Stability and prognosis of teeth with severe root resorption is problematic in orthodontics. Because severe root resorption, when it occurs in orthodontic patients, is an iatrogenic consequence of treatment, periodic analysis for all patients is encouraged. This article reports a case of severe root resorption 25 years after the completion of orthodontic treatment. The root resorption did not exhibit significant progression and the patient had a healthy periodontal status. Orthodontic patients with sharp, pointed roots who require premolar extraction might have a greater risk of severe root resorption.
Severe root resorption is characterized by the loss of more than one third of root length. This condition can compromise the success of orthodontic treatment, reduce tooth longevity and capacity to endure mastication forces, and limit its use as an anchor in prosthetic rehabilitation.
Although the association between root resorption and orthodontic treatment has been studied for years, there is no consensus in the literature regarding the causes of this condition. Generalized resorption of more than 3 mm occurs in 4% of orthodontic patients. At least 5% of adults and 2% of adolescents are prone to having 1 or more teeth with more than 5 mm of resorption during orthodontic treatment with fixed appliances. The problem becomes even more critical because there are few studies that assess the posttreatment stability and prognosis of teeth with severe root resorption. Extensive root resorption induced by orthodontic movement could be influenced by problems with the predictability, prevention, and early diagnosis of this condition.
This paper reports a case of severe root resorption associated with orthodontic treatment and discusses the clinical implications concerning the diagnosis and treatment carried out. It also describes the clinical and radiographic status of the same patient 25 years after completing orthodontic treatment.
Case report
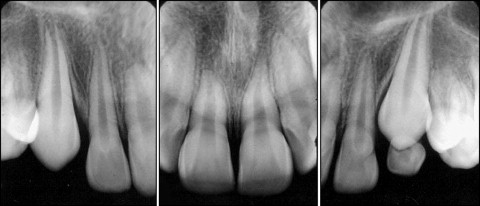
A male patient aged 10 years 4 months presented with an esthetic complaint of dental biprotrusion. The patient had a symmetrical face, protruding profile, good overall health status and oral hygiene, and normal breathing, deglutition, and dental eruption. The molar relationship was defined as Angle Class I malocclusion. The patient presented a 5-mm overjet and slight overbite. The lower arch exhibited minor crowding and there was gyration of the premolars and molars. There were no harmful oral habits. Radiographic analysis revealed the presence of all teeth, with the incisors exhibiting a small crown-to-root proportion and the roots were thin and pointed ( Fig 1 ).
The treatment plan involved a fixed upper and lower appliance (banded) and the use of headgear with the aim of aligning and evening the dental arches. Subsequently, there would be the use of intermaxillary elastic bands in order to promote a better dental intercuspidation. The pure edgewise method was employed.
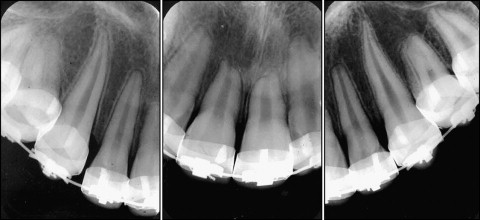
Treatment began in July 1974. Two years later, the patient was uncooperative regarding the use of the headgear. The decision was made to restudy the case, culminating in the option to extract the 4 first premolars. Periapical radiographs taken at this time revealed one-third resorption of the upper incisors, with the respective apices taking on an obtuse form ( Fig 2 ).
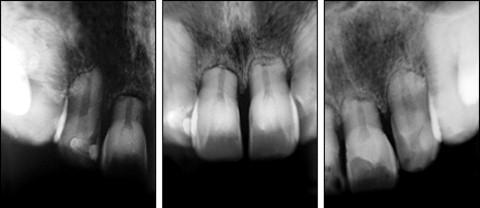
The treatment proceeded with little cooperation from the patient regarding the use of the headgear. In 1982, the bands on all the teeth were replaced with braces. There was also an indication for the use of Class II 1/4 intermaxillary elastic bands 16 hours per day. In 1983, the treatment was finalized, and a Hawley retainer and lower bicanine brace were placed. The periapical radiographs taken at the end of the treatment revealed severe horizontal resorption of the upper and lower incisors and slight resorption of the upper and lower canines ( Fig 3 ). Twenty-five years after completing treatment, new radiographs were taken and a new periodontal evaluation was performed, revealing that the root resorption did not exhibit significant progression ( Fig 4 ) and the patient had a healthy periodontal status.

Discussion
The case presented illustrates the occurrence of severe root resorption associated with orthodontic treatment and its evolution 25 years after completion of treatment. During the anamnesis, the patient reported no systemic disorder that could be associated with the risk of developing severe root resorption. Although the patient had no signs of root resorption at the beginning of treatment, he presented thin, pointed incisor roots. Current evidence states that pointed roots or those in the shape of a pipette are more prone to developing external apical root resorption. At the beginning of treatment, however, little attention was given to this issue, based on the information on the patient’s clinical chart and on the information about root resorption available at that time.
As the patient had dental biprotrusion and was motivated for treatment, the decision was made to use headgear. However, because of the lack of cooperation on the part of the patient regarding the use of the headgear, the case was restudied and the decision was made to extract the 4 first molars. At this time, active resorption was also observed in the upper and lower anterior teeth, which indicated a greater risk for the development of severe root resorption throughout the treatment. Furthermore, the treatment was prolonged because of changes in the planning and the frequent poor attendance of the patient regarding the orthodontic appointments. According to Mirabella and Artun, the duration of the active phase is a risk factor for the occurrence of severe root resorption. In a recent meta-analysis, Segal et al stressed that the need for prolonged treatment involving significant degrees of dental movement is a strong risk factor for severe resorption. Thus, the long duration of treatment, the retraction mechanics employed, and prolonged use of intermaxillary elastic bands may have contributed significantly to the severe root resorption in this patient. Furthermore, during treatment, the orthodontist did not observe any predisposing signs in the patient for the occurrence of severe root resorption. This resorption could have been easily noticed in periapical radiographs of the anterior teeth in the first 6 months after beginning treatment. The early detection of slight root resorption during orthodontic treatment is essential to the identification of teeth with a risk of severe resorption.
It is currently known that the root resorption process is interrupted once the applied force is removed. After a few days, the repair of the resorption gaps is observed, with the depositing of cementum. Thus, the inclusion of rest periods (with no application of force) in the treatment of patients with a tendency toward root resorption is important. In the case described here, there was no interruption of the active phase of treatment to minimize the progression of the resorption process. This certainly had a direct contribution to the degree of root resorption, which became increasingly more accentuated.
Severe apical root resorption is an undesirable consequence of orthodontic treatment and has received considerable attention because of the medical-legal implications. As severe root resorption is an iatrogenic consequence of orthodontic treatment, orthodontists must carry out a risk-benefit analysis for all patients, considering the likely iatrogenic responses to treatment.
Currently, there is no consistent evidence regarding the long-term stability of teeth with severe root resorption. In this context, an important factor in the case presented here is the fact that the patient reported healthy oral hygiene habits over the years and frequent visits to a dentist for prophylactic procedures. Another significant aspect in the patient’s report is that over the 25 years after orthodontic treatment, he was never concerned with or was instructed to restrict the foods to be chewed. This is an aspect that also may have received little attention, as the magnitude of root resorption could compromise mastication function and efficiency with foods of a harder consistency.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


