In the early days of fixed-appliance orthodontic treatment, brackets were welded to gold or stainless steel bands. Before treatment, the orthodontist had to create enough space around each tooth to accommodate the bands, and then those spaces had to be closed at the end of treatment, when the bands were removed. This was time-consuming for the orthodontist and uncomfortable for the patient. Banded appliances frequently caused gingival trauma when fitted, and decalcification could occur under the band. In the mid-1960s, Dr George Newman, an orthodontist in Orange, New Jersey, and Professor Fujio Miura, chair of the Department of Orthodontics at Tokyo Medical and Dental University in Japan, pioneered the bonding of orthodontic brackets to enamel. Many developments have occurred in the decades that followed, including many new adhesives, sophisticated base designs, new bracket materials, faster or more efficient curing methods, self-etching primers, fluoride-releasing agents, and sealants. The purpose of this article is to review the history of orthodontic bonding, especially the materials used in the bonding process.

From the inception of fixed-appliance orthodontic treatment, brackets traditionally have been welded to gold or stainless steel bands. The band encompassed the tooth circumferentially, requiring the creation of interproximal space to accommodate the width of the band material. This separation process, which was accomplished initially by placing wires and later elastomerics, was time-consuming for the orthodontist and uncomfortable for the patient. At the conclusion of treatment, these interproximal gaps had to be addressed again. In addition, banded appliances frequently caused gingival trauma when fitted, and decalcification under bands sometimes occurred during treatment. Therefore, the obvious solution to these problems was for the clinician to attach the brackets directly to tooth enamel, thus eliminating the need for bands.
Dr George Newman, an orthodontist in Orange, New Jersey, and Professor Fujio Miura, chair of the Department of Orthodontics at Tokyo Medical and Dental University in Japan, pioneered the bonding of orthodontic brackets to enamel. Coincidentally, they both began their experimentations in the mid-1960s. It is unfortunate that they lived on different continents, since they both had the same passion and vision—the development of an adhesive that would bond plastic brackets directly to enamel with enough strength to withstand the forces of occlusion during treatment, mastication, and archwire stress while allowing for biomechanical control and allowing for removal of the brackets without causing significant damage to the enamel. In addition, bonding had to be accomplished in a humid environment and needed to last from bracket placement through the final phase of treatment.
In the early 1970s, Miura developed a technique for bonding polycarbonate plastic brackets to phosphoric acid−etched enamel using a restorative filling material developed by Masuhura et al, also at Tokyo Medical and Dental University. The adhesive, Orthomite (Rocky Mountain Orthodontics, Denver, Colo), consisted of methyl methacrylate and polymethyl methacrylate with tri-n-butylborane as the catalyst. Miura found that the bond strength decreased with time as a result of exposure to oral fluids. In addition, mastication and abrasive metal archwires used with plastic brackets resulted in broken tie wings and deformed archwire slots. However, this system became popular as an alternative to bands and fueled the research to develop stronger adhesives and more durable plastic attachments, with an end goal of eventually developing bondable metal brackets. Other methyl methacrylate and polymethyl methacrylate systems followed from GAC International (Bohemia, NY) and TP Orthodontics (LaPorte, Ind) with the same successes and drawbacks.
Newman continued his work with epoxy resins, while Retief et al from South Africa developed an adhesive to bond metal brackets, based on research conducted by Bowen on epoxy resins. Epoxy resins did not experience significant polymerization shrinkage when setting, had the same coefficient of thermal expansion as enamel, and were cross-linked to minimize water absorption. These characteristics produced the strength needed to resist the inherent mechanical and masticatory forces. The final hurdle was increasing the strength of the brackets so that they could withstand the forces of 3-dimensional mechanics.
Retief et al partnered with 3M Unitek (Monrovia, Calif) to develop a mesh grid welded onto flattened stainless steel band material with a metal bracket welded to it. Strangely, this metal bracket/pad design was not available commercially until the late 1970s. The primary drawback to that design was that the weld spots on the mesh base prevented the adhesive from flowing between the mesh and the foil pad properly, resulting in reduced mechanical retention.
In the mid-1970s, Lexan plastic (General Electric, Fairfield, Conn) was used to fabricate anterior brackets for patients demanding better esthetics. This improved polycarbonate was harder and consequently less susceptible to wear and tie-wing fracture; however, it still was not as durable or reliable as stainless steel. Eventually, the continued demand for improved esthetics led to the development of ceramic materials for clear brackets. Ceramic was able to withstand forces, did not break or discolor, and still is a material of choice for appliances that are esthetically pleasing.
In the early 1970s, 3M Unitek’s Concise and Adaptic from Johnson & Johnson (New Brunswick, NJ) were popular composite restorative filling materials, formulated from the research conducted previously by Bowen. Both systems used a 2-paste bisphenol A glycidyl methacrylate (BisGMa) resin with quartz as a filler and amine-peroxide as the catalyst. These systems were cross-linked adhesives that experienced minimal polymerization shrinkage. Both systems required acid etching of the enamel with a 40% concentration of phosphoric acid. An unfilled resin then was applied to the enamel as a wetting agent, and the metal brackets were bonded to the conditioned enamel with a chemically cured paste.
At this time, metal brackets were welded to a perforated base ( Fig 1 ). The adhesive became interlocked through the perforations to provide mechanical adhesion. The only complaint with perforated base brackets was that the adhesive covering the base through the perforations was affected by the oral environment so that it often became stained and discolored during routine orthodontic treatment.

To bond chemically to the 2-paste epoxy resin adhesive, plastic brackets had to be coated with methyl methacrylate plastic conditioner before paste application. Several 2-paste chemically cured systems entered the marketplace shortly thereafter. In 1974, Dentsply/Caulk (Milford, Del) introduced the first single-paste ultraviolet (UV) light curable bracket adhesive, Nuva Tach; this system used a UV unfilled bonding resin (Nuva Seal) on the enamel and a single UV curable paste (Nuva Tach).
The paste and the unfilled resin were polymerized with light-emitting energy in the 280-nm range. These UV light-cured composites, like their chemically cured predecessors, originally were introduced as restorative materials with a slight modification in paste viscosity. Unlike the chemically cured systems, however, the UV light-cured system did not have working-time constraints. This characteristic allowed the clinician unlimited working time to place brackets, clean peripheral paste flash, and, if necessary, change bracket position before curing. However, the use of these UV light-cured systems was cut short when it was discovered that they were harmful to exposed skin and eyes, sometimes even resulting in burned soft tissues. Also, these UV systems used the perforated base metal brackets.
In 1975, while working at Lee Pharmaceuticals (South El Monte, Calif), I had an idea for a no-mix, chemically cured direct bonding system that would require the clinician to apply a liquid activator to the etched enamel and to the metal (or plastic) bracket base. A single paste would be applied to the primed bracket base that then would be placed on the tooth and pressed into position. The liquid activator from the enamel and bracket base mixed with the paste and resulted in polymerization. This system eliminated the mixing steps of Adaptic and Concise. The system yielded effective strength, but it depended on how well the bracket base fit the corresponding enamel surface. A flush fit produced the strongest bond. The chemistry of this product was perfected in 1980 by Dr Byoung Suh, a renowned polymer chemist in the dental industry. His formula for this type of adhesive still is used today.
The strength and working time of 2-paste self-curing composites afforded manufacturers the flexibility to develop specialty adhesives to suit the needs of clinicians. In the early 1980s, McNamara and McNamara and Howe introduced a version of the Herbst appliance, the acrylic splint design, that was made from 3-mm-thick splint Biocryl (Great Lakes Orthodontic Products, Tonawanda, NY). Soon thereafter, the acrylic splint expander was developed as a mixed-dentition appliance for the treatment of maxillary constriction and Class III malocclusion. Both appliances necessitated the bonding of splint Biocryl to the maxilla, a procedure that required a strong, thin paste that adhered well to plastic and resisted washout from under the appliance. Excel was developed in 1983 by Reliance Orthodontic Products (Itasca, Ill) specifically for bonding large acrylic appliances. Excel allowed appliances to be bonded and removed successfully without decalcification occurring during treatment.
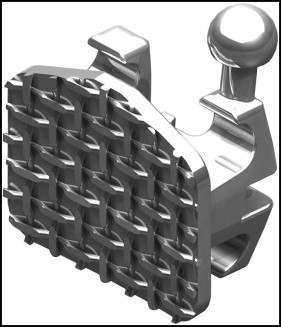
In 1979, Ormco (Orange, Calif) developed and patented a technique to braze mesh to a metal foil pad, eliminating strength-reducing weld spots ( Fig 2 ). This design allowed the adhesive to penetrate between the mesh and the foil pad, thus increasing mechanical retention (this process of brazing still is used by bracket manufacturers that offer foil/mesh metal brackets.) The new Ormco foil-mesh base contained the adhesive under the pad where it would not be susceptible to discoloration, resulting in improved esthetics.
In the early 1980s, visible light–cured restorative materials were introduced in all areas of dentistry. These materials became increasingly popular for bonding orthodontic brackets, lingual retainers, and bands for the same reason that the UV light–cured materials were popular—they allowed unlimited work time. Unlike their UV predecessors, however, the catalyst for these adhesives was camphorquinone, which cured in the visible light range (440-480 nm) with a quartz-tungsten-halogen light, making them safe for exposed eyes and skin.
An essential element of these systems (as is the case today) is achieving proper light penetration under the metal bracket base. The unfilled resin and paste in a light-cured system contain a catalyst. All curing light counterparts emit photons. The catalyst absorbs the photons, and polymerization occurs. The key to success with this system is to have as many photons as possible contact the paste directly.
The 3 keys to complete light polymerization are intensity, proximity, and duration. Keeping these factors in mind, the operator curing the composite under a metal bracket base must be cognizant of the intensity of the light to properly position it relative to the composite; the clinician also must use the correct amount of time required to completely cure with a specific light. To completely cure such a composite, 10,000 mJ of energy are required. The formula to accomplish this is the following: intensity of curing light (MW/cm 2 ) × curing time (in seconds) = 10,000 (mJ/cm 2 ).
In the early 1980s, there were areas of the United States in which the enamel of certain patients was so hard because of the fluoride in the water supply that etching the enamel with any concentration of phosphoric acid was unsuccessful. In 1985, Suh produced Enhance for Reliance Orthodontic Products, which made bonding to fluorosed and atypical surfaces possible with any chemical or light-curing system. Enhance was applied on the etched enamel before the unfilled resin. In addition, the monomer in Enhance (biphenyl dimethacrylate) bonded chemically to composite and metal. Clinicians now had the ability to bond to any metal surface without using a metal primer (such as 4meta) or to a composite restoration without using a plastic conditioner (methyl methacrylate).
Crypsis, a color-change adhesive, was introduced in 1986. This 2-paste dual-cure bracket adhesive was developed and marketed by Orec (Beaverton, Ore). The 2-paste material was yellow after it was mixed and during the gel period, but it turned tooth color when it polymerized. This color characteristic allowed the operator to see the composite flash around the bracket base and remove it before it polymerized. The color-change mechanism was a function of the light-cure catalyst.
In 2004, several single-paste light-cured, color-changing adhesives entered the market from Reliance Orthodontic Products, 3M Unitek, and Ormco. The color-change mechanism in the bracket adhesive from Ormco was temperature induced and could be reversed to show adhesive remnants left behind at debonding by simply introducing cold water into the oral environment. Fluorescing light-cure pastes and sealants also became available at this time with Lumilux LV (Honeywell International, Chicago, Ill), a UV marker that discloses adhesive before and after bonding when illuminated with a black light.
In 1995, Silverman et al developed a technique for bonding metal brackets to wet enamel with no acid etching using Fuji Ortho LC (GC America, Alsip, Ill), a dual-cure glass ionomer cement. This 2-part system comprises a powder (fluoroaluminosilicate glass) and a liquid (polyacrylic acid, water, hydroxyethyl methacrylate [HEMA], and camphorquinone-light activator). The patient’s enamel is cleaned, rinsed, and dried. The powder and liquid are mixed together and applied to a metal bracket base, and the bracket is placed on the enamel. The paste under the bracket base is light cured for 20 seconds per bracket with a curing light. After 5 minutes, the clinician can place an active archwire.
How does this adhesive adhere to nonetched enamel? The polyacrylic acid etches the enamel because it serves as the catalyst for chemically cured polymerization. All powder-liquid glass ionomer cements work in this manner with a self-etching mechanism. However, unlike chemically cured glass ionomer cements that take 20 minutes to reach adequate strength to ligate a bracket, the addition of a light activator makes Fuji Ortho LC practical for bracket bonding. In addition, the hydrophilic property of Fuji Ortho LC allows a bracket to be placed on a slightly contaminated surface.
Unfortunately, the shear bond strength of Fuji Ortho LC in its ideal state is considerably less than that of the highly filled, cross-linked hydrophobic bracket composite. Compton et al reported that even with nitric acid conditioning of the enamel, the shear bond strength value of a dual-cured glass ionomer cement to enamel was 17.2 MPa. Proffit et al reported that forces generated on brackets in the posterior quadrants exceeded 20 MPa. Additionally, the hydrophobic composites maintain their strength over time, enduring exposure to oral fluids better than glass ionomer cements. However, glass ionomer cement, especially dual-cure cement, is a necessary tool when the clinician is trying to bond a band, crown, or bracket in a wet field.
In 1996, 3M Unitek introduced a metal bracket system with a light-cured adhesive preapplied to the base. The operator simply etched the enamel surface, applied an unfilled resin to the enamel, and placed the bracket. The prepasting by the bracket manufacturer eliminated the need for an assistant to place the composite on the bracket base.
In 1998, several hydrophilic primers were introduced. Ortho Solo (Ormco), Assure (Reliance Orthodontic Products), and MIP (3M Unitek) were hydrophilic bonding resins that bonded well to wet or dry enamel, making the bonding procedure more forgiving. In addition, Assure would bond to atypical enamel such as fluorosed enamel, aprismatic enamel, and primary enamel and to dentin. Assure contained biphenyl dimethacrylate, which allows the operator to bond to gold, amalgam, stainless steel, and composite restorations without metal or plastic primers.
Bonding to porcelain always has been a problem for the orthodontic professional. Not only is adequate adhesion required to withstand the forces of treatment, but the surface must be restored to a high luster finish after the appliance is removed. The first porcelain surface produced was fabricated from glass. Clinicians were able to achieve acceptable shear bond strength values when the porcelain was roughened with a fine diamond and treated with silane. As time passed, a portion of the glass was removed, and other materials such as aluminum oxide were added to improve structural stability and esthetics. As a result, adhesion became more difficult.
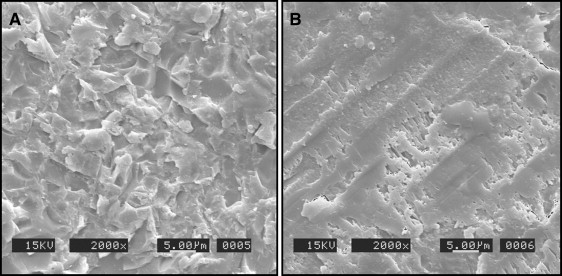
Microetching (sandblasting) became the mechanical preparation of choice in the dental restorative field in the early 1990s. Aluminum oxide, the preferred abrasive powder for intraoral microetching, created fine surface roughness and significantly increased the mechanical retention to artificial surfaces ( Fig 3 ). In addition, microetching allowed for a quick and easy high luster restoration process. This mechanical preparation has been shown to increase adhesion to these surfaces by as much as 100%.