This article discusses contemporary pediatric restorative dentistry. Indications and contraindications for the choice of different restorative materials in different clinical situations, including the risk assessment of the patient, are presented. The specific use of glass ionomer cement or resin-modified glass ionomer cement, resin-based composite, and stainless steel crowns is discussed so that preparation design and restoration placement is understood.
Key Points
- •
The indications and contraindications of the use of dental restorative materials are identified, including the implementation of risk assessment in decision making.
- •
The specific clinical use of glass ionomer cement/resin-modified glass ionomer cement is presented.
- •
The specific clinical use of resin-based composite is presented.
- •
The specific clinical use of full-coverage stainless steel crowns is presented.
Introduction
Initiating preventive dentistry care for children, preferably beginning no later than the age of 1 year, helps prevent dental caries. Although it is ideal to strive for children to be caries free, data indicate that 70% of children have experienced at least 1 cavitated carious lesion by age 17. Many children, particularly children at high risk for dental caries, still experience cavitated lesions in both the primary and permanent dentitions.
Using the concept of minimally invasive dentistry, restoration placement is a last resort when prevention of a cavitated lesion has failed. Teeth can be restored using a minimally invasive restorative protocol with restorative materials that most appropriately meet the needs of the patient, risk assessment, age of the patient, size of the cavitated lesion, and ability to isolate the cavity preparation all being important considerations.
Introduction
Initiating preventive dentistry care for children, preferably beginning no later than the age of 1 year, helps prevent dental caries. Although it is ideal to strive for children to be caries free, data indicate that 70% of children have experienced at least 1 cavitated carious lesion by age 17. Many children, particularly children at high risk for dental caries, still experience cavitated lesions in both the primary and permanent dentitions.
Using the concept of minimally invasive dentistry, restoration placement is a last resort when prevention of a cavitated lesion has failed. Teeth can be restored using a minimally invasive restorative protocol with restorative materials that most appropriately meet the needs of the patient, risk assessment, age of the patient, size of the cavitated lesion, and ability to isolate the cavity preparation all being important considerations.
Glass ionomer cement/resin-modified glass ionomer cement
Fluoride release occurs during the glass ionomer cement setting reaction and continues at low fluoride release levels for years. There is an advantage of using glass ionomer cement restorations in children that are at moderate risk for the development of caries or secondary caries because the fluoride associated with the glass ionomer restorative materials can inhibit tooth demineralization at the restoration cavosurface margin.
Occlusal Restorations
Occlusal glass ionomer cement restorations have shown clinical success. Contemporary heavily filled glass ionomer cements and resin-modified glass ionomer cements have compressive strengths that provide adequate wear properties for the posterior primary dentition. Glass ionomer would be considered for occlusal restorations when there might be difficulty in isolating a tooth to keep it dry enough for the placement of a resin-based composite restoration.
Class II Restorations
Class II resin-modified glass ionomer cement restorations have shown clinical success. The advantage of not needing to acid-etch tooth structure before restoration placement and knowing the glass ionomer chemical reaction will occur even with mild saliva contamination, makes the material favorable for the pediatric patient, in whom speed is critical and tooth isolation difficult.
Preparation design for class II glass ionomer cement restorations in the primary dentition is similar to amalgam preparations. The proximal box should be deep enough to break contact, and the axial wall should ideally extend 1.25 mm. The lateral walls should slightly converge to the occlusal, which aids in mechanical retention of the restorative material. The proximal box buccal and lingual walls should remain within the line angles of the tooth; breaking buccal or lingual contact is not necessary. No cavosurface bevels are placed in glass ionomer cement preparations because glass ionomer cement is brittle and could easily break or chip at beveled cavosurface beveled margins. After preparation, a matrix band or T-band is placed interproximally and wedged firmly so that the restorative material can be placed and adapted into the cavity preparation, and an adequate contact point can be created with the adjacent tooth.
Class III Restorations
Class III glass ionomer cement restorations have shown clinical success. These glass ionomer cement restorations would be indicated when perfect isolation for a resin-based composite restoration is not possible. Lingual access for maxillary anterior teeth and labial access for mandibular anterior teeth is appropriate for class III preparations.
Class V Restorations
Class V glass ionomer cement restorations have shown clinical success in the primary dentition. Glass ionomer cement/resin-modified glass ionomer cement class V restorations are indicated when good isolation of the tooth is difficult or impossible for the placement of a resin-based composite restoration.
The Class V glass ionomer preparation design extends 1.25 mm pulpally, unless caries progresses further. No bevels are placed on the cavosurface margin because of the brittle nature of glass ionomer cement and potential for fracture at a beveled cavosurface margin.
Interim Therapeutic Restoration
The interior therapeutic restoration is the current term used in place of the initially introduced term atraumatic restorative technique . Atraumatic restorative technique was introduced in areas in which contemporary air-driven hand pieces and suction were not readily available. Hand instruments were used to remove caries, then chemically cured glass ionomer cement was placed as a restorative material. This technique originated for use in third-world countries, where access to dental care was difficult. Today, the interim therapeutic restoration is thought to be more descriptive of the procedures performed, particularly in the United States.
Resin-based composite
Occlusal Restorations
Resin-based composite is the restorative material of choice for occlusal restorations when the tooth can be adequately isolated. The wear and compressive strength of currently available resin-based composites have shown clinical success for occlusal and class II posterior restorations.
Occlusual preparations extend as far as caries progresses. Cavosurface margins are beveled, and heavily filled resins are used to withstand occlusal stress and wear. Any pits and fissures not included in the preparation can have sealant placed to prevent the development of future caries. Enamel should be acid etched with 35%–40% phosphoric acid for 15–30 seconds and thoroughly rinsed, then a resin adhesive placed according to the manufacturer’s instructions. If the preparation extends well into dentin, a glass ionomer cement base can be used to replace dentin, then a heavily filled resin-based composite should be placed in 2-mm increments to ensure that the material is polymerized adequately. Restorations are finished and polished and a final adhesive is then placed to fill in any imperfections created during finishing and to reach maximum polymerization at the restoration surface.
Class II Restorations
Class II resin-based composite has shown clinical success. The American Dental Association Statement on Posterior Resin-Based Composites reports that recommendations for class II restorations were for preparations that did not include restoration margins exhibiting heavy occlusal wear, that is, restorations that do not extend beyond the line angles of the tooth or approximately one-half the intercuspal distance.
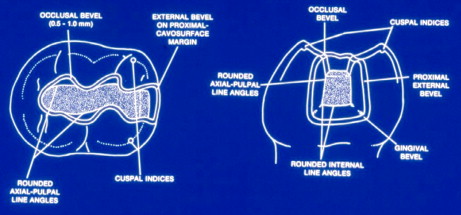
The class II resin-based composite preparation design is similar to that of the class II glass ionomer cement preparation in the primary dentition ( Fig. 1 ). The main difference is that a cavosurface bevel is placed on all enamel margins in a resin-based composite preparation. The proximal box should ideally just break gingival contact; the buccal and lingual walls should be within the line angles and converge toward the occlusal. There should be an occlusal extension from the proximal box that dovetails into the occlusal surface to provide additional retention. A matrix or T-band is placed interproximally and firmly wedged to achieve an adequate restoration contact point. After bevel placement on cavosurface margins, the tooth is acid etched with 35%–40% phosphoric acid for 15–30 seconds; the chosen adhesive should be placed according to manufacturer’s instructions, and resin-based composite is then placed and polymerized in 2-mm increments. The matrix is removed and the restoration is finished and polished, followed by the placement of an adhesive over the polished surface of the restoration.
Class III Restorations
Class III resin-based restorations have shown clinical success and have been recommended for the primary and permanent dentitions. These restorations are appropriate for anterior teeth that can be adequately isolated to prevent contamination during restoration placement. The incisal edge should be intact after preparation to adequately retain the resin-based composite. Patients considered at high-risk for future caries development may be better served with more aggressive treatment, such as placement of full tooth coverage restorations. Lingual preparation access is recommended for maxillary anterior teeth and labial preparation access is recommended for mandibular anterior teeth. The box of the preparation should extend to where caries has progressed, and all enamel cavosurface margins should be beveled. Resin-based composite is then placed in 2-mm increments and polymerized and the restorations finished and polished as previously described.
Class IV Restorations
Class IV resin-based composite restorations have been recommended for the primary and permanent dentions. Although class IV restorations would be unusual in the primary dentition, because in most circumstances a strip crown would be appropriate, there may be circumstances in which minimal enamel is chipped and a resin can be placed. Class IV resin-based composite restorations in the permanent anterior dentition have been recommended as an esthetic and effective restoration. Contemporary highly filled resin-based composites offer greater strength to restorations than the lower-filled resins used traditionally. Because of this increased strength, a beveled chamfer preparation can offer additional bond strength to prevent fracture at the margin of the restoration.
Class V Restorations
Class V resin-based composite restorations have been recommended for the primary and permanent dentions. Isolation is critical to prevent contamination of the acid-etched preparations during restoration placement. Cavity preparation should extend only as far as caries has progressed. Ideally, the axial wall would extend 1.25 mm, and all internal walls should be rounded. Mechanical retention is created naturally with the use of a #330 bur. Enamel cavosurface margins should be beveled. A glass ionomer liner/base can be placed over prepared dentin, or a dentin adhesive can be placed over prepared dentin following manufacturer’s instructions. Enamel margins are acid etched with 35%–40% phosphoric acid for 15–30 seconds, adhesive is applied according to manufacturer’s instructions, and then resin-based composite is placed and polymerized in 2-mm increments. Finishing and polishing is accomplished as previously discussed.
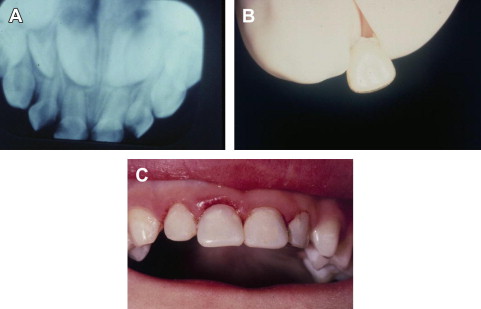
Strip Crown Restorations
Bonded resin-based composite strip crowns have been recommended for the restorations of multiple-surface carious primary incisors. Adequate tooth structure is necessary after cavity preparation to support the bonding of a strip crown. Gingival health is also important when placing strip crowns. Gingivitis leads to bleeding at pressure contact; therefore, the pressure created by the celluloid strip crown forms can cause bleeding.
Preparation design for strip crowns includes reduction of the incisal edge 1.5 mm, reduction of proximal surfaces 1.0–1.5 mm with tapering toward the incisal edge, then placement of a labial-incisal and lingual-incisal bevel.
The appropriate celluloid crown is then selected. The natural mesiodistal width of the unprepared tooth is the easiest dimension to use when selecting the appropriate celluloid crown size. The gingival margin of the celluloid crown can be cut with scissors to adapt to the natural free gingival margin. The prepared tooth structure is then acid-etched with 35%–40% phosphoric acid for 15–30 seconds. Bonding adhesive is applied according to manufacturer’s instructions, and then a celluloid crown that has been approximately half filled with resin-based composite is fit onto the prepared tooth ( Fig. 2 ). The recommendation is to place a small hole in the incisal edge of the celluloid crown form so that excess resin can extrude through the hole. This method relieves the creation of air voids within the strip crown resin. Excess resin is removed from the gingival margin and the incisal edge of the celluloid crown, and then the resin is polymerized from both the facial surface and lingual surface. The celluloid crown form is peeled away, and there should be minimal finishing and polishing needed. Occlusion should be checked to see that the restoration is in normal occlusion and does not have premature incisal contact.