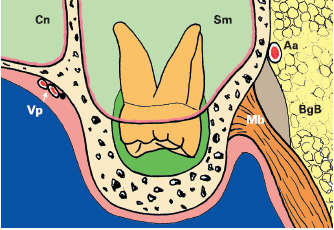
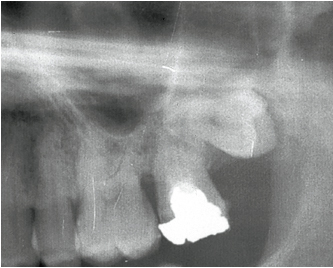
• The bone crypt develops around the tooth germ inside the tuberosity, which represents the extension of the maxillary alveolar process. Bone trabeculation is less dense than in the mandible. It is surrounded by a thinner cortical bone plate, which renders the posterior wall fragile and likely to fracture during an extraction procedure (Fig 12-1).
• The tuberosity is covered with the mucoperiosteal gingival tissue. The posterior limit of this gingival surface includes the pterygomaxillary groove and, laterally, the alveolar mucosa, which lines the bottom of the vestibule (Fig 12-2a).
• The insertions of the buccinator muscle extend beyond the bottom of the vestibule. These may be reflected with the periosteum when creating the flap. They should be replaced in their original anatomic position at the end of surgery (Fig 12-2b).
• When an extensive flap is required, the periosteal tissue is carefully removed along with the buccinator fibers; tearing of the periosteum could lead to exposure of the area that contains Bichat’s fat ball and the release of this fat tissue mass into the surgical site (see Fig 12-2b).
• The relationship between the sinus and the third molar is variable:
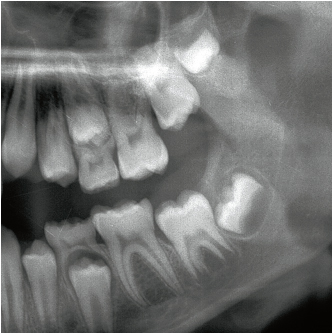
• The inferior wall of the sinus is sometimes associated with the apices of the third molar (Fig 12-3).
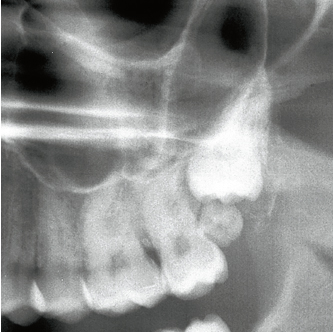
• The posterior sinus wall may form the anterior wall or the lateral walls of the bone crypt (Fig 12-4).
• Following extraction, the sinus tends to progressively fill the empty socket.
• Calcification of the tooth bud occurs as early as 8 to10 years of age, and tooth emergence occurs mainly between the ages of 17 and 21 years, when the first third of the root has developed. Root configuration is quite variable:
• 75% of the roots are fused and are most often short and conical.
• Root divergence may sometimes be strongly marked. The orientation or individualization of the palatal root is often masked by the buccal roots (see Figs 12-18a and 12-18d).
• If there are several roots, their orientation and extreme thinness will result in surgical complications.
• The displacement of the ramus coronoid process is an anatomic factor that limits surgical access. Therefore, limiting the area of the incision and lateral displacement of the mandible will facilitate the clinician’s work.
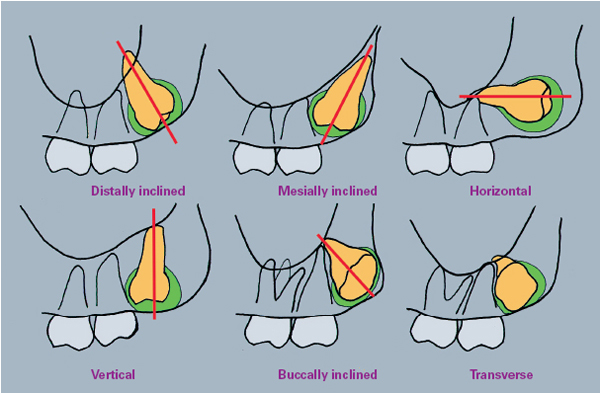
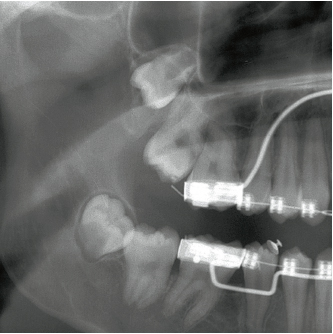
As in the case of the mandible, the degree of difficulty increases with the depth of impaction. Radiographs will show the orientation of the tooth’s great axis in relation to that of the second molar, which may be distally inclined, mesially inclined, horizontal, vertical, and sometimes transverse (Figs 12-5 to 12-7).
Intraoral examination and radiographic images will show the position of the tooth. When it is developing or impacted, inflammatory pericoronitis is much less frequent than in the mandible. The indication for extraction of the third mandibular molars may be prophylactic. This indication may also be included in the planning of orthodontic treatment (Fig 12-8).
Inspection using a mirror and probe is carried out when mouth opening is limited to 25–30 mm. If the tooth is in a submucosal situation, palpation with the index finger indicates the bone texture or the shape cusp tips. However, this procedure is mainly used to measure the size of the tuberosity in the anteroposterior dimension and is not an accurate method for determining the depth of the impaction. The methods used for determining anatomic specificities in this region emphasize the lack of direct visibility, which is frequently compensated for by the clinician’s tactile sense.
In the majority of cases, extraction is carried out without sectioning the tooth because this is a difficult procedure to control. The operator must avoid excessive and inadequately directed mechanical maneuvers that may be likely to induce:
• Projection of the tooth into the sinus
• Displacement of the tooth into the pterygomaxillary fossa or the buccal soft tissues (Figs 12-9a and 12-9b)
• Root fractures
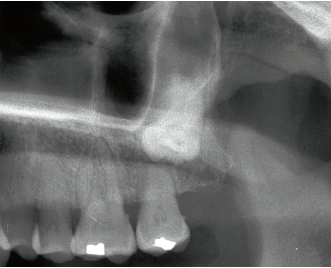
12-6 In this 70-year-old female patient, the left maxillary third molar is vertically impacted, and its location against the posterior wall of the sinus has induced the root resorption of the adjacent second molar. In the absence of clinical symptoms, extraction is contraindicated in such cases.
Anesthesia of the maxillary molars is either periapical or complete nerve block. Targets of anesthesia a/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses