Short-root anomaly is a rare condition, but it can be a problem for orthodontists and their patients. Our aim in this article was to report the treatment of an orthodontic patient with short-root anomaly, highlighting the diagnostic aspects involved and the strategy used.
Short-root anomaly (SRA) is a rare condition, with a prevalence estimated at 1.3%. It is more common in female patients and principally affects the premolars and the maxillary incisors, the apexes of which are rounded rather than the usual pointed shape. The condition has a genetic background and is related to other dental anomalies, such as agenesis, invaginated teeth, conoid teeth, supernumerary teeth, microdontia, taurodontia, pulp calculus, and type I dentin dysplasia. Moreover, it can be related to syndromes, such as Down and Stevens-Johnson. SRA has also been associated with exogenous factors, including radiation of the head and neck or chemotherapy in children with malignant tumors during dental development.
Short dental roots, resulting in unfavorable root-crown ratios, can affect the prognosis of teeth and complicate the treatment plan in orthodontics and prosthodontics when considering aspects such as anchoring and the capacity of teeth to bear mastication forces. Specifically in orthodontic patients, this problem takes on an even more critical dimension, because of the tendency in patients with short roots toward root resorption during orthodontic treatment. Moreover, anomalies such as agenesis, ectopic teeth, and taurodontism are risk factors for periapical resorption.
Although SRA is a potential problem in the clinical practice of orthodontists, no studies were found that directly address this subject. Thus, our aim in this study was to present the treatment of an orthodontic patient with SRA, highlighting the diagnostic aspects involved and the strategy used.
Case report
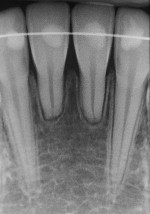
A girl, aged 10 years 7 months, sought orthodontic care, accompanied by her parents. Their objective was to continue the treatment that had been started 6 months earlier by another orthodontist. The girl had an orthodontic appliance in her maxillary arch from second premolar to second premolar ( Fig 1 ). She had a mesofacial growth pattern, a convex facial profile, and a Class II dental and skeletal malocclusion. The radiographs showed SRA in the maxillary and mandibular central incisors and first premolars ( Fig 2 ). The mandibular central incisors were affected to the greatest degree. There were no reports of disease or systemic abnormalities.


The new treatment plan involved removal of the fixed appliance and placement of a functional orthopedic appliance aimed at mandibular advancement ( Fig 3 ). Headgear was also prescribed to limit the anterior movement of the maxilla. After 8 months of functional orthopedic appliance treatment, the patient exhibited significant mobility in the mandibular central incisors. The decision was then made to place a fixed lingual retainer, with a 0.025-mm braided fiber, on the mandibular incisors and canines ( Fig 4 ). After 19 months of retention, there was stability of the sagittal correction and satisfactory intercuspation ( Fig 5 ). Throughout this period, there was no change in the amount of root shortening ( Fig 6 ).