Introduction
Our objective was to compare root resorption degree of the maxillary central incisors retracted with and without skeletal anchorage.
Methods
This nonrandomized historical control study included 37 patients requiring maximum anterior retraction and treated with extraction of 2 maxillary premolars. Group 1 consisted of 22 patients (11 male, 11 female) in whom anterior retraction was performed without skeletal anchorage, and group 2 included 15 patients (3 male, 12 female) treated with skeletally anchored anterior retraction. Periapical radiographs were used to evaluate root resorption degree by a scoring system. The groups were compared regarding the resorption score and resorption degree distribution with the Mann-Whitney U test, chi-square test, and Z test on proportions.
Results
There was no statistically significant intergroup difference regarding root resorption, but the number of patients with severe and extreme root resorption degrees was significantly greater in group 2.
Conclusions
Although the root resorption degree of the skeletal anchorage group was not significantly different from the group without skeletal anchorage, the number of patients with severe to extreme resorption in the first group was significantly greater. Therefore, careful clinical monitoring of skeletally anchored anterior retraction is needed, especially when there are known root resorption predisposing factors.
Highlights
- •
Incisors retracted with skeletal and conventional anchorage had similar root resorption.
- •
Skeletal anchorage showed slightly greater horizontal apex displacement of the inciors.
- •
Retraction with mini-implants had more incisors with moderate to severe root resorption.
- •
Extreme root resorption is uncommon in both anchorage methods.
- •
No incisors were free of root resorption in either anchorage method.
External apical root resorption (EARR) is a well-known sequelae of orthodontic treatment. The concentration of forces on the root apex during tooth movement is a mechanical effect that seems to trigger biologic events associated with apical root resorption especially in deviated root shapes. Excessive orthodontic loading can lead to more destruction of cementoblasts by compression of these cells and the periodontal blood vessels, increasing tooth root vulnerability to the resorption process.
Several studies have demonstrated that maxillary incisors are the most affected teeth by EARR and that horizontal displacement of the tooth root during orthodontic treatment is positively associated with incisor root shortening mainly in extraction patients. Anterior retraction anchored on mini-implants can produce greater incisor displacement and less anchorage loss when compared with orthodontic mechanics with conventional anchorage.
Occlusal and esthetic results of some Class II malocclusions and bialveolar dental protrusion can be significantly benefitted if premolars are extracted and maximum incisor retraction is performed with skeletal anchorage. However, root resorption susceptibility of the maxillary incisors could be increased by greater displacement of these teeth and longer treatment time during skeletally anchored anterior retraction. Taking into account this risk/benefit relationship and the scarcity of scientific studies evaluating root resorption of incisors retracted with skeletal anchorage, the purpose of this study was to evaluate the following null hypothesis: root resorption degrees of the maxillary central incisors are similar during anterior retraction with conventional and skeletal anchorage.
Material and methods
The orthodontic records were obtained from the files of the Department of Orthodontics at Bauru Dental School, University of São Paulo, Brazil. Group 1 was retrospectively selected from the records of patients who sought orthodontic treatment and satisfied the inclusion and exclusion criteria for group 2 selection. Group 2 was prospectively selected according to the following criteria: Class II Division 1 malocclusion or Class I with biprotrusion requiring 2 maxillary first premolar extractions and maximum anterior retraction for occlusal and esthetic improvement; no history of trauma to the maxillary incisors; no endodontic treatment or preexisting resorption on the initial periapical radiographs, and maxillary crowding smaller than 3 mm. Patients with supernumerary or impacted teeth, malformed roots, tooth shape and size anomalies, and previous orthodontic treatment were excluded. There was no distinction for race, sex, or socioeconomic aspects in the selection process of these patients.
Sample size calculation took into account the value of measurement variances of a similar study, which evaluated maxillary incisor resorption after orthodontic treatment with fixed appliance using the Malmgren scoring system. The sample size was adjusted to detect a mean score difference of 0.5 between the groups, with power of 80% at a significance level of 5%. These parameters determined a minimum sample size of 12 subjects in each group.
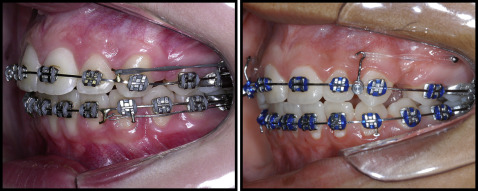
Similar initial anteroposterior discrepancies to be corrected with maximum anterior retraction were selected in both groups. Group 1 included 22 patients (mean age, 14.04 ± 2.83 years; 11 boys, 11 girls) with severe Class II maloccusion requiring maximum anterior retraction. Group 2 included 15 patients (mean age, 19.87 ± 5.86 years; 3 male, 12 female) with similar malocclusion type and severity, except for 2 patients who had Class I with biprotrusion. All patients had 2 maxillary first premolar extractions and maximum anterior retraction, performed without skeletal anchorage (group 1) and with skeletal anchorage (group 2). The patients in both groups had no history of previous orthodontic treatment. No patient had rapid maxillary expansion previously performed, and similar orthodontic mechanics were applied to both groups using fixed 0.022 × 0.028-in preadjusted edgewise appliances (Roth prescription). A typical wire sequence characterized by 0.014-in and 0.016-in nickel-titanium archwires, followed by 0.016-, 0.018-, 0.020-, and 0.019 × 0.025-in stainless steel archwires was used for leveling and alignment. Anterior retraction was performed with continuous rectangular stainless steel archwires (0.019 × 0.025-in; Fig 1 ). Orthodontic forces of 250 g were applied on each side with intramaxillary elastic chains extending from the retraction hook to the first molar tube hook (group 1) or to the mini-implant (group 2) to retract the maxillary anterior teeth en masse ( Fig 1 ). The anterior retraction force was activated monthly and measured with an orthodontic tension gauge (Correx series 040-712-00; Dentaurum, Ispringen, Germany). In group 1, cervical headgear was used during anterior retraction to prevent anchorage loss with an average wear time of 14 to 16 hours per day. Patients treated with mini-implants did not have Class II correction with intermaxillary elastics, and 14 noncompliant patients with the anchorage reinforcement appliance had the Class II canine relationship normalized with intermaxillary elastics after extraction space closure for a mean time of 5.85 months. Total treatment times were calculated for both groups.
Mini-implants were inserted near the mucogingival line for all patients of group 2 under local infiltrative anesthesia in the maxillary buccal alveolar bone between the maxillary first and second premolar of each side to anchor the anterior retraction forces. The insertion protocol was performed without cortical bone drilling with a surgical drill, and the mini-implants were manually screwed with a screwdriver using surgical techniques previously proposed by the authors. A radiographic-surgical guide was used to allow mini-implant insertion in anatomic sites with critical interradicular septum width at the cervical area, avoiding excessive apical positioning of the mini-implants. Self-drilling 1.5 × 7 mm mini-implants (SH 1514-07; Absoanchor, Dentos, Daegu, Korea) were used in this study.
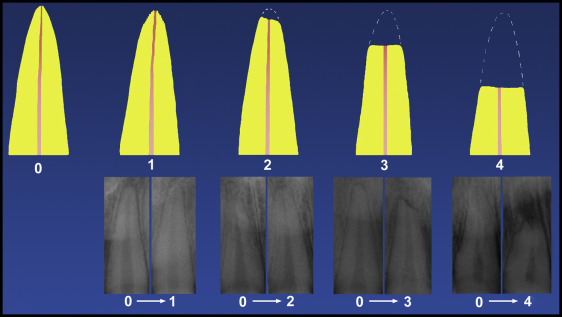
Periapical radiographs were taken at the end of treatment using the paralleling technique. All periapical radiographs were selected by the quality of the image, and radiographs with either excessive distortion or lack of clarity were not considered. To classify the severity of resorption in the roots of the maxillary central incisors during anterior retraction, pretreatment periapical radiographs were taken as a parameter ( Fig 2 ). To minimize the standardization problem between the periapical radiographs, the scoring system proposed by Malmgren et al was used to quantify root resorption degree instead of metrical evaluation. The classification consists of 5 scores ( Fig 2 ): 0, no root resorption; 1, mild resorption, with only an irregular outline and the root showing normal length; 2, moderate resorption, with little loss of root and the root apex showing an almost straight outline; 3, sharp resorption, with great root loss, reaching almost a third of its length; and 4, extreme resorption, with loss greater than a third of the root length.
The periapical radiographs were scanned with the Sprint Scan 35 Plus scanner (version 2.7.2; Polaroid, Cambridge, Mass) with a resolution of 675 dpi and a 1:1 ratio or 100%. The images were analyzed with Adobe Photoshop CS (version 8.0; Adobe, San Jose, Calif) and could be enlarged up to 300% to improve the evaluation accuracy without loss of quality. The evaluations were blindly conducted in a twilight atmosphere by 2 examiners (V.O.B., K.C.). Any disagreements were resolved by a weighted reevaluation to the satisfaction of both examiners. The mean score between the right and left maxillary central incisors was calculated for each patient.
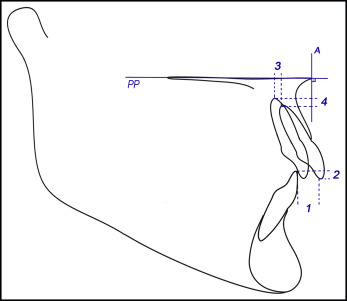
The cephalometric characteristics studied consisted of initial overjet and overbite, changes in overjet and overbite, and horizontal and vertical displacements of the maxillary central incisor apices ( Fig 3 ). The pretreatment and posttreatment lateral cephalometric radiographs were traced by the same examiner (K.C.), and checked for outline of the anatomic structures and landmark demarcation by a second examiner (S.E.B.). Cephalograms were digitized, and the data were analyzed with Radiocef Studio 2 software (version 2.0, release 12.82; Radio Memory Ltda, Belo Horizonte, Brazil), which corrected the magnification factors of the radiographs. Treatment changes were calculated as pretreatment minus posttreatment values.
Statistical analyses
To evaluate measurement errors of the radiographic analysis, 15 posttreatment periapical radiographs were randomly selected and remeasured after 2 weeks. Intraobserver agreement was determined by the weighted Cohen kappa (kw) coefficient.
All continuous variables were evaluated regarding normality using the Shapiro-Wilk test ( Table I ). The degree of root resorption in the groups was compared using the mean score of root resorption of the 2 maxillary central incisors of each patient. Since the mean scores obtained from an ordinal scale can have a normal distribution, the Shapiro-Wilk test was also used to evaluate data distribution and normality ( Table I ).
| Variable | Group 1 | Group 2 | ||
|---|---|---|---|---|
| W | P | W | P | |
| Malmgren score | 0.892 | 0.021 ∗ | 0.878 | 0.045 ∗ |
| Age | 0.875 | 0.009 ∗ | 0.869 | 0.033 ∗ |
| Crowding | 0.935 | 0.159 | 0.866 | 0.032 ∗ |
| Treatment time | 0.956 | 0.422 | 0.983 | 0.986 |
| Overjet (T1) | 0.905 | 0.044 ∗ | 0.920 | 0.394 |
| Overjet (T1-T2) | 0.900 | 0.038 ∗ | 0.892 | 0.213 |
| Overbite (T1) | 0.958 | 0.481 | 0.968 | 0.881 |
| Overbite (T1-T2) | 0.940 | 0.225 | 0.933 | 0.518 |
| Horizontal apex displacement (T1-T2) | 0.937 | 0.196 | 0.900 | 0.252 |
| Vertical apex displacement (T1-T2) | 0.939 | 0.209 | 0.816 | 0.318 |
According to normality tests, parametric ( t test) and nonparametric (Mann-Whitney rank sum test) tests were used to compare the groups regarding root resorption degree, initial age, crowding severity, treatment time, initial overjet and overbite, overjet and overbite treatment changes, and incisor apex displacements. Intergroup sex distribution was compared with the chi-square test.
The distribution of root resorption scores between the groups was evaluated with the chi-square test. The percentages of patients with slight to moderate and with severe to extreme root resorption in each group were compared with the Z test on proportions.
Since the groups were not matched for sex and age, the influence of these variables on root resorption was evaluated using the Mann-Whitney rank sum test and the Spearman correlation test. Results were considered statistically significant at P <0.05.
Results
Intraobserver agreement was considered high with a weighted Cohen kappa coefficient of 0.809 (95% confidence interval, 0.63-0.98). The agreement percentage between the first and second root resorption evaluations was 83.33% ( Table II ).
| Variable | Weighted kappa coefficient | SE | 95% CI | Percentage of agreement | Strength of agreement ∗ |
|---|---|---|---|---|---|
| Intraobserver agreement | 0.809 | 0.09 | 0.63-0.98 | 83.33% | Substantial |
∗ According to the classification suggested by Landis and Koch for kappa test results.
There was no statistically significant difference between the groups regarding root resorption ( Table III ). Initial age and sex distributions were not similar between the groups. The groups had similar crowding, treatment times, initial overjet and overbite, changes in overjet and overbite, and vertical incisor apex displacements. The skeletal anchorage group had a greater horizontal incisor apex displacement ( Table III ).
| Variable | Group 1 (n = 22) | Group 2 (n = 15) | P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Lower quartile | Upper quartile | Median | Mean ± SD | Lower quartile | Upper quartile | Median | Mean ± SD | ||
| Resorption degree | 1 | 2.5 | 2 | 1.81 ± 0.73 | 1.5 | 3 | 2 | 2.33 ± 0.77 | 0.061 † |
| Initial age | 12.91 | 14.91 | 13.45 | 14.04 ± 1.83 | 13.00 | 28.25 | 18.08 | 19.87 ± 6.87 | 0.008 ∗ † |
| Crowding | −3 | 0.00 | −1.5 | −1.02 ± 1.83 | −3 | 0.00 | −1 | −1.2 ± 1.86 | 0.768 † |
| Treatment time | 2.22 | 2.95 | 2.69 | 2.69 ± 0.65 | 2.69 | 3.16 | 2.97 | 2.92 ± 0.32 | 0.203 ‡ |
| Overjet (T1) | 5.14 | 7.98 | 6.03 | 6.73 ± 2.48 | 6.21 | 8.12 | 6.66 | 6.98 ± 1.67 | 0.353 † |
| Overjet (T1-T2) | 2.82 | 4.46 | 3.91 | 4.06 ± 2.46 | 4.16 | 6.39 | 4.51 | 4.89 ± 1.73 | 0.141 † |
| Overbite (T1) | 1.51 | 4.79 | 3.38 | 3.30 ± 2.03 | 2.94 | 4.32 | 3.44 | 3.62 ± 1.26 | 0.593 ‡ |
| Overbite (T1-T2) | 0.31 | 2.99 | 1.91 | 1.75 ± 1.84 | 1.18 | 2.5 | 1.34 | 1.61 ± 1.25 | 0.802 ‡ |
| Horizontal apex displacement (T1-T2) | −3.71 | −1.83 | −2.95 | −2.59 ± 1.35 | −5.62 | −2.43 | −3.38 | −3.75 ± 1.85 | 0.036 ∗ ‡ |
| Vertical apex displacement (T1-T2) | 0.14 | 1.62 | 0.85 | 1.03 ± 1.03 | 1.12 | 2.14 | 1.57 | 1.22 ± 2.08 | 0.719 ‡ |
| Sex distribution | 11 boys, 11 girls | 3 boys, 12 girls | 0.021 ∗ § | ||||||
Group similarity regarding root resorption was not kept when the score distribution was compared between them ( Tables IV and V ). Group 2 had more severe root resorption scores; consequently, there were significantly more patients in group 1 with scores from 1 to 2, and in group 2 there were more patients with scores from 3 to 4 ( Tables IV and V ).
| Score | Group 1 (n = 44) | Group 2 (n = 30) | Total (n = 74) | ||
|---|---|---|---|---|---|
| n | % | n | % | n | |
| 0 | 0 | 0.00 | 0 | 0.00 | 0 |
| 1 | 17 | 38.64 | 5 | 16.67 | 22 |
| 2 | 19 | 43.18 | 11 | 36.67 | 30 |
| 3 | 7 | 15.91 | 13 | 43.33 | 20 |
| 4 | 1 | 2.27 | 1 | 3.34 | 2 |
| Chi-square = 8.12 | df = 3 | P = 0.0435 ∗ | |||
Gender was not associated with the root resorption degree in conventional anchorage group. Patient age was not significantly correlated with root resorption in this sample ( Table VI ).
| Variable | Group 1 boys (n = 11) | Group 1 girls (n = 11) | P | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Lower quartile | Upper quartile | Median | Mean ± SD | Lower quartile | Upper quartile | Median | Mean ± SD | ||
| Root resorption degree | 1 | 2 | 2 | 1.81 ± 0.84 | 1 | 2.5 | 2 | 1.81 ± 0.63 | 0.767 ∗ |
| Root resorption degree × patient age | R = 0.169 | 0.316 † | |||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


