Hemifacial microsomia (HFM; Online Mendelian Inheritance in Man [OMIM] 164210) is the most common congenital craniofacial anomaly after cleft lip or palate (or both) and occurs in 1 in every 4000 to 5600 children. This congenital condition involves the structures of the first and second branchial arches, with variable clinical dysplasia of both skeletal and soft tissues. The five major craniofacial components of HFM include the ear (most consistent finding), mandible (most commonly involved skeletal structure), orbit, cranial nerve VII, and facial soft tissues (including the masticatory muscles) on the affected side. HFM is frequently unilateral; however, bilateral involvement may also occur.
Etiology/Pathology
The etiology and pathogenesis of HFM are unknown, although it is presumed that there is interference with neural crest cell migration during embryologic development. The condition is believed to be sporadic, but examples of familial transmission have been documented.
Classification
Many classification systems have been used to describe the varying degrees of deformity associated with HFM. These systems often use the mandible as the cornerstone of the classification since it is frequently affected and treatment of the mandible is typically inevitable. One of the most commonly used classification systems is the modification of the Pruzansky classification described by Kaban and colleagues. It is based on discrete findings of the presence or absence of critical elements of the mandible, particularly the condyle-ramus-glenoid fossa unit, and it consists of, in order of severity, types I, IIa, IIb, and III ( Fig. 94-1 ). This classification has been instrumental in directing appropriate surgical corrections to achieve mandibular symmetry.


The OMENS classification is also commonly used and is more comprehensive. It includes the five affected facial components of HFM: orbit, mandible, ear, nerve, and soft tissue. Each of the five components is graded 0 to 3 based on the degree of abnormality, with 0 indicating no abnormality and 3 indicating absence or severe deficiency of the structure. This classification system is particularly useful in categorizing the phenotypic variations seen in patients with HFM ( Fig. 94-2 ).

In general, the muscular hypoplasia correlates with the degree of bone deficiency. If the coronoid process is missing, the temporalis muscle demonstrates severe hypoplasia and abnormal muscle recruitment; the same relationship holds true between the masseter muscle and the gonial angle. Additionally, the higher the OMENS score, the more likely extra-craniofacial abnormalities are present, including abnormalities of the cardiac, vertebral, central nervous, renal, and pulmonary organ systems. There are developmental correlations between the severity of the mandibular hypoplasia and the other facial anomalies; however, the correlations are weak because of an extremely diverse phenotypic spectrum.
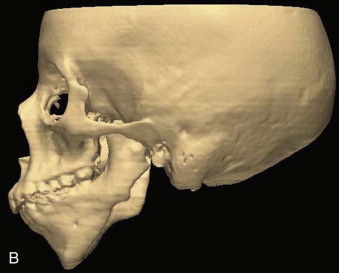
In all patients with HFM, the unilateral impairment in growth causes deviation of the mandibular skeletal midline toward the affected side. Because the mandible is short, retrusive, and narrow on the affected side, downward growth of the maxilla is restricted and a secondary deformity occurs. This results in a vertically short maxilla and an occlusal plane that tilts upward on the affected side.
Classification
Many classification systems have been used to describe the varying degrees of deformity associated with HFM. These systems often use the mandible as the cornerstone of the classification since it is frequently affected and treatment of the mandible is typically inevitable. One of the most commonly used classification systems is the modification of the Pruzansky classification described by Kaban and colleagues. It is based on discrete findings of the presence or absence of critical elements of the mandible, particularly the condyle-ramus-glenoid fossa unit, and it consists of, in order of severity, types I, IIa, IIb, and III ( Fig. 94-1 ). This classification has been instrumental in directing appropriate surgical corrections to achieve mandibular symmetry.


The OMENS classification is also commonly used and is more comprehensive. It includes the five affected facial components of HFM: orbit, mandible, ear, nerve, and soft tissue. Each of the five components is graded 0 to 3 based on the degree of abnormality, with 0 indicating no abnormality and 3 indicating absence or severe deficiency of the structure. This classification system is particularly useful in categorizing the phenotypic variations seen in patients with HFM ( Fig. 94-2 ).

In general, the muscular hypoplasia correlates with the degree of bone deficiency. If the coronoid process is missing, the temporalis muscle demonstrates severe hypoplasia and abnormal muscle recruitment; the same relationship holds true between the masseter muscle and the gonial angle. Additionally, the higher the OMENS score, the more likely extra-craniofacial abnormalities are present, including abnormalities of the cardiac, vertebral, central nervous, renal, and pulmonary organ systems. There are developmental correlations between the severity of the mandibular hypoplasia and the other facial anomalies; however, the correlations are weak because of an extremely diverse phenotypic spectrum.
In all patients with HFM, the unilateral impairment in growth causes deviation of the mandibular skeletal midline toward the affected side. Because the mandible is short, retrusive, and narrow on the affected side, downward growth of the maxilla is restricted and a secondary deformity occurs. This results in a vertically short maxilla and an occlusal plane that tilts upward on the affected side.
Treatment
Multidisciplinary treatment is required for an ideal outcome. The maxillomandibular complex is often the focus of treatment, with the severity of mandibular deformity dictating the appropriate treatment. The role of the oral and maxillofacial surgeon is critical in establishing the ideal and most stable skeletal foundation that can support the soft tissue augmentation and ear construction. For the purpose of this chapter, we will focus on current therapies related to the skeletal abnormalities associated with HFM and briefly describe therapies to correct the ear and soft tissue abnormalities.
Sequence and Controversies
The main considerations in the surgical management of patients with HFM are timing and the anatomic extent of construction. The ear is typically constructed around the age of 6 years, followed by surgery on the external auditory canal if needed; the maxillomandibular deformities may be addressed while the patient is growing or when skeletal maturation has occurred; and the soft tissue augmentation is performed 6 to 8 months after maxillomandibular correction. The differences in surgical strategy and timing result from inconclusive evidence regarding the progression of mandibular asymmetry in patients with HFM. It is unclear whether there is sustained growth on the affected side that continues at the same rate as on the unaffected side with stable facial asymmetry (constant asymmetry) or whether there is progressive worsening of the facial asymmetry because of the lag in growth of the affected side (progressive asymmetry).
Interestingly, proponents of both the constant versus progressive nature of the mandibular asymmetry have used the same two radiographic studies that monitored longitudinal facial growth in patients with HFM as support for their theory. In radiographic studies by Rune and associates and Polley and co-workers, it was originally concluded that the degree of mandibular asymmetry remains relatively constant throughout craniofacial development, and this was corroborated by clinical observations. Based on this theory, correction of the facial deformity is performed after the patient has completed growth, as is the case for most orthognathic corrections.
The other possibility is that the affected side lags behind the unaffected side and the patient demonstrates progressive facial asymmetry over time. Re-interpretation of the data by Rune and colleagues and Polley and co-workers, however, has also been used to support the concept that the mandibular asymmetry is progressive, as reflected by worsening of vertical mandibular skeletal asymmetry and mandibular ramus height ratios. In addition, the degree of progressive asymmetry has been shown to correlate with the severity of mandibular deformity. Follow-up of a cohort of children after costochondral graft reconstruction also demonstrated that diminished growth of the constructed ramus and condyle (similar to the undergrowth on the untreated affected side) resulted in progressive facial asymmetry with worsening occlusal, piriform, and intergonial canting. Proponents of the second theory favor early treatment of patients with HFM, while they are still growing, to improve facial and mandibular growth, reduce secondary deformities in the maxilla, and enhance the development of a positive body image.
Management of the MaxilloMandibular Complex
The hallmark of HFM is facial asymmetry as a result of asymmetric development of the mandible. Treatment of these patients can be grouped into two categories based on the Kaban-Pruzansky classification: types I and IIa are typically treated similarly, and types IIb and III are treated similarly. The timing of treatment is dependent on when the patient and family initiate treatment and whether early or delayed surgical intervention is recommended by the treating craniofacial team or surgeon. Particular goals of treatment are to (1) increase the size of the malformed and underdeveloped mandible and soft tissues, (2) create an articulation between the mandible and the temporal bone, (3) correct the secondary deformities of the maxilla, and (4) establish functional occlusion and optimal facial symmetry. When treatment is initiated before completion of craniofacial growth, these goals are accomplished by adhering to the following treatment phases: presurgical orthodontic-orthopedic treatment, mandibular surgery, postsurgical bone induction and secondary correction of the maxillary deformity, final orthodontic treatment, and soft tissue augmentation.
Treatment Planning
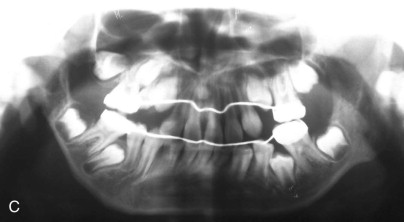
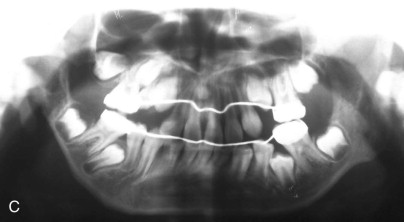
The combined orthodontic-orthopedic and surgical treatment decisions are based on the patient’s clinical findings and craniofacial imaging. Previously, plain films, including a Panorex, posteroanterior cephalogram, and lateral cephalogram, were used to determine the mandibular classification and provide a treatment plan. Currently, computed tomography (CT) with three-dimensional (3D) reconstruction is being used to clearly delineate the asymmetry in patients with HFM because this condition has an impact on the craniofacial skeleton in all three dimensions. These images demonstrate not only the asymmetry of the facial bones but also the extent of cranial base asymmetries and soft tissue deficiencies ( Fig. 94-3 ). Composite 3D models of a patient with HFM can be fabricated; however, 3D surgical treatment planning can also be performed with available software, and the 3D models may not be necessary.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


