Introduction
The purpose of this prospective study was to evaluate the dentoskeletal effects of a new magnetic functional appliance, the Sydney Magnoglide (Macono Orthodontic Lab, Sydney, Australia), after both active treatment with the appliance and comprehensive fixed appliance therapy, compared with a group of untreated Class II controls.
Methods
Thirty-four consecutively treated Class II Division 1 patients treated with the Sydney Magnoglide followed by fixed appliances were compared with 30 untreated Class II controls with the same initial dentoskeletal Class II features and matched for age and sex. Lateral cephalograms were taken before treatment, immediately after functional appliance therapy, and after comprehensive fixed appliance therapy. Cephalometric analyses included the Pancherz analysis and linear and angular measurements. The comparisons were made with Student t tests ( P <0.05). There were 3 dropouts, for a final sample for statistical analysis of 31 subjects.
Results
There was no statistically significant difference between the treated and control groups before treatment. Treatment with the Sydney Magnoglide and comprehensive fixed appliance therapy normalized the overjet and corrected the Class II relationship in all treated subjects. The ANB angle showed a reduction of 1.0°, as opposed to an increase of 0.3° in the untreated controls, and was associated with a statically significant improvement in the SNB angle ( P <0.05). There was a significant gain of 2.3 mm in mandibular length in the treated group compared with the control group ( P <0.01).
Conclusions
The outcomes of this prospective study demonstrate that the compliance-free Sydney Magnoglide is an effective functional appliance for Class II correction.
Class II malocclusion is a common orthodontic problem, occurring in about one third of the population. A variety of skeletal and dental configurations arise in combination with a Class II relationship, with mandibular skeletal retrusion the most consistent finding. Therefore, functional appliance therapy, which aims to stimulate mandibular growth by forward posturing of the mandible, has been a popular approach for Class II treatment.
Many functional appliances have been developed for this purpose. Functional appliances can be classified as fixed, such as the Herbst, and removable, such as the Twin-block and activator. A recent systematic review found that the Herbst appliance had the highest efficiency for enhancing mandibular growth, followed by the Twin-block. However, there are shortcomings associated with both of these appliances. A multicenter, randomized clinical trial reported a 33% failure-to-complete rate for the Twin-block, indicating that compliance is an issue, and a high rate of breakages with the Herbst appliance, necessitating more appointments for repairs.
A new magnetic functional appliance has been developed to address these shortcomings. The Sydney Magnoglide (Macono Orthodontic Lab, Sydney, Australia) is a fixed functional appliance consisting of maxillary and mandibular right and left bonded acrylic resin blocks. Each block has embedded magnets arranged in a manner that postures the mandible into a Class I occlusion. Bonding the appliance addresses the issue of compliance, and the lack of moving parts reduces the likelihood of breakage and improves patient comfort.
Magnetic forces have been used in orthodontics for both tooth movement and orthopedic correction with varying degrees of success. The magnets initially used were bulky, and there were concerns about possible toxic effects. Improved safety with better coatings and the introduction of rare earth magnets, which led to a dramatic reduction in magnet size, stimulated further interest in orthodontic applications. The advantages of magnets over traditional force-delivery systems include no friction, no material fatigue, the ability to produce predictable force levels over long periods of time, and no need for direct contact.
Various magnetic functional appliances have been introduced in the literature. With such appliances, the mandible is held in a forward position with the help of magnetic forces. Darendeliler and Joho introduced the magnetic activator device II for this purpose and demonstrated successful correction of Class II malocclusion with the appliance. The design of the appliance has evolved to improve efficiency and patient compliance, and reduce bulk. This resulted in the new magnetic functional appliance used in this study, the Sydney Magnoglide.
Treatment timing has also been acknowledged as a critical factor for success in Class II correction, and it is now generally accepted that treatment should be undertaken during the peak of mandibular growth. The rate, onset, duration, and intensity of the pubertal spurt in mandibular growth varies for each patient. Thus, optimal timing of dentofacial orthopedics is intimately linked to the identification of periods of accelerated growth. Numerous maturational indexes have been suggested to evaluate skeletal maturity in growing patients. Among these, the cervical vertebral maturation method (CVM) has been validated as a biologic indicator of mandibular and somatic skeletal maturity. The growth interval between CVM stages 3 and 4 has been shown to coincide with the pubertal peak in mandibular growth and is advocated as the optimal time for Class II treatment.
The purpose of this prospective study was to evaluate the dentoskeletal effects of a new magnetic functional appliance, the Sydney Magnoglide, after both active treatment with the appliance and comprehensive fixed appliance therapy, compared with a group of untreated Class II controls. Both treated and control subjects were evaluated with reference to the CVM method because of the impact of timing on treatment outcomes. The breakage rate and the complications with the Sydney Magnoglide appliance were also evaluated.
Material and methods
This prospective clinical study was based on the records of 34 consecutively treated patients from the private practice of the third author (R.H.). The sample comprised 20 boys and 14 girls. The criteria for enrollment in the study were (1) Class II Division 1 malocclusion of a half or full cusp, (2) overjet of 6 mm or greater, (3) ANB angle greater than 3.5°, and (4) a nonextraction treatment plan.
Of the original sample, 2 patients moved during their treatments, and 1 terminated treatment early because of poor oral hygiene. These 3 dropouts led to a final sample for statistical analysis of 31 subjects.
Lateral cephalograms were taken before treatment (T1), immediately after functional appliance therapy (T2), and after comprehensive fixed appliance therapy (T3). Clinical photographs and study models were obtained for all subjects at the start and conclusion of treatment. The time between T1 and T2 was approximately 1.0 year (SD, 0.4 year). Fixed appliance therapy immediately followed the functional jaw orthopedics (T3-T2), with a mean duration of 1.0 year (SD, 0.4 year). As shown in Table I , the mean age of the patients at T1 was 13.5 years (SD, 1.2 years). The mean age at T2 was 14.5 years (SD, 1.1 years), and the mean age at T3 was 15.4 years (SD, 1.2 years).
| At T1 | Magnoglide group Class II subjects (n = 31) | Control group untreated Class II subjects (n = 30) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (y) | 13.5 | 1.2 | 13.0 | 1.6 |
| Subjects (n) | % | Subjects (n) | % | |
|---|---|---|---|---|
| CS 1 | 0 | 0 | 0 | 0 |
| CS 2 | 4 | 12.9 | 2 | 6.7 |
| CS 3 | 8 | 25.8 | 13 | 43.3 |
| CS 4 | 16 | 51.6 | 14 | 46.7 |
| CS 5 | 3 | 9.7 | 1 | 3.3 |
| CS 6 | 0 | 0 | 0 | 6 |
| At T2 | Mean | SD | Mean | SD |
|---|---|---|---|---|
| Age (y) | 14.5 | 1.1 | 14.3 | 1.2 |
| Subjects (n) | % | Subjects (n) | % | |
|---|---|---|---|---|
| CS 1 | 0 | 0 | 0 | 0 |
| CS 2 | 0 | 0 | 0 | 0 |
| CS 3 | 0 | 0 | 0 | 0 |
| CS 4 | 20 | 64.5 | 13 | 43.3 |
| CS 5 | 10 | 32.3 | 14 | 46.7 |
| CS 6 | 1 | 3.2 | 3 | 10 |
| At T3 | Mean | SD | Mean | SD |
|---|---|---|---|---|
| Age (y) | 15.4 | 1.2 | 15.3 | 1.3 |
| Subjects (n) | % | Subjects (n) | % | |
|---|---|---|---|---|
| CS 1 | 0 | 0 | 0 | 0 |
| CS 2 | 0 | 0 | 0 | 0 |
| CS 3 | 0 | 0 | 0 | 0 |
| CS 4 | 2 | 6.5 | 0 | 0 |
| CS 5 | 26 | 83.9 | 15 | 50 |
| CS 6 | 3 | 9.6 | 15 | 50 |
| T1-T2 | Mean | SD | Mean | SD |
|---|---|---|---|---|
| Age (y) | 1.0 | 0.4 | 1.1 | 0.8 |
| T2-T3 | Mean | SD | Mean | SD |
|---|---|---|---|---|
| Age (y) | 1.0 | 0.4 | 1.1 | 0.8 |
The treated group was compared with an untreated control group of 30 subjects (15 boys, 15 girls) with the same initial dentoskeletal Class II features as the treated subjects ( Table II ). The control subjects were derived from the University of Michigan Elementary and Secondary School Study and the University of Florence in Italy. The control group was matched as closely as possible to the treatment group for age, sex, and CVM stage. The control group was followed on a parallel basis with the treated subjects. As shown in Table I , the mean age of the controls at T1 was 13.0 years (SD, 1.6 years). The mean age at T2 was 14.5 years (SD, 1.2 years), and the mean age at T3 was 15.4 years (SD, 1.3 years).
| Magnoglide boys (n = 19) T1 | Magnoglide girls (n = 12) T1 | Magnoglide total (n = 31) T1 | Untreated Class II controls (n = 30) T1 | Difference Magnoglide total – controls T1 | Significance | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Cephalometric measurement | ||||||||||
| SNA (°) | 83.1 | 3.3 | 83.0 | 3.6 | 83.0 | 3.3 | 81.8 | 3.5 | 1.2 | NS |
| SNB (°) | 77.9 | 3.6 | 76.8 | 3.3 | 77.5 | 3.5 | 76.6 | 3.4 | 0.9 | NS |
| ANB (°) | 5.2 | 1.6 | 6.2 | 1.3 | 5.6 | 1.5 | 5.5 | 1.3 | 0.1 | NS |
| SN-GoMe (°) | 31.8 | 6.0 | 33.7 | 5.9 | 32.5 | 5.9 | 30.8 | 5.1 | 1.7 | NS |
| Co-Gn (mm) | 117.8 | 5.6 | 109.4 | 5.0 | 114.5 | 6.7 | 113.9 | 4.9 | 0.6 | NS |
| Ar-Gn (mm) | 110.6 | 5.9 | 102.8 | 5.1 | 107.6 | 6.7 | 108.1 | 4.8 | −0.5 | NS |
| Y-axis (°) | 67.1 | 4.5 | 68.0 | 3.8 | 67.5 | 4.2 | 66.7 | 3.8 | 0.8 | NS |
| U1 to SN (°) | 109.6 | 8.2 | 106.1 | 7.2 | 108.2 | 7.9 | 108.2 | 7.1 | 0.0 | NS |
| L1 to GoMe (°) | 98.5 | 4.3 | 96.0 | 12.8 | 97.5 | 8.5 | 98.7 | 6.2 | −1.2 | NS |
| Pancherz analysis | ||||||||||
| Maxillary base (mm) ss | 81.9 | 3.8 | 79.1 | 3.1 | 80.8 | 3.8 | 80.9 | 4.1 | −0.1 | NS |
| Mandibular base (mm) pg | 82.9 | 5.0 | 78.5 | 6.0 | 81.2 | 5.7 | 79.8 | 5.1 | 1.4 | NS |
| Maxillary incisor (mm) is | 91.4 | 4.2 | 87.7 | 4.5 | 90.0 | 4.7 | 92.7 | 4.7 | −2.7 | NS |
| Mandibular incisor (mm) ii | 83.2 | 4.5 | 80.6 | 4.4 | 82.2 | 4.6 | 83.6 | 4.6 | −1.4 | NS |
| Overjet (mm) is/OLp minus ii/OLp | 8.2 | 1.6 | 7.1 | 1.1 | 7.8 | 1.5 | 9.1 | 1.7 | −1.3 | NS |
| Maxillary molar (mm) ms | 57.7 | 4.3 | 55.4 | 3.5 | 56.8 | 4.1 | 55.8 | 4.4 | 1.0 | NS |
| Mandibular molar (mm) mi | 56.6 | 4.9 | 54.1 | 4.2 | 55.6 | 4.7 | 54.9 | 4.7 | 0.7 | NS |
| Molar relation (mm) ms/OLp minus mi/OLp | 1.1 | 1.6 | 1.3 | 1.4 | 1.2 | 1.5 | 0.9 | 1.4 | 0.3 | NS |
The patients were categorized according to their CVM stage as described by Baccetti et al. As shown in Table I , 77.4% of the treated subjects were at CVM stage 3 or 4 at T1, 12.9% were at CVM stage 2, and 9.7% were at CVM stage 5. Ninety percent of the untreated Class II control subjects were at CVM stage 3 or 4 at T1, 6.7% were at CVM stage 2, and 3.3% were at CVM stage 5. Thus, most subjects were between CVM stages 3 and 4 at T1, indicating they were treated or observed during a period of intense mandibular growth rate. At T2 and T3, all subjects in both groups were at a postpubertal stage of skeletal maturation (CVM stages 4-6).
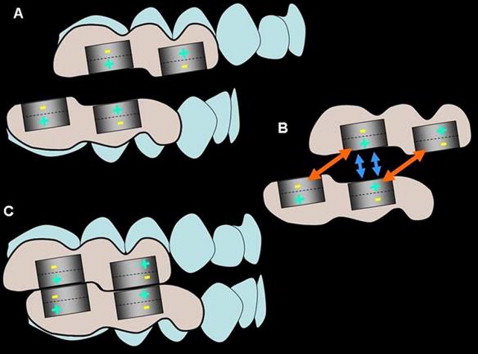
The Sydney Magnoglide is a fixed functional appliance composed of 4 acrylic resin blocks. Two blocks are bonded to the maxillary right and left buccal segments, and 2 to the mandibular right and left buccal segments. Each block contains 2 embedded (7 × 4 × 3 mm) neodymium-iron-boron magnets, arranged to be in attraction with the 2 magnets in the opposing jaw when the casts are positioned in a Class I occlusion through the construction bite registration ( Fig 1 ). The appliance thus postures the mandible forward into a Class I occlusion with the magnets in attraction, while repulsive forces deflect the occlusion away from a retrusive position ( Fig 2 ). A small step in the occlusal surface of the acrylic resin blocks is also designed to mechanically interlock the occlusion in a Class I relationship. This configuration provides both mechanical and magnetic forces to maintain protrusion of the mandible. The magnets are positioned buccally to minimize the vertical dimension of the appliance and improve patient comfort.
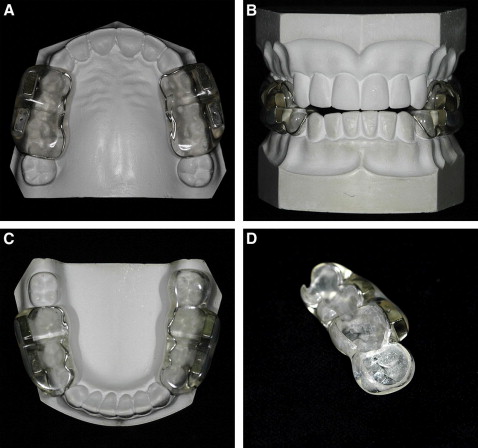
The magnets are encased in nickel and copper, and then coated with a Signum metal bond (Heraeus, Hanau, Germany) to improve the retention with the acrylic resin. The blocks also include a cobalt-chromium alloy framework, which is essential to facilitate removal of the blocks in a single piece when treatment is completed. The internal surface of the blocks is sandblasted to improve the interlocking with the bonding cement. The appliance is cemented by using glass ionomer cement after the enamel surface is cleaned and polished ( Fig 1 ).
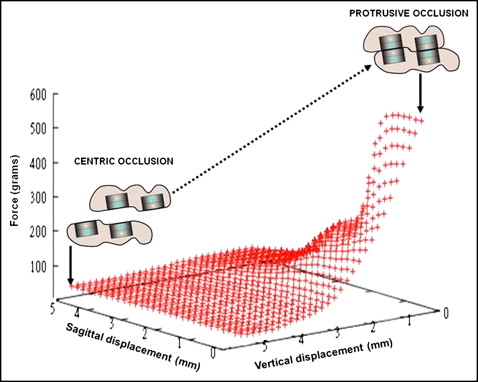
The robotic-measurement system was used to measure the force-displacement characteristics of the Sydney Magnoglide by simulating mandibular jaw movements vertically, transversally, and sagitally ± 5 mm. The robotic-measurement system consists of a precision industrial robot (RX 60; Stäubli, Bayreuth, Germany) with 6 degrees of freedom and a 3-dimensional force-moment sensor (FTS nano 12-0.12; Schunk, Lauffen/Neckar, Germany). The starting position (x = y = z = 0) corresponds to the constructed protruded position with a vertical separation of 0.5 mm. Figure 3 depicts a 3-dimensional force displacement curve of the Sydney Magnoglide with changes in vertical and sagittal displacements. Because of the overall thickness of the acrylic resin coating (0.5-0.6 mm), the intermagnet distance, produced by a gap between the magnets of 1 to 1.5 mm, reduced the force magnitude to 325 to 442 g on each side.
The magnetic appliances were cemented for 7 to 8 months, and no other fixed appliance treatment was rendered during the functional appliance stage. One week after the removal of the functional appliance, all patients underwent nonextraction fixed appliance therapy with a straight-wire appliance. Three bracket systems were used: SPEED (Strite Industries, Cambridge, Ontario, Canada), Inspire Ice (Ormco, Orange, Calif), and In-Ovation (GAC, Bohemia, NY). Class II elastics (.25 in, 3.5 oz) were worn during fixed appliance therapy for an average of 17 weeks (SD, 16 weeks). The average treatment time with fixed appliances was 1.0 year (SD, 0.4 year).
Radiographs were traced by the same operator (A.P.). The lateral cephalograms were analyzed manually by using the method described by Pancherz, and several classic linear and angular measurements from the analyses of Steiner, Ricketts, and McNamara were measured with a customized digitization regimen (version 11; Dolphin Imaging, Chatsworth, Calif). The magnification factor of all lateral cephalograms was 8%.
Statistical analysis
The power of the study as calculated on the number of subjects enrolled in the prospective trial and the standard deviations of the chosen cephalometric variables at an alpha of 0.05 exceeded 0.90. An exploratory Shapiro-Wilks test showed normal distributions of the data in both the treated and control groups. Therefore, Student t tests were applied to compare the starting forms in the 2 groups at T1, and then for the T2-T1, T3-T2, and T3-T1 changes for all the cephalometric variables.
Lateral cephalograms were randomly chosen, retraced, and redigitized to calculate the method error with Dahlberg’s formula. Both intraoperator and interoperator measurement errors were analyzed. The intraoperator error was assessed by comparing 30 cephalograms measured by the operator (A.P.) at 2 time points ( t test for paired observations, P <0.05). The errors for linear measurements ranged from zero (molar relationship) to 0.3 mm (Co-Pg), and the errors for angular measurements varied from zero (y-axis) to 1.2° (L1 to GoMe). No differences between repeated measurements were significant. The interoperator error was assessed by comparing 20 cephalograms measured by the operator (A.P.) and another expert operator (N.E.T.) ( t test for independent observations, P <0.05). The errors ranged from 0.1 mm for Ar-Gn to 0.7° for U1 to SN. No differences in the measurements between the 2 operators were significant.
Results
The comparison between the treatment and control groups at T1 showed no statistically significant differences between them ( Table II ). Changes in the subjects in the treatment and control groups from T2 to T1, T3 to T2, and T3 to T1 are compared in Tables III to V . The results in the treated group were not used separately for statistical comparisons.
| Magnoglide total (n = 31) T2-T1 | Untreated Class II controls (n = 30) T2-T1 | Difference Magnoglide total – controls T2-T1 | Significance | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Cephalometric measurement | ||||||
| SNA (°) | −0.8 | 1.6 | 0.5 | 1.2 | −1.3 | * |
| SNB (°) | 0.4 | 1.5 | −0.2 | 1.5 | 0.6 | NS |
| ANB (°) | −1.2 | 1.1 | 0.4 | 1.2 | −1.6 | ‡ |
| SN-GoMe (°) | 0.7 | 1.5 | 0.5 | 2.2 | 0.2 | NS |
| Co-Gn (mm) | 5.2 | 1.9 | 2.7 | 2.2 | 2.5 | ‡ |
| Ar-Gn (mm) | 4.7 | 1.9 | 2.3 | 2.3 | 2.4 | ‡ |
| Y-axis (°) | 0.9 | 1.4 | 0.3 | 2.6 | 0.6 | NS |
| U1 to SN (°) | −3.6 | 4.5 | −1.4 | 3.6 | −2.2 | NS |
| L1 to GoMe (°) | 0.1 | 3.3 | −0.3 | 2.4 | 0.4 | NS |
| Pancherz analysis | ||||||
| Maxillary base (mm) ss/OLp(d) | 0.7 | 1.5 | 0.6 | 1.5 | 0.1 | NS |
| Mandibular base (mm) pg/OLp(d) | 2.6 | 2.6 | 0.7 | 2.2 | 1.9 | † |
| Maxillary incisor (mm) is/OLp(d) | −0.3 | 2.2 | 1.4 | 0.8 | −1.7 | † |
| Mandibular incisor (mm) ii/OLp(d) | 3.1 | 1.9 | 1.3 | 0.9 | 1.8 | † |
| Overjet (mm) is/OLp minus ii/OLp | −3.4 | 1.3 | 0.1 | 0.6 | −3.5 | ‡ |
| Maxillary molar (mm) ms/OLp(d) | −0.5 | 1.8 | 1.1 | 1.6 | −1.6 | ‡ |
| Mandibular molar (mm) mi/OLp(d) | 4.2 | 2.3 | 1.1 | 1.8 | 3.1 | ‡ |
| Molar relation (mm) ms/OLp minus mi/OLp | −4.7 | 1.4 | 0 | 0.8 | −4.7 | ‡ |
| Dental changes in the skeletal base | ||||||
| Maxillary incisor (mm) is/OLp(d) minus ss/OLp(d) | −1.0 | 1.6 | 0.8 | 0.9 | −1.8 | † |
| Mandibular incisor (mm) ii/OLp(d) minus pg/OLp(d) | 0.5 | 1.7 | 0.6 | 0.8 | −0.1 | NS |
| Maxillary molar (mm) ms/OLp(d) minus ss/OLp(d) | −1.2 | 1.1 | 0.5 | 0.6 | −1.7 | † |
| Mandibular molar (mm) mi/OLp(d) minus pg/OLp(d) | 1.6 | 2.1 | 0.4 | 1.1 | 1.2 | NS |
| Magnoglide total (n = 31) T3-T2 | Untreated Class II controls (n = 30) T3-T2 | Difference Magnoglide total – controls T3-T2 | Significance | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Cephalometric measurement | ||||||
| SNA (°) | 0.4 | 1.3 | 0.0 | 1.4 | 0.4 | NS |
| SNB (°) | 0.2 | 1.5 | −0.1 | 1.5 | 0.3 | NS |
| ANB (°) | 0.2 | 0.9 | −0.1 | 0.8 | 0.3 | NS |
| SN-GoMe (°) | −0.1 | 1.8 | −0.1 | 1.6 | 0.0 | NS |
| Co-Gn (mm) | 1.7 | 1.0 | 1.9 | 1.4 | −0.2 | NS |
| Ar-Gn (mm) | 1.5 | 1.6 | 1.6 | 1.4 | −0.1 | NS |
| Y-axis (°) | −0.4 | 1.6 | 0.1 | 1.7 | −0.5 | NS |
| U1 to SN (°) | −0.8 | 6.1 | 0.6 | 5.4 | −1.4 | NS |
| L1 to GoMe (°) | 4.8 | 5.2 | 0.5 | 6.2 | 4.3 | * |
| Pancherz analysis | ||||||
| Maxillary base (mm) ss/OLp(d) | 0.0 | 1.5 | 0.3 | 1.4 | −0.3 | NS |
| Mandibular base (mm) pg/OLp(d) | −0.4 | 2.7 | 0.1 | 2.5 | −0.5 | NS |
| Maxillary incisor (mm) is/OLp(d) | −1.0 | 2.5 | −0.1 | 2.4 | −0.9 | NS |
| Mandibular incisor (mm) ii/OLp(d) | 1.0 | 2.7 | −0.3 | 2.6 | 1.3 | NS |
| Overjet (mm) is/OLp minus ii/OLp | −2.0 | 1.8 | 0.2 | 0.4 | −2.2 | † |
| Maxillary molar (mm) ms/OLp(d) | 0.8 | 2.0 | 0.1 | 2.1 | 0.7 | NS |
| Mandibular molar (mm) mi/OLp(d) | −0.2 | 2.1 | −0.6 | 2.2 | 0.4 | NS |
| Molar relation (mm) ms/OLp minus mi/Olp | 1.0 | 1.5 | 0.7 | 0.8 | 0.3 | NS |
| Dental changes in the skeletal base | ||||||
| Maxillary incisor (mm) is/OLp(d) minus ss/OLp(d) | −1.0 | 1.9 | −0.4 | 0.6 | −0.6 | NS |
| Mandibular incisor (mm) ii/OLp(d) minus pg/OLp(d) | 1.4 | 3.0 | −0.4 | 0.7 | 1.8 | * |
| Maxillary molar (mm) ms/OLp(d) minus ss/OLp(d) | 0.8 | 1.6 | −0.2 | 0.7 | 1.0 | NS |
| Mandibular molar (mm) mi/OLp(d) minus pg/OLp(d) | 0.2 | 2.0 | −0.7 | 0.8 | 0.9 | NS |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


