrome. Recommendations have been made for screening procedures and management of endocrinopathies associated with fibrous dysplasia. The dental implants may be placed after a young patient has completed growth to avoid submerged implants and revision of prosthesis.
Cemento-osseous Dysplasia
Cemento-osseous dysplasia is the most common fibro-osseous lesion in dental practice and the lesion is histologically characterized by the fibrocellular connective tissue stroma with avascular cementum–like areas. The 3 types of this disorder are focal, periapical, and florid cement osseous dysplasia. Cases have been reported of dental implant placement and successful results in florid cemento-osseous dysplasia. Recently, a case was reported of implant failure after 26 months in a patient, and the histopathologic evidence suggested concomitant florid cemento-osseous dysplasia with cemento-ossifying fibroma. The investigators of this report recommended a thorough radiographic evaluation of dental arch to locate suspected bony lesions that may lead to implant failure. The dental implants are not contraindicated; however, radiographic evaluation for the presence of sclerotic bone is required, which indicates the hypovascularity. This bone has a chance of become infected and result in the failure of healing.
Bisphosphonate-Treated Patients
Bisphosphonates (BPs) are drugs used in the management of osteoporosis, Paget disease, metastatic bone neoplasm, breast cancer, multiple myeloma, and malignant hypercalceima to increase survival and quality of life. The oral and intravenous BPs bind with bone and inhibit the osteoclast activity and osteoclastic bone resorption and induce their apoptosis. The recent BPs include nitrogen in their molecules, which inhibits tumor proliferation and angiogenesis. Depending on the strength and half-life of BPs, the complication of osteonecrosis development may be observed. The frequency of development of osteoradionecrosis are greater with intravenous therapy than oral delivery of BPs. The fast development of osteoradionecrosis among intravenous BP users is due to higher and more rapid accumulation of these drugs in the bone. The results of experimental studies on animals indicate a better osseointegration of dental implants with BPs. Case reports of dental implant placement in patients receiving BPs have been reported, however, with development of osteoradionecrosis of jaw. The inconsistent results obtained in animal experimental studies and human cases may be due to the short medication and follow-up period with BPs in animal studies. Grant and colleagues, in 2008, in their review of 115 cases, reveal that oral BPs do not seem to significantly affect implant success and suggest that all patients undergoing implant placement should be questioned about BP therapy, including drug taken, drug dosage, and length of treatment prior to surgery.
The American Association of Oral and Maxillofacial Surgeons has provided guidelines for patients treated with BPs. (1) If BP is administered intravenously in cancer patients, dental implant placement is contraindicated. (2) If BP is taken orally, 3 possibilities exist: (a) In patients treated with BPs for less than 3 years who have no clinical risks, dental implants can be placed without altering the conventional surgical treatment; (b) If patients have been treated for fewer than 3 years and are treated jointly with corticoids, BPs must be removed 3 months before and not administered again, until the bone has completely healed; and (c) If patients have taken BPs for more than 3 years, it is possible to place dental implants if BPs are removed for 3 months before surgery and not administered again until the bone has completely healed.
Paget Disease
Paget disease of bone is characterized by abnormal and anarchic resorption and deposition of bone, resulting in distortion and weakening of the affected bones. Paget disease is a relative contraindication for dental implant placement due to the diminished bone quality and it interferes with osseointegration. Cases have been reported of placement and survival of dental implants in remission cases of Paget disease and patients under BP therapy. Rasmussen and Hopfensperger, in 2008, report that on surgical placement of dental implants, poor quality of bone was observed.
Multiple Myeloma
Multiple myeloma is a malignant neoplasm of plasma cell origin that often seems to have a multicentric origin within the bone, with osteolytic destruction of the bone. Pathologic fractures are often noted in some cases due to the osteolytic destruction. The dental implant placements in this neoplastic condition are a relative contraindication due to the severity of the disease and severe destruction of the bone. A case was reported of dental implant placement in a patient with multiple myeloma who wished to maximize his quality of life. The reported case was reported as successful.
Irradiated Bone
Radiotherapy results in the hypovascular, hypoxic, and hypocellular state of hard and soft tissue. Caution needs to be taken prior to the placement of dental implants. The radiation exposure, type of and total cumulative dose and timing, region of implant installation, quality of bone, implant length, and design need to be evaluated prior to implant therapy. Implant prostheses are recommended rather than soft tissue prosthesis in irradiated patients, which reduce the possible soft tissue irritation in these patients. The failure rate of dental implants in irradiated patients may be reduced by adjunctive hyperbaric oxygen therapy.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


