Virtual 3-dimensional planning in orthognathic surgery allows for a detailed visualization and analysis of skeletal and dental deformities, especially in patients with asymmetries. This approach also eliminates conventional stone model surgery through computer-aided fabrication of surgical stents. This article presents a new approach with 3-dimensional cone-beam computed tomography-based treatment planning for the surgical correction of facial asymmetry in conjunction with the surgery first approach. Good esthetic and occlusal outcomes were obtained for 2 patients after orthognathic surgery and orthodontic treatment with a short total treatment time.
Conventional surgical planning for orthognathic surgery involves collection of data, including a clinical examination, extraoral and intraoral photographs, lateral and posteroanterior cephalograms, and plaster dental models. Dental models are mounted on an articulator, and the interdisciplinary team of the orthodontist and the oral-maxillofacial surgeon evaluates, simulates, and decides on a treatment plan. A surgical splint is fabricated to the newly determined dental occlusion. The main limitation of conventional surgical planning is its 2-dimensional approach, a major handicap especially in patients with facial asymmetries, when often the deformity involves all 3 dimensions. Appropriate surgical treatment starts with accurate diagnosis by evaluating all dimensions and determining the nature of the asymmetry because it might be a combination of hard-tissue and soft-tissue components.
To overcome those shortcomings, cone-beam computed tomography (CBCT) for imaging the craniofacial region heralds a true paradigm shift from a 2-dimensional to a 3-dimensional (3D) approach. CBCT allows a 3D display of the craniofacial anatomy with possibilities of image segmentation, thereby expanding the role of imaging from diagnosis to simulation of the surgical procedures and fabrication of the surgical splints in craniofacial surgery. Three-dimensional computer-aided surgical planning techniques for craniofacial deformities introduced by Xia et al and Swennen et al allow 3D analysis and a virtual surgical plan and provide the information for fabrication of computer-manufactured surgical splints without conventional model surgery. This virtual planning allows for more thorough analysis and surgical planning, especially in patients with facial asymmetries.
Before the 1960s, most orthognathic surgeries were performed either without orthodontic treatment after removing the orthodontic appliances, or before any orthodontic treatment. Later, the 3 stages of conventional surgical orthodontic treatment became popular because of the stability of the results and satisfaction with the posttreatment outcomes. Successful outcomes were due to the development of new surgical techniques and orthodontic materials and the use of rigid internal fixation. However, longer treatment times and transitional detriment to the facial profile have led to a new approach called “surgery first,” which eliminates the presurgical orthodontic phase.
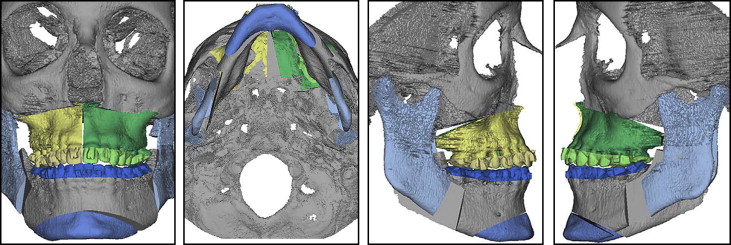
The purpose of this article is to document the treatments of 2 patients with facial asymmetry who had orthognathic surgery with the surgery first approach with 3D computer-aided surgical planning based on 1 CBCT scan procedure as described by Xia et al. A virtual composite skull model was created with Simplant OMS software (Materialise, Leuven, Belgium). A computer-aided surgical stent was manufactured for 1 patient based on the occlusion of the projected skeletal outcome.
Patient 1 was a 22-year-old white woman who reported to the orthodontic clinic at the University of Connecticut Health Center with a chief complaint of forwardly placed maxillary incisors ( Fig 1 ). She had a convex profile caused by a retrognathic mandible ( Fig 2 ; Tables I and II ), vertical maxillary excess with an occlusal cant, and transverse maxillary constriction. Dentally, she had a Class II molar and canine occlusion, an upper midline shifted to the right side, a unilateral posterior crossbite on the left side, an increased overjet, and an anterior open-bite tendency. Her smile showed excessive gingival display and increased buccal corridors, indicating a narrow maxillary arch. Additionally, she had facial asymmetry with the chin point deviated toward the left. The patient had been previously treated orthodontically for an asymmetric Class II malocclusion with maxillary transverse deficiency, and the maxillary right first premolar was extracted at that time.


| Variable | Norm | Pretreatment | Posttreatment | Change |
|---|---|---|---|---|
| SNA (°) | 82 | 78 | 79 | 1 |
| SNB (°) | 80 | 72 | 76 | 4 |
| ANB (°) | 2 | 6 | 3 | −3 |
| FMA (°) | 32 | 31 | 28 | −3 |
| IMPA (°) | 90 | 91 | 96 | 5 |
| U1-NA (mm) | 4 | 4.5 | 5 | 0.5 |
| L1-NB (mm) | 4 | 4.5 | 6 | 1.5 |
| Interincisal angle (°) | 131 | 128 | 125 | −3 |
| Upper lip to E-line (mm) | −4 | −4.5 | −4 | 0.5 |
| Lower lip to E-line (mm) | −2 | −2.5 | −4 | −1.5 |
| Variable | Norm | Pretreatment | Posttreatment | Change |
|---|---|---|---|---|
| Occlusal plane tilt (°) | 0 | 2 | 0 | −2 |
| AG right-MSR (mm) | 34 | 34 | 34 | 0 |
| AG left-MSR (mm) | 34 | 34 | 37 | 3 |
| J-MSR, right (mm) | 29 | 23 | 25 | 2 |
| J-MSR, left (mm) | 29 | 25 | 28 | 3 |
| A-Me-MSR (°) | 0 | 5.5 | 0 | −5.5 |
| Z-MSR, right (mm) | 41 | 36 | 36 | 0 |
| Z-MSR, left (mm) | 41 | 37 | 37 | 0 |
| AG right-Me (mm) | 40 | 48 | 42 | −6 |
| AG left-Me (mm) | 40 | 45 | 44 | −1 |
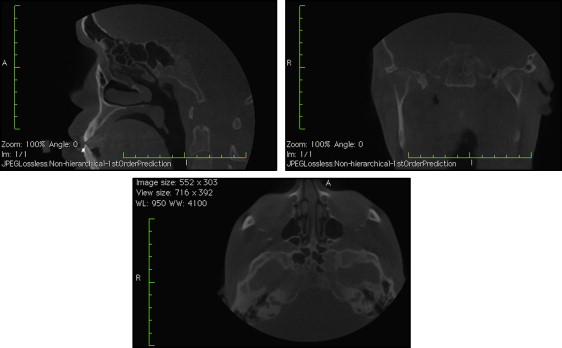
Patient 2 was a 26-year-old white man requesting correction of his underbite and crooked smile at the Oral and Maxillofacial Surgery clinic of the University of Connecticut Health Center. The clinical examination ( Fig 3 ) showed a mild concave skeletal and soft-tissue profile caused by a retrusive maxilla and a slightly prognathic mandible. The pretreatment CBCT image ( Fig 4 ) also showed an incidental finding of a lesion at the base of the skull. As a follow-up, magnetic resonance imaging was taken by a medical radiologist, who gave clearance for the orthognathic surgical procedure and recommended a 6-month follow-up based on the likely nonaggressive nature of the lesion.

From a frontal view, a maxillary cant with slightly excessive gingival display on the right was evidenced on smiling. Facial asymmetry was appreciable in the lower third of the face, with the chin deviated toward the left in relation to the facial midline. Dentally, the patient had Class III molar and canine relationships, an anterior crossbite, a mandibular midline shifted to the left, and compensated retroclined mandibular incisors. He had also been treated orthodontically during his adolescence.
The treatment objectives for both patients aimed to address their chief complaints and correct their facial asymmetries. Treatment goals consisted of correlating the maxillary midline to the facial midline, and the frontal occlusal plane parallel to the horizontal plane in natural head position and the chin point in line with the facial midline. Both patients required asymmetric maxillary impaction. From a profile perspective, patient 1 required a significant mandibular advancement to achieve ideal facial convexity. On the other hand, patient 2 required maxillary advancement and unilateral mandibular setback to achieve a balanced profile. Patient 1 required expansion of the maxilla, especially on the left side. Alignment was good, and a nonextraction approach was chosen for both patients. Since they already had previous orthodontic treatment, they were concerned about having to undergo it again. The surgery first approach was offered as a treatment option, and both patients accepted because it addressed their chief complaints while minimizing the time required with fixed orthodontic appliances.
In patient 1, 4 weeks before surgery, the maxillary and mandibular teeth were bonded with 0.022-in slot preadjusted edgewise appliances, and the molars were banded. The canine and premolar brackets had built-in hooks; additionally, surgical hooks were crimped interdentally between the anterior teeth on the 0.016 × 0.016-in nickel-titanium archwire. The archwire was removed and ready to be used in the operating room before the start of surgery. A CBCT scan (exposure time, 14 seconds; field of view, 12 in; voxel size, 1.25 mm) based on the Simplant OMS guidelines was taken for the construction of a composite skull model. The virtual surgical plan consisted of a LeFort I maxillary osteotomy with expansion, advancement, impaction, and bilateral sagittal split osteotomy for mandibular advancement with lateral sliding genioplasty ( Fig 5 ). Analysis of the surgical simulation shows the differential movements of the maxilla and the mandible to correct the facial asymmetry. The planned virtual surgery was replicated by stone model surgery, and acrylic splints were fabricated.