Sleep bruxism (SB) is a common sleep-related motor disorder characterized by tooth grinding and clenching. SB diagnosis is made on history of tooth grinding and confirmed by polysomnographic recording of electromyographic (EMG) episodes in the masseter and temporalis muscles. The typical EMG activity pattern in patients with SB is known as rhythmic masticatory muscle activity (RMMA). The authors observed that most RMMA episodes occur in association with sleep arousal and are preceded by physiologic activation of the central nervous and sympathetic cardiac systems. This article provides a comprehensive review of the cause, pathophysiology, assessment, and management of SB.
Definition and classification of sleep bruxism
In dentistry, bruxism is traditionally considered an oral parafunction characterized by involuntary grinding and clenching of the teeth. Although this definition describes the main characteristics of the disorder, it lacks a substantial and important distinction between the wake and sleep states in which this oral parafunction may occur. In fact, a wake-time habit of clenching, grinding, or gnashing the teeth seems to be a different nosologic entity, probably with a different cause and pathophysiology, and it should be distinguished from bruxism during sleep.
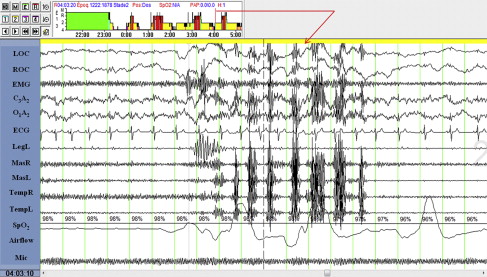
According to the American Academy of Sleep Medicine (AASM) ( International Classification of Sleep Disorders, Second Edition [ICSD-II]), sleep bruxism (SB) is classified as a sleep-related movement disorder. The characteristic electromyography (EMG) pattern of SB is found in repetitive and recurrent episodes of rhythmic masticatory muscle activity (RMMA) of the masseter and temporalis muscles that are usually associated with sleep arousals. RMMA shows a frequency of 1 Hz and typically occurs cyclically during sleep ( Fig. 1 ). RMMA episodes are observed in 60% of the general adult population as physiologic activity of the jaw muscles during sleep. Many other forms of masticatory and facial muscle activity are also observed during sleep, such as swallowing, coughing, sleep talking, smiling, lip sucking, jaw movements, and myoclonus. These orofacial activities account for approximately 85% of EMG events scored on the masseter and temporalis muscles in control subjects and 30% in patients with SB. In fact, RMMA frequency is 3 times higher in patients with SB than in controls and is typically associated with tooth-grinding sounds (in 45% of cases), as reported by patients, bed partners, parents, or siblings.
SB may be an extreme manifestation of a physiologic orofacial motor behavior during sleep (RMMA and chewinglike activity) whereby certain factors increase its occurrence until it falls into the pathologic range of jaw-muscle activity. Therefore, SB refers to the sleep motor disorder, whereas RMMA is the characteristic EMG pattern that is scored during sleep to make a polysomnographic diagnosis of SB.
Assessment and diagnosis of SB
The assessment and diagnosis of SB are often challenging. Generally, the assessment is based on reports of tooth-grinding sounds during sleep and the presence of clinical signs and symptoms. However, only an EMG recording of the masticatory muscles can confirm the SB diagnosis. Several portable diagnostic tools have been developed to record masseter or temporalis EMG activity during sleep to avoid using the more sophisticated but highly cost- and time-consuming polysomnography (PSG). However, the reliability of most portable devices has not yet been validated, and their use may be considered only as support in a clinical assessment of SB. In fact, the SB diagnosis is usually clinical, although the gold standard remains a full-night PSG with audio-video recording ( Table 1 ). The future direction for SB assessment would be to develop a handy tool that can directly, reliably, and rapidly measure ongoing bruxism activity and that can be used in both clinical (for diagnosis, treatment outcome evaluation, and follow-up) and research settings.
| Method | Notes |
|---|---|
| Patient history | Many patients may not be aware of their tooth-grinding habit during sleep. It is more reliable if the bed partner, parents, or siblings report current tooth-grinding sounds during sleep |
| Clinical assessment | It is used to assess the clinical signs and symptoms that suggest SB (eg, tooth wear; see Box 1 ) and the presence of potential risk factors for other comorbidities (eg, enlarged tonsils, skeletal class II, and Mallampati score III or IV for the risk of concomitant SDB) |
| Questionnaires | It is used to investigate patients’ general and oral health, sleep quality, sleep habits, oral parafunctions, presence and characteristics of pain, headache, fatigue, depression, anxiety and stress, and comorbidities. |
| Ambulatory EMG monitoring | It allows recording EMG activity during sleep from the temporalis or masseter muscles, depending on the device used. However, there is very low specificity and sensitivity in distinguishing actual RMMA episodes from the many other orofacial and motor activities that occur during sleep. Furthermore, there is no monitoring on awakening from sleep, arousal, sleep staging, or other sleep variables. This tool could be valuable in the clinical assessment of SB and in large-sample studies (eg, general population epidemiologic studies) |
| Ambulatory PSG recording (type II, III, and IV) | It is usually performed at patients’ homes. Normally, there is no audio-video monitoring; specificity and sensitivity in detecting RMMA depends on the device used, and more particularly, on the number of variables monitored (EEG, EOG, ECG, EMG, and respiratory channels). This method may be used for scoring sleep stages, sleep arousals, leg movements, and EMG activity, and for monitoring breathing |
| Full audio-video PSG recording (type I) | It remains the gold standard for the diagnosis of SB and the assessment of comorbidity with other sleep disorders (eg, SDB, PLMS, RLS, RBD, parasomnias). Normally, it allows full-night monitoring of EEG, EOG, EMG, ECG, leg movements, respiratory effort, airflow, and oxygen saturation. Concomitant audio-video recording increases the specificity and sensitivity in RMMA detection and scoring by distinguishing between RMMA episodes and orofacial (eg, swallowing, coughing, sleep talking) and other muscular activities (eg, head movements, eye blinking) that occur during sleep |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


