The technologic advances in temporomandibular joint arthroscopy and arthrocentesis have given oral surgeons a treatment for patients who have not responded to conservative and pharmacologic treatment without the surgical risks and long-term recovery of open joint surgery.
The technological advances in temporomandibular arthroscopy and arthrocentesis have given oral surgeons a treatment for patients who have not responded to conservative and pharmacologic treatment without the surgical risks and long-term recovery of open joint surgery.
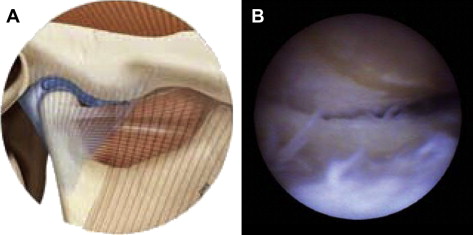
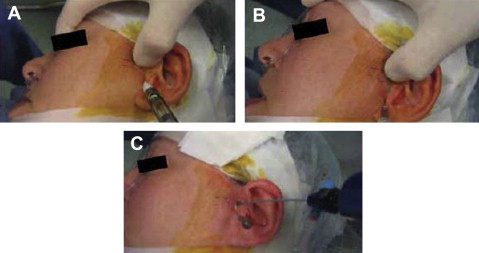
The development of a less-invasive surgical treatment of temporomandibular joint (TMJ) pathology began in 1975 when Ohnishi first used an arthoscope to enter and study the TMJ. The major surgical procedures that would follow to be used with the arthroscope were diagnostic, by attaching the arthroscope to a screen to visualize the joint and the lysis and lavage of the joint ( Fig. 1 ). This procedure most commonly involves the placement of two arthroscopic portals, one of which is for the arthroscope and the other for a blunt probe. As the joint is observed and the adhesions are encountered, the probe can be used in a sweeping fashion to break up the adhesion. The use of the probe along with the hydraulic distention of the joint allow for stretching of the joint space. Images of preparation for and performing the procedure can be seen in Fig. 2 . When the adhesions are broken down and the joint space distended, the joint movement improves and range of motion increases. Drugs, such as corticosteroids and sodium hyaluronate, have also been injected following the joint to reduce inflammation and improve lubrication, respectively. By 1991, Nitzan and colleagues showed that performing lavage of the TMJ without the scope, a procedure called arthrocentesis, gave similar results in the reduction of pain with success rates in up to 91% of patients. Arthrocentesis involves placement of two cannulas into the superior joint for hydraulic distension and joint lavage. The initial application of the procedure was for the treatment of internal derangement of the TMJ. Later stages in this disorder can eventually lead to anterior disc displacement without reduction, also called closed lock because of the limited mobility of the jaw. This disorder is often accompanied by pain but the exact mechanism seems multifaceted. With the procedure’s success in reducing pain and increasing mobility, arthrocentesis was expanded for treatment in other joint disorders. Recent comparisons between arthroscopy and arthrocentesis have shown both procedures to be successful (82% to 75%, respectively) with no significant difference in their success rates. Some investigators have argued that patients with chronic long-standing closed lock are more resistant to arthrocentesis and require TMJ arthroscopic lysis and lavage.
There have been many theories as to the etiology of TMJ dysfunction and of how it results in pain. The focus of TMJ research at one time was on the shape and anatomic position of the deranged disc but the focus has changed to the biochemical environment and inflammatory mediators related to the pathologic joint. One theory for the success of arthrocentesis comes from the active elimination of the altered synovial fluid, which, together with physiotherapy, produces improved joint function with a diminished pain sensation. Despite many studies showing that disc position and perforations do not improve with arthrocentesis, many patients have experienced improved TMJ function with less pain from this procedure.
Before arthroscopic surgery or arthrocentesis is performed, conservative management must be attempted to see if symptoms can be relieved with out surgery. Literature has shown that nonsurgical management, which includes physical therapy, behavioral changes, and pharmaceuticals for internal derangement, can improve a patient’s symptoms without the need for surgical treatment from 74% to 85% of the time. Those who do not respond to conservative treatment may still benefit from arthrocentesis and/or arthroscopic lysis and lavage. Kim and colleagues conducted a study investigating closed lock patients who had not shown response to the conservative treatment for more than 3 months. TMJ lysis and lavage were performed using an ultrathin arthroscopy, and positive outcomes were found in 80% of patients.
The other major indications for arthrocentesis are
- 1.
Acute and chronic limitation of opening because of anteriorly displaced disc without reduction
- 2.
Chronic pain with good range of motion and anterior disc displacement with reduction
- 3.
Degenerative osteoarthritis
- 4.
A condition of TMJ open lock where the condyle is entrapped anterior to the condyle.
Contraindications to TMJ arthrocentesis are patients who have undergone successful conservative treatment, demonstrate bony or fibrous ankylosis, or have extracapsular sources of pain.
Arthrocentesis of the TMJ may be performed with the patient receiving a local anesthetic, intravenous conscious sedation, or general anesthetic depending on surgeon and patient preference.
As TMJ arthroscopy and arthrocentesis have gained popularity, new techniques, entry portals, and technology have been developed to enhance the classic arthroscopic procedure of the TMJ.
Moses highlighted the general principles that all arthroscopy techniques must include the following:
- 1.
The joint should be fully distended allowing easier trocar puncture and minimizing the risk of iatrogenic intracapsular damage.
- 2.
The skin should be punctured with a sharp trocar.
- 3.
All intracapsular procedures should be done with care to prevent articular surface damage.
- 4.
Attention should be given to preserve as much healthy synovium as possible to enhance its physiologic effects on the joint.
- 5.
The joint space should be kept expanded during instrumentation by a slow infusion irrigation system.
Over the past two decades the popularity of arthroscopy and arthrocentesis has grown because it has been considered a safe and effective procedure for TMJ pain with a low complication rate. Tsuyama and colleagues first reported a 10.3% complication rate after arthroscopic procedures but a larger and more recent study showed a complication of only 1.3%, demonstrating the success of the new techniques and surgeons’ increased experience with arthroscopy. The major portion of complications was otologic problems, including blood clots in the external auditory meatus, perforation of the tympanic membrane, partial hearing loss, ear fullness, and vertigo. Other injuries included neurologic injury to fifth and seventh cranial nerves and TMJ injury possibly causing osteoarthritis. Correct portal placement lowers the chances of complications and decreases the chances of limited access within the TMJ during the arthroscopic technique. McCain and de la Rua are given credit for combining anatomic knowledge with a surgical perspective, giving detailed, precise anatomic measurements for portal placement. Due to the anatomic variations from one patient to another, the portals are anatomically measured, then palpated for confirmation before cannulization is started.
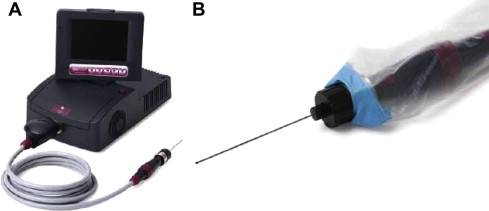
Some of the major contributions to TMJ arthroscopy have come from the technological advances in arthroscopes. The improvements in camera and lens technology have advanced the ability to diagnose a wide variety of pathologic conditions within the TMJ. The Onpoint 1.2 mm Scope System is an innovative breakthrough that provides minimally invasive visualization of the joint in the convenience of an office-based setting ( Fig. 3 ). The button on the hand piece allows still image and video recording for the visual effect of patient instruction, and visualization and smaller size could prevent complications. The disposable fiberoptic scope tube is approximately the size of an 18-gauge needle and is sterile packaged for single use. The Onpoint system is a single-portal system, thereby requiring only one puncture of the joint, and the new fiberoptic design tolerates more flexion to help avoid tissue trauma.