The Alimentary Canal
Digestion and Absorption
• Discuss factors that influence food intake.
• Describe general functions of each digestive organ.
• Identify chemical secretions necessary for digestion of energy-containing nutrients and in what parts of the gastrointestinal tract they are secreted.
• Point out the nutrients that require digestion and the digested products that can be absorbed.
• Explain the role of gastrointestinal motility in digestion and absorption.
• Choose points in Nutritional Directions for educating dental patients.
• Describe how digestion and absorption may affect nutritional status and oral health.
Physiology of the Gastrointestinal Tract
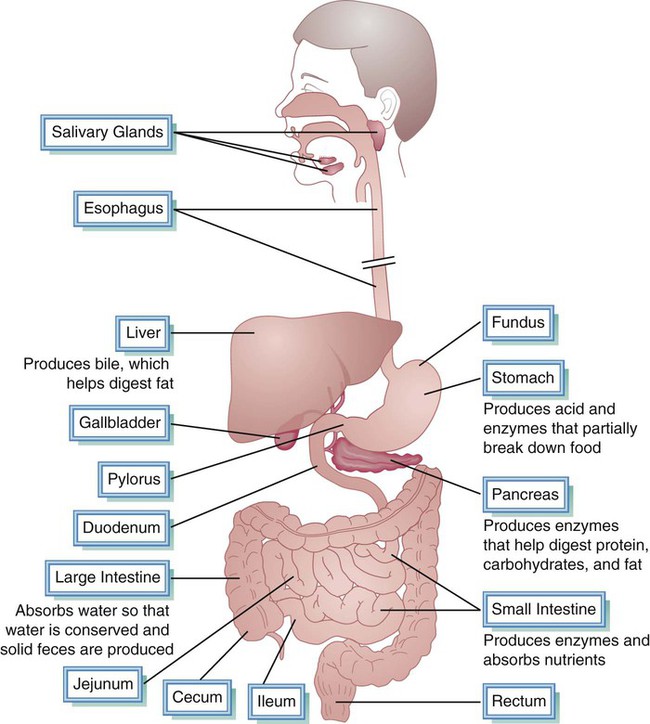
The digestive system includes the alimentary canal and several accessory organs (Fig. 3-1). The alimentary canal is a tubular structure approximately 30 feet long (five times the height of an average man). The alimentary canal, extending from the mouth to the anus, comprises all the body parts through which food passes. It includes the oral cavity, pharynx, esophagus, stomach, small intestine, and large intestine. The small intestine is comprised of the duodenum, jejunum, and ileum; the large intestine includes the cecum, colon, and rectum. Accessory organs—the salivary glands, liver, gallbladder, and pancreas—provide secretions essential for digestion and absorption. Digestion involves two basic types of action on food: (a) mechanical and (b) chemical. Mechanical actions include chewing and peristalsis, which break up and mix foods, permitting better blending of foodstuffs with digestive secretions. Chemical actions involve salivary enzymes and digestive juices, reducing foodstuffs to absorbable molecules.
Chemical Action
< ?xml:namespace prefix = "mml" />

Because the enzyme is reused, only small amounts are needed. Enzymes function comparable to keys: they are very specific and function on only one substrate, similar to a key fitting a particular lock, as shown in Chapter 2, Figure 2-10. The name for some enzymes is derived from the name of the substrate, with the suffix -ase (e.g., lactase is the enzyme produced to catalyze the breakdown of lactose).
Mechanical Action
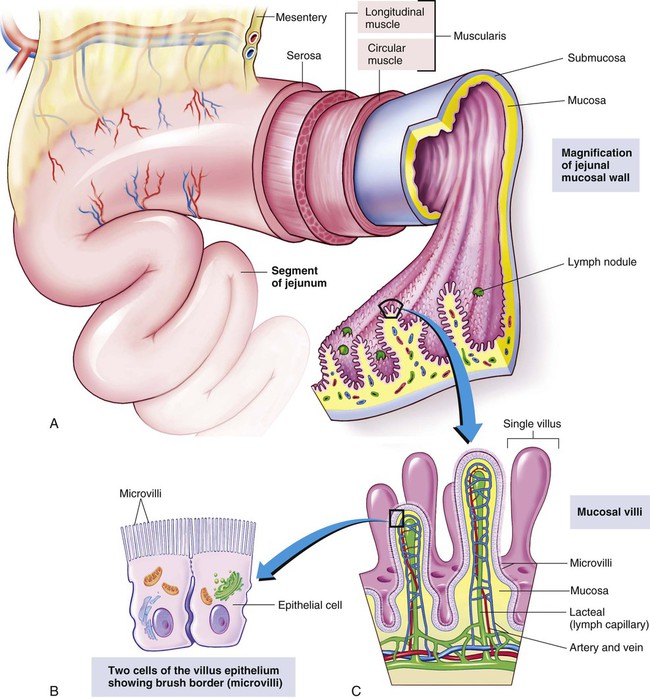
The wall of the gastrointestinal tract is similar from the esophagus to the rectum (Fig. 3-2, A). A layer of muscles encircles the tube, allowing the diameter of the tube to expand and contract. Food particles are broken up and mixed by the churning action. The outer fibers of the muscular coat (longitudinal muscle) run lengthwise and are responsible for peristalsis, involuntary rhythmic waves of contraction traveling the length of the alimentary tract.
Oral Cavity
Taste and Smell
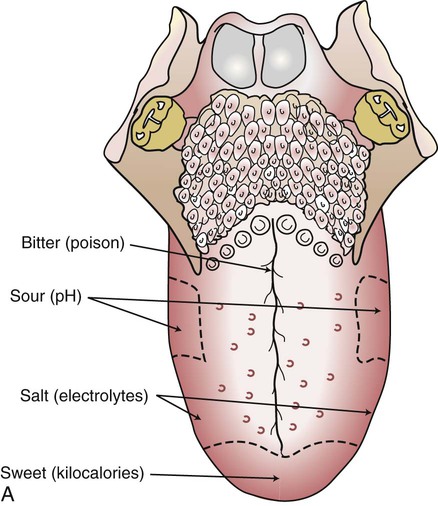
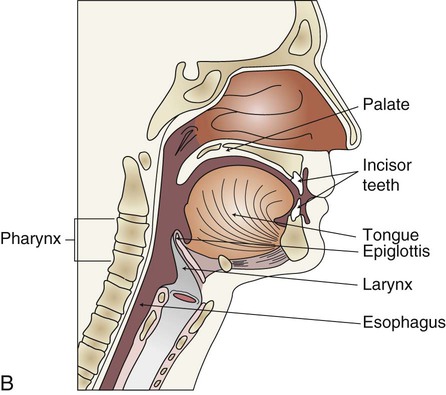
Nerve cells carry messages to the brain, which interprets flavors as sweet, sour, salty, or bitter. These four basic tastes reflect specific constituents of food. Taste buds for all four sensations are located throughout the mouth, but specific kinds of buds are concentrated in certain (but overlapping) areas. Taste buds also are found on the soft palate, epiglottis, larynx, and posterior wall of the pharynx (Fig. 3-3). Taste and smell are essential for maintaining sufficient intake to meet physiological needs.
Loss of smell, or anosmia, results in limited capacity to detect flavor of food and beverages. Ability to smell food being prepared and eaten influences food selection. Smell is also a protective mechanism; odors are used to help determine whether foods are harmful or spoiled. Upper respiratory infections, nasal or sinus problems, neurological disorders, endocrine abnormalities, aging, or head trauma may cause anosmia. A common cold often impairs a person’s sense of smell, causing loss of appetite and limiting the ability to “taste” and enjoy food. The rate of the continuous renewal process undergone by olfactory receptor cells is depressed in malnutrition and by some antibiotics. Some of these disorders are self-limited; however, chemosensory losses from chemotherapy, upper respiratory infection, and aging may be irreversible.1,2
Dysgeusia is persistent, abnormal distortion of taste, including sweet, sour, bitter, salty, or metallic tastes. Dysgeusia without identifiable taste stimuli is called phantom taste. Dysgeusia may be caused by a previous viral upper respiratory infection, head trauma, a neurological or psychiatric disorder, a systemic condition (a disease or disorder that affects the whole body), xerostomia (dry mouth from inadequate salivary secretion), a severe nutritional deficiency, an invasive dental procedure resulting in nerve damage, an oral bacterial or fungal infection, or burning mouth syndrome,3 or it may have an iatrogenic causation. Iatrogenic refers to an adverse condition resulting from medical treatment, e.g., medications, irradiation, surgery. These conditions may also cause hypogeusia or loss of taste, and hypergeusia or heightened taste acuity. Dysgeusia may also result from breathing through the mouth. The dental hygienist is frequently the first healthcare provider to detect a patient’s taste disorder. Hyperkeratinization of the epithelium causing blockage of taste buds and affecting dietary intake may be observed during an oral examination.
Saliva
Saliva is supersaturated with calcium phosphates that allow demineralized areas of hydroxyapatite in enamel to be remineralized. Demineralization occurs when calcium, phosphate, and other minerals are lost from tooth enamel, causing tooth enamel to dissolve. This occurs because of acids produced by fermentable carbohydrates combining with acidogenic bacteria (see Chapter 18); it is not caused by insufficient calcium. Genetic variations of saliva, especially amylase, affect food preferences and intake by influencing oral sensory properties of food.4
Acidic, sour, or bitter tastes stimulate salivary flow. Saliva production is also stimulated by consumption of tasty foods and gum chewing. An increase in oral clearance rate decreases risk of caries formation (for more information, see Chapter 18). Saliva blends with food particles to moisten foods so they are more easily manipulated and prepared for swallowing.
Some chemical action or hydrolysis of nutrients begins in the mouth. Table 3-1 shows the functions of the different constituents in saliva. Because food is normally in the mouth briefly, ptyalin, or salivary amylase, initiates starch digestion. If a carbohydrate food, such as a cracker, is chewed and held in the mouth for a few seconds, it will begin to taste sweet, indicating that some starch is being hydrolyzed to dextrin and maltose.
Table 3-1
| Saliva Component | Classification | Function |
| Mucin | Glycoprotein | Lubricates food for easier passage and protects the lining of the gastrointestinal tract |
| Ptyalin (amylase) | Enzyme | Initiates hydrolysis of complex carbohydrates to simple sugars |
| Lysozyme (antibody) | Enzyme | Breaks down cell walls of some ingested bacteria |
Dry mouth from inadequate salivary flow, also called xerostomia, leads to diminished gustatory function (see Chapter 20 for additional details). Xerostomia may result in frequent oral ulcerations, increased sensitivity of the tongue to spices and flavors, and increased risk of dental caries. Many drugs, including diuretics, cause xerostomia. Diuretics, prescribed to help the body eliminate fluids, also cause a decrease in salivary flow. Increasing fluid intake to 8 to 10 cups daily is important to compensate for these losses.
Teeth
Teeth play a major role in digestion by crushing and grinding food into smaller pieces, a process known as mastication. In contrast to bone, neither tooth enamel nor dentin can be repaired or replaced in significant amounts by any natural process. Only small amounts of enamel and dentin are repaired or replaced through enamel remineralization and through secondary dentin deposition around the pulp chamber of the tooth (Fig. 3-4). Mineral deposition and resorption affect the bone that supports the dentition. This supporting bone, known as alveolar bone, is primarily trabecular bone (bony spikes forming a meshwork of spaces) and cancellous bone (bone within the spaces created by the network of trabecular bone, which appears spongy and contains bone marrow in small hollows). Negative calcium balance increases susceptibility to resorption and bone loss in the alveolar process
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


