Type of tooth preparation
% reduction in stiffness
Conservative endodontic access
5
Occlusal cavity preparation
20
MO or DO preparation involving at least one marginal ridge
46
MOD preparation involving both marginal ridges
63
The prognosis of an endodontically treated tooth depends on the quality of endodontic treatment and minimizing the chances for leakage of oral fluids and microbes into the canal space by prompt placement of a coronal restoration. In fact, it has been shown that only after 3-day exposure to artificial saliva, there was extensive coronal leakage through apparently sound endodontic gutta-percha fillings (Saunders and Saunders 1994). In a retrospective study of 1273 endodontically treated posterior teeth without coronal coverage (i.e., lacking a restoration that at least covers cusps), the failure rate was between 39 and 50 % (Sorensen and Martinoff 1984a). In another study, endodontically treated teeth that were not crowned after obturation failed at a rate six times greater than teeth crowned after obturation (Aquilino and Caplan 2002). When 220 endodontically treated permanent molars without coronal coverage were evaluated, overall survival (i.e., lack of tooth fractures) at 1, 2, and 5 years were 96 %, 88 %, and 36 %, respectively (Nagasiri and Chitmongkolsuk 2005). The 5-year survival rate of molars with Class I access cavity preparations and at least 2.0 mm of axial wall thickness was 78 % (i.e., 22 % had failed). More than 50 years ago, Rosen (1961) described the hugging action (encirclement) of vertical axial tooth structure provided by a crown, and he referred to it as the extracoronal brace. Encirclement of a circumferential area of axial dentin superior to the preparation finish line is known today as the ferrule effect, which protects a tooth from fracture. This concept will be described further.
The advantages of adhesive restorations (dentin bonding) have misled some clinicians into believing that the creation of a monoblock dentin-post-core complex would enable more uniform distribution of forces along the root, maximize a tooth’s ability to absorb stresses, and minimize the possibility of root fracture. This belief has caused some clinicians to minimize the benefits of coronal coverage and the ferrule effect (Morgano 2015). Costa’s in vitro study (Costa and Pegoraro 1997) evaluated the fracture resistance (strength) of endodontically treated teeth with MOD preparations restored with (1) amalgam restorations, (2) bonded cast inlays, and (3) onlays cemented with zinc phosphate. Fracture resistance proved to be the greatest for group 3 and least for group 1. The need for cuspal coverage of endodontically treated posterior teeth is revealed further in a clinical study in which bonded Empress inlays were evaluated (Stoll et al. 2007). Results of this long-term study revealed a survival rate of 53 % (or 47 % failure rate) after only 23 months, and failures began to surface early in the study. Restoration of endodontically treated teeth with inlays was not recommended. The amount of remaining coronal tooth structure appears to have the most influence on survival rates of endodontically treated teeth. According to Rosenstiel (2016), posterior teeth are subjected to greater occlusal loads than anterior teeth because they are closer to the fulcrum of the jaw (the temporomandibular joint) in what is a Class III lever system. The longest lever arm in a Class III lever has the weakest force, which is why much less force can be applied to an object placed between the central incisors than between molars. Consequently, this fact and the morphology that characterizes posterior teeth (a divided occlusal surface with cusps that can be wedged apart) make them susceptible to fracture, especially during excursive movements when working and/or balancing interferences are present. Endodontically treated posterior teeth should be restored with cuspal coverage to prevent bite forces from causing tooth fracture. Although they are in a minority, endodontically treated premolars or molars with sufficient remaining sound tooth structure should be restored with a cast or bonded all-ceramic restoration with occlusal coverage, such as an MOD onlay. Perhaps the only exceptions are when mandibular premolars and first molars have conservative access preparations and substantial remaining marginal ridge widths of at least 2.0 and 1.6 mm, respectively, and are protected by canine guided occlusion. Endodontically treated maxillary premolars especially are at higher risk for failure, and complete coverage restorations are recommended to protect against fracture.
6.1.2 Rationale for Using Posts to Restore Anterior Teeth
The decision to use a post to restore and endodontically treated tooth should be based on the quantity of remaining coronal tooth structure after removal of all caries and remaining restorative materials and the type of tooth. Traditionally, an endodontically treated tooth received a post to reinforce it and a full- or partial-coverage crown to protect it from occlusal load forces. Retrospective clinical studies have prompted a reevaluation of this strategy (Table 6.2). Similar success rates were uncovered for endodontically treated anterior teeth with and without crowns—87.5 % and 85.4 %, respectively. Lovdahl and Nicholls (1977) found that the mean failure load of endodontically treated maxillary central incisors with intact crowns was approximately 3.6 times greater than those restored with cast gold post-cores. Two in vitro studies revealed that inserting posts in relatively intact endodontically treated anterior teeth does not increase their fracture resistance (Guzy and Nicholls 1979; McDonald et al. 1990). Clearly, endodontically treated anterior teeth do not always require complete coverage with a crown. A crown might be indicated when composite restorations will have a limited prognosis, as in the case of large proximal restorations and unsupported tooth structure. Previous research has demonstrated that endodontic access only in an otherwise intact tooth has only a minimal effect on the strength of the tooth (Steele and Johnson 1999; Reeh et al. 1989b). If the crown structure is largely intact and occlusal loading is favorable, as it often is on an anterior tooth far from the fulcrum (temporomandibular joint), then an endodontically treated anterior tooth with a conservative access preparation may be restored with composite placed in the access cavity. In cases where the crown is nearly intact, the tooth is better served with a conservative, bonded restoration (Fig. 6.1). If tooth devitalization results in discoloration of the crown, and shade change is needed, then bleaching is a better option than crown placement when the tooth is relatively intact (Goerig and Mueninghoff 1983a). When a restoration is necessary, the facial surface of a tooth could be restored less destructively with a porcelain laminate veneer.

Table 6.2
Efficacy of post placement in anterior teeth
|
Studies on anterior teeth endodontically treated
|
No post
|
Post placed
|
Years of survival of tooth after treatment
|
|---|---|---|---|
|
Ross (1980)
|
61 %
|
Nonapplicable
|
5 years or more
|
|
84.7 %
|
89.4 %
|
1–25 years
|

Fig. 6.1
Anterior teeth with intact crowns can be restored with composite restorations in the endodontic access cavity (Reproduced from Rosenstiel et al. (2016))
6.1.3 Quantifying Tooth Loss
The primary purpose of a post is to retain core material that substitutes for missing extensive crown structure resulting from caries, previous restorations, trauma, and/or endodontic access. Often, in these teeth, insufficient axial tooth structure remains after tooth preparation for a full- or partial-coverage definitive restoration. The indication for post placement depends on the degree of coronal tooth destruction in a tooth that is being evaluated for endodontic treatment. Unfortunately, the amount of tooth destruction necessary to justify placing a post has not been defined clearly. An attempt to quantify the extent of destruction was detailed by Peroz et al. (2005). They used a classification that described five categories of crown destruction, based on the number of remaining axial walls. In the Class I category (the most conservative), the endodontic access cavity is surrounded by all four axial walls. Class II describes the typical mesio-occlusal (MO) or disto-occlusal (DO) cavity in which one cavity wall is missing. Class III represents the MOD cavity with two remaining axial walls. In the Class IV category, a single axial wall—either buccal or lingual—remains. Class V depicts the crownless tooth with no remaining axial walls (Figs. 6.2, 6.3, and 6.4). A cavity wall thickness greater than 1.0 mm after tooth preparation should retain core material for a crown and is considered the absolute minimum to resist functional loads (Peroz et al. 2005; Pilo and Tamse 2000). When cusp thickness is less than 1.0 mm, teeth prepared for crowns will lose all remaining axial tooth structure (ferrule) for strength and stability. The ferrule may be defined as a circumferential area of axial dentin superior to the preparation finish line. The design of the ferrule will be discussed further.
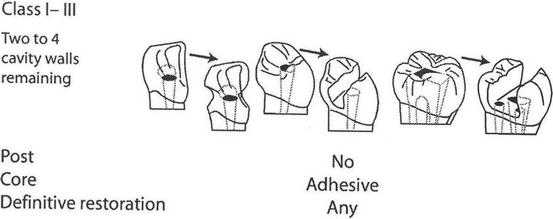
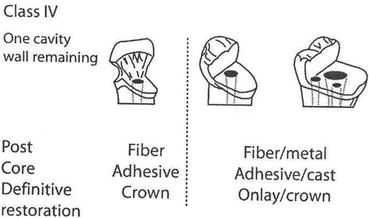
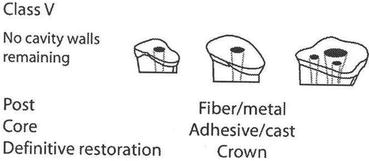
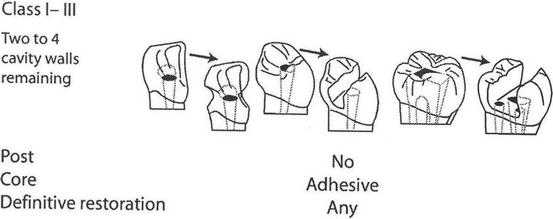
Fig. 6.2
A post is not required when at least two axial walls remain. If axial wall thickness after tooth preparation is >1 mm, a post is not required. When axial wall thickness prior to preparation is <2 mm, it must be considered as missing (Reproduced from Peroz et al. (2005))
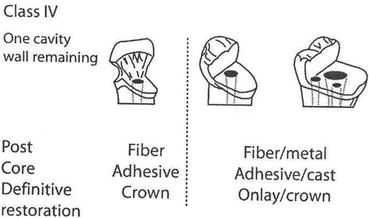
Fig. 6.3
A post is indicated when one cavity wall remains. Fiber posts are used in anterior teeth (metal is used with porcelain-metal crowns); fiber or metal posts are used in posterior teeth. A bonded composite core or cast post-core may be used. Full-coverage crowns should be made for anterior teeth; crowns or onlays are indicated for posterior teeth (Reproduced from Peroz et al. (2005))
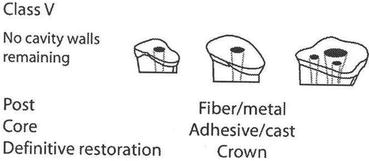
Fig. 6.4
A post (fiber or metal) must be used when no axial walls remain. A ferrule of at least 2 mm is needed to minimize root fracture (Reproduced from Peroz et al. (2005))
According to Peroz et al. (2005), if Class I, II, and III cavity walls have thicknesses greater than 1.0 mm and axial heights of at least 2.0 mm, then a post is not recommended. Most types of definitive restorations may be considered in these situations because remaining coronal tissues provide sufficient surface area for building cores with adhesive systems. Research by Steele and Johnson (1999) compared the fracture resistance (strength) of endodontically treated premolars with conservative MOD cavity preparations and endodontic access preparations. The teeth received either amalgam or composite resin restorations. Their study revealed that the addition of both restorations increased the resistance to fracture, although never approaching the strength of unaltered (control) teeth or teeth with standard endodontic access preparations only. They noted that teeth with access preparations only were more resistant to fracture than MOD preparations. A study by Ausiello et al. (1997), using maxillary premolars, disclosed that the fracture resistance of teeth prepared with conservative MOD preparations and restored with dentin bonding systems and resin composite restorations provided fracture values comparable to intact teeth. Moreover, anterior teeth with Class III cavity preparations do not benefit from post placement (Strub et al. 2001). Vertical root fractures were noted in 28 % of teeth with extensive MOD restorations and without crowns (Testore et al. 1993). Among 468 endodontically treated teeth restored with full-coverage crowns, and which exhibited root fractures, 78 % were premolars, with maxillary premolars comprising 62 %. The maxillary second premolar was most often found to be fractured (Rud and Omnell 1970). It is important that premolar roots have sufficient bulk and that they are sufficiently straight and long prior to restoring with post-cores.
When only one cavity wall remains (as in the Class IV category), the fracture resistance of endodontically treated mandibular molars is not enhanced by core buildups with different materials (Foley et al. 1997). A core buildup restoration must be capable of withstanding the rigors of crown preparation and impression procedures. It must contribute to the retention and support of a provisional restoration in the short term and, in the long term, to the definitive extracoronal restoration. In function—and especially in parafunction—a core buildup transmits axial loads to all remaining tooth structure and contributes to the resistance form and distribution of laterally applied loads. If a Class IV category tooth must serve as an abutment for fixed or removable partial denture (RPD), then crown preparation will further diminish its fracture strength (Burke et al. 2000). When only one cavity wall remains in anterior teeth, it is recommended to use fiber posts with all-ceramic crowns; both metal and nonmetal posts are acceptable options for posterior teeth. In a clinical study (Ferrari et al. 2000), endodontically treated posterior teeth with one remaining coronal wall and a post experienced a restorability success rate of 95 % after 2 years. When posts were omitted, the success rate declined to 30 % over the same period.
6.1.4 Ferrule
When there are no remaining cavity walls (as in the Class V category), a post is needed to secure the core to the root. Also, the post must transfer bite forces to surrounding root structure. The post is most effective when it distributes those forces over the entire wall of the post space to minimize concentration of stresses to any particular area. In extensively damaged crowns, the post provides the definitive crown restoration with retention that would have otherwise been obtained from coronal tooth structure. In the Class V category, the ferrule makes a major contribution toward preserving the fracture resistance of a tooth because it provides the major anchorage for the core. When a crown encircles 1.5–2.0 mm of vertical axial tooth structure (with a minimum horizontal thickness of 1.0 mm) above the finish line, it will help minimize the risk of a root splitting open under stresses generated by the post (Shillingburg et al. 2012).
Endodontically treated posterior teeth with no remaining cavity walls and ferrules less than 2.0 mm showed a success rate of 80 % when posts were inserted. When posts were omitted, the success rate fell to 40 % (Ferrari et al. 2000). In an in vitro study, maxillary central incisors restored with cast post-cores and full-coverage crowns were subjected to cyclical fatigue loads within the range of physiological masticatory loads (Libman and Nicholls 1995). Teeth prepared with 1.0-mm ferrules survived 10 times more cyclical loads before their cement seals fractured at the crown margins than those with 0.5-mm ferrules. Crowns on teeth with 1.5-mm ferrules survived 63 times as many cyclical loads as those with 1.0-mm ferrules. Although most studies concur that ferrules improve fracture resistance and help protect the integrity of the cement seal of the artificial crown, sufficient coronal tooth structure is absent in many instances. A study of endodontically treated incisors by Rendez da Silva et al. (2010) showed that teeth lacking a ferrule that were restored with ceramic crowns exhibited higher fracture resistance than those restored with metal crowns. In fact, the use of ceramic crowns in this study seemed to nearly overcome the problem of lack of ferrule; however, the fracture patterns seen in teeth without ferrules, and restored with ceramic crowns, were more serious compared to teeth restored with metal crowns. In a review of available clinical studies, Dietschi et al. (2008) stated that fatigue studies support conservation of tooth structure and the presence of a circumferential ferrule to optimize tooth biomechanical properties. The studies clearly indicate that resistance to failure of core buildups and natural crown structure increases with the amount of tooth structure remaining. Every attempt should be made to incorporate a ferrule bracing of at least 1.5 mm (optimally 2.0 mm) because with sufficient ferrule, post length and post design features (i.e., parallel sided or tapered) take on a subordinate role (Weine et al. 1991; Assif et al. 1993; Sorensen and Engelman 1990).
Goodacre et al. (2003) reviewed 12 clinical studies, which evaluated almost 3000 posts and cores. A mean complication incidence of 10 % was reported over a time span ranging from 1 to 25 years. Among the most common complications relating to post and cores, post dislodgement accounted for 5 % and root fracture 3 %. The ferrule helps minimize root fracture by encircling tooth structure.
A Ferrule Performs Three Additional Functions
- 1.
Protects the post against fracture
- 2.
Minimizes post dislodgement
- 3.
Protects the cement seal at the margin of the crown
A search of the literature on fracture threshold revealed that if the intaglio surface of the crown apposes 1.5–2.0 mm of ferrule, then the force needed to fracture the tooth is increased. Among the 788 posts studied by Torbjőrner et al. (1995), 5.7 % dislodged from the canal space and 2.7 % failed because of root fracture. All 6 (0.8 %) post fractures were attributed to a lack of ferrule. These findings are in agreement with those of Goodacre et al. (2003). The results of both studies show that if the margin of a crown and the core-tooth interface are at the same cervical level, then all forces of occlusion will be placed on the post that exits the post space; eventually, the post could fatigue and fracture. When a crown rests entirely on core material, occlusal stresses are concentrated on root structure, close to the crown margin. In this scenario, vertical root fracture is more likely. The complete coverage crown with a 2-mm ferrule on sound tooth structure will change the distribution of forces to the root and the post-core complex. A circumferential ferrule helps minimize the chances for damage to the tooth and the post-core complex when they are subjected to occlusal loads (Ree and Schwartz 2010; Morgano et al. 2004). The most important design feature of the tooth preparation to protect it from fracture is likely to be a 360° ferrule, with a minimal vertical height of 1.5–2.0 mm above the finish line (Eissmann and Radke 1976; Schwartz and Robbins 2004) (Fig. 6.5).
Fig. 6.5
Preparation of a ferrule (arrows in a) minimizes fracture of an endodontically treated tooth during function. (b) Preparation of tooth without a ferrule (Reproduced from Rosenstiel et al. (2016))
A classical study by Kaufman et al. (1961) showed that most retention in full-coverage crown preparation designs is derived from the cervical areas of the preparations; therefore, inclusion of a circumferential ferrule provides sound tooth structure in a critical area. When a core is added to increase the axial height of a tooth preparation, it enhances resistance, or the ability of the preparation to prevent dislodgment of the restoration by forces directed in an apical, oblique, or horizontal direction.
6.1.5 Biologic Width and Crown Lengthening
One microleakage study found that with dynamic loading, as the height of the ferrule increases, the potential for leakage into the crown decreases (Libman and Nicholls 1995). Microleakage was observed to progress between the crown margin and finish line, up the ferrule, and then into the tooth-core interface. Leakage patterns that invade the tooth-core junction eventually progress into the post space. Often, if a crown is placed on a tooth that lacks an adequate ferrule, then fracture of the underlying preparation is likely, most probably in the region of the crown margin where stress is greatest and the tooth is thinnest. Perhaps a modification in treatment planning should be considered when a tooth lacks a circumferential ferrule of at least 1.5 mm, especially when the final restoration will be subjected to increased occlusal loads, as a fixed partial denture (FPD) abutment, or an abutment for a distal extension RPD. Increasing ferrule height might be accomplished by preparing the finish line farther apically without invading the biologic width (i.e., the combination of connective tissue attachment and epithelial adhesion to root. Two millimeters is the average minimum space of the biologic width). In general, to avoid biologic width impingement, the minimum distance required from the osseous crest to the final restoration margin is approximately 2.5 mm. Subgingival margin placement should not exceed half the depth of the gingival sulcus (Rosenstiel et al. 2016). If this is not possible for those teeth with severe coronal destruction, then it might be necessary to perform periodontal crown lengthening or orthodontic extrusion to increase ferrule height. The choice between each option should be based on the effect each procedure will have on the esthetic outcome of the case (e.g., gingival margin location and symmetry), the possibility of creating an unfavorable crown-to-root ratio, or uncovering furcations in the tooth and in neighboring teeth as well. When little crown structure remains and the furcation is high, crown lengthening is usually not indicated because the long-term prognosis of the tooth is poor. Extraction is a better alternative than placing a well-executed restoration on a questionable tooth (Faria et al. 2011).
Kovarik et al. (1992) have shown that the type of core material one uses also impacts on the integrity of the cement seal. When teeth were prepared with less than 1.0-mm ferrules (where occlusal forces were shouldered by the post-core materials), and restored with prefabricated posts and flexible composite cores, 83 % of the cores eventually failed. Fifty percent of the failures occurred as a result of failure of the zinc phosphate cement at the crown-core interface, the post-root interface, or both. Forty percent of the failures were the result of fractured posts. Failures were attributed to the flexure of composite cores under dynamic loading, which placed increased shearing stresses at the cement interface, and just below the junction of the post with the core material. In these situations, leakage of a crown is often impossible to detect clinically because the crown will remain on the tooth as long as the post and core are cemented. Although everything appears to be intact, microleakage can occur along the cement crack, and this can result in a radiographically undetectable carious lesion in the structure of the tooth beneath the crown. The core material that held up best in this study was amalgam, although the failure rate was still unacceptably high at 33 %. All core buildups with glass ionomer failed.
Conclusions by Kovarik et al. (1992) Regarding Cores
- 1.
Almost any core material might be acceptable with 2 mm of circumferential vertical dentin that extends coronally from the finish line of the preparation (i.e., the ferrule).
- 2.
When remaining tooth structure is scarce, the choice of core materials is critical.
- 3.
The use of composite resin or reinforced glass ionomer core buildup materials should be avoided when very little axial tooth structure remains.
6.1.6 Restorative Problems Associated with Premolars
Thin roots and radicular fluting (a mesio-proximal invagination of the tooth, near the cemento-enamel junction [CEJ]), characteristic of many maxillary first premolars, can pose a particularly great restorative challenge. When there is little remaining crown structure, crown lengthening or orthodontic eruption might be needed to obtain adequate ferrule. Either procedure could result in uncovering the fluted area or furcation, which could create prosthodontic or periodontal maintenance problems. Another potential problem associated with restoring premolars involves the location and number of posts to be placed. The problem was uncovered in a study that was designed to investigate the point at which cyclic loads, directed at maxillary first premolars, would cause crack propagation in the cement seals of full-coverage crowns cemented over cores maintained with prefabricated and cast posts (Fan et al. 1995). Each tooth in the study was prepared with a 1.0-mm ferrule and received an occlusal load, within a functional range, that was directed to the palatal incline of the buccal cusp. Posts and crowns were cemented with zinc phosphate. When posts—cast and prefabricated stainless steel (with amalgam cores)—were cemented into palatal canals, all specimens exceeded the upper limits of 250,000 cyclic loads without evidence of crack propagation in the cement layer of the crowns. Similar results were observed when two stainless-steel prefabricated posts (with amalgam cores) were cemented. However, when posts were placed in buccal canals only, failure occurred after an average of 164 cyclic loads. The authors recommended placing two posts when restoring endodontically treated and structurally compromised premolars to ensure protection from occlusal forces from either the buccal or palatal/lingual directions. Cracks in the cement seal are impossible to detect clinically; therefore, the choice of post location could have a profound effect on the survival of a restoration. When teeth with full-coverage crowns experience preliminary failure (i.e., cracks in the luting cement caused by cyclic loading), leakage of microbes could progress to the coronal level of the gutta-percha and compromise the root canal seals (Freeman et al. 1998). Gutta-percha does not present an effective barrier to leakage down the canal space. The evidence presented highlights the importance of adequate ferrule height for teeth being considered for full-coverage restorations and the need for crown lengthening or orthodontic eruption when there is minimal coronal tooth structure available to design a ferrule.
While some groups of teeth will not require a post in many clinical situations, Sadan (2002) recommended placing post-cores in the majority of premolars that must be restored with full-coverage crowns. His concerns were based on their relatively narrow diameter at the CEJ and their relatively wide buccolingual dimension at the height of contour—i.e., many premolars have “narrow waists” and “broad shoulders.” Current design parameters for finish lines for full-coverage crowns advocate deep chamfer or shoulder widths in the range of 0.9–1.2 mm for maximum esthetics in porcelain (Rosenstiel et al. 2016). With this in mind, when an endodontically treated premolar is prepared for a full-coverage crown and a deep finish line is prepared, a significant quantity of crown structure will be eliminated at the height of contour before the chamfer or shoulder can be fashioned, even when the prepared tooth is tapered minimally (6–10°), which is not likely on many posterior teeth. Often, what remains is a tooth preparation with very thin axial wall structure. The crown of the tooth is further compromised structurally as additional dentin is removed from inside the crown to create an access preparation for endodontic treatment. The resultant tooth preparation often contains paper thin axial walls or areas that lack axial dentin. It must be remembered that in function, complete coverage crowns distribute stresses over axial dentin, transfer loads to the post-core, and provide the ferrule effect to minimize root fracture. When a crack propagates within the luting cement, any resisting force provided by the cement is increasingly transferred to the post. Eventually, the post could become the last remaining structure to resist applied loads, which could result ultimately in catastrophic failure of the restoration.
Older retrospective studies often failed to specify whether a ferrule was present in the teeth that were tested. Conversely, the concept of a ferrule and its importance to the survival of restorations is addressed in some newer prospective studies. For example, a study by Ellner et al. (2003) examined fifty single-rooted teeth in need of single full-coverage crowns. Especially meaningful was the fact that the study evaluated four different post-core systems over a period of up to 10 years. All teeth had a ferrule at least 2.0 mm in height. The following post-core systems were evaluated: system 1, conventional tapered post-cores cast in gold alloy; system 2, prefabricated gold ParaPosts and cast gold cores; system 3, the ParaPost system (using burnout patterns) with cast gold post-cores; and system 4, Radix Anchor-threaded titanium posts with resin cores. Teeth receiving Radix Anchor posts were excluded from the randomization process as the shape of the core sections was too large and could not be used to restore teeth. The overall failure rate for all four groups was 6 %. When the Radix Anchor posts were excluded, the failure rate diminished to 3 % over the 10-year period, which represented a very good success rate. In the literature, threaded posts are associated with greater failure rates (Mentink et al. 1993). A meta-analysis of ten in vitro and six in vivo studies revealed no significant difference in the performances of direct and cast post-cores (Heydecke and Peters 2002). Also, no statistically significant differences were found between prefabricated (direct) and cast post-core systems that would justify recommending one over the other (Reagan et al. 1999).
In a prospective study by Creugers et al. (2005), in which the follow-up rate was 5 years, 319 teeth were studied to determine whether (1) the survival rate of cast post-core restorations was greater than the survival of direct metal post and resin core restorations and post-free (all-composite) restorations; and (2) the survival rate of the buildup restoration was influenced by the length of the ferrule in teeth restored with full-coverage crowns. Two hundred one prepared teeth contained a collar of dentin sufficient in height for a classical ferrule; 118 teeth contained a minimal collar of dentin—not sufficient for a classical ferrule. Restorations made on teeth with sufficient ferrule had a 98 % survival rate; restorations made on teeth with a minimal collar of dentin had a survival rate of 93 %. Post-core restorations fabricated for teeth with a sufficient ferrule performed significantly better than those placed on teeth that lacked sufficient ferrule. The evidence is compelling that ferrule height is more important to the survival of the restoration than the design of the core buildup.
A prospective study from the endodontic literature compared the survival rates of endodontically treated teeth restored by different post-core systems and compared them to endodontically treated teeth without post-core restorations (Salvi et al. 2007). Restored teeth served as abutments for single metal-ceramic crowns, composite crowns, or FPDs. Post-cores were omitted only in teeth in which approximately two-thirds of the remaining clinical crown structure was still available. A dentin ferrule was incorporated in all tooth preparations. Although it was not specifically stated by the authors, it is assumed that a substantial ferrule (1.5–2.0 mm) characterized all preparations. After 5 years, success rates for teeth restored with prefabricated titanium posts, cast post-cores, and teeth without posts amounted to 93 %, 97 %, and 94 %, respectively. The high rates of success attest to the importance of the dentin ferrule in increasing tooth fracture resistance. When uniform and nonuniform ferrule heights were incorporated into the designs of full-coverage crown preparations of maxillary central incisors that were restored with cast post-cores and crowns, Tan et al. (2005) found that teeth with nonuniform ferrules (0.5–2.0 mm vertical height) withstood 27 % fewer static loads than those with uniform (2.0 mm) ferrules. Teeth that lacked ferrules withstood 55 % fewer static loads than teeth with uniform ferrules. Based on the magnitude of forces at which the teeth fractured, it was concluded that teeth without a ferrule are at risk of fracture when subjected to maximal clenching forces, whereas teeth with nonuniform ferrules could resist forces from maximal clenching.
6.1.7 Fiber-Reinforced Posts
Various post systems have been used to restore endodontically treated teeth in many different clinical situations (Sorensen and Martinoff 1984a; Fraiman 2010). The first composite reinforced fiber post systems were made with carbon fibers arranged longitudinally in an epoxy resin. The potential disadvantage of carbon fiber posts is their black color, which could transmit through all-ceramic crowns, especially those made for anterior teeth. Black fibers were replaced subsequently by more esthetic white or translucent glass and quartz fibers, which have become standard components of fiber posts; they are the better choice for cases with greater esthetic demands. The manufacturers of these posts claim that as they will flex with dentin under occlusal loading, they will distribute forces and guard against tooth fracture. As mentioned previously, this has caused some clinicians to believe that the classic concept of a ferrule is not applicable when fiber posts are used. In fact, the use of posts has been associated with fractures of teeth; this occurs in many more teeth with posts than without. With this in mind, it should be remembered that the purpose of the post is to retain the core while minimizing the risk for tooth fracture. A 3-year prospective clinical study by Mancebo et al. (2010) that evaluated the survival of fiber posts where more than one-quarter of the teeth are restored with fiber posts, but without ferrules, failed after 3 years (Table 6.3). When Soares et al. (2008a) subjected endodontically treated teeth with major loss of crown structure (i.e., MOD cavity preparation +  loss of occluso-cervical (O-C) cusp height + composite resin restoration and MOD cavity preparation +
loss of occluso-cervical (O-C) cusp height + composite resin restoration and MOD cavity preparation +  loss of O-C cusp height + glass fiber post + composite resin restoration) to compression loads at 30°, their fracture resistance decreased. Adding a glass fiber post to these teeth did not restore the fracture resistance significantly. However, inserting a fiber post in teeth exhibiting minor structural loss significantly reduced their fracture resistance. Although posts did not reinforce endodontically treated teeth, they were found to reduce catastrophic root fractures in teeth with major loss of crown structure. Endodontically treated teeth with MOD cavity preparations, two-thirds loss of O-C cusp height and composite resin restorations suffered 80 % catastrophic root fractures, whereas inserting a fiber post reduced catastrophic fractures to 40 %. Obviously, the use of fiber posts in this situation promoted more favorable fracture patterns that were considered retreatable. Their results seem to reinforce the main function of posts in endodontically treated teeth with major crown structure loss—retention of restorative core material and not reinforcement of the dental unit. Despite the loss of fracture resistance in teeth with major loss of crown structure, studies show that the combination of a fiber (glass or quartz) post with an adhesive restoration created a higher incidence of rerestorable failure types (Soares et al. 2008a; Akkayan and Gülmez 2002; McLaren et al. 2009; Zhi-Yue and Yu-Xing 2003). It appears that when a post is needed to retain a foundation restoration (core), the best option is a fiber-reinforced post with physical properties that resemble natural dentin, bonded to tooth structure (Dietschi et al. 2008).
loss of O-C cusp height + glass fiber post + composite resin restoration) to compression loads at 30°, their fracture resistance decreased. Adding a glass fiber post to these teeth did not restore the fracture resistance significantly. However, inserting a fiber post in teeth exhibiting minor structural loss significantly reduced their fracture resistance. Although posts did not reinforce endodontically treated teeth, they were found to reduce catastrophic root fractures in teeth with major loss of crown structure. Endodontically treated teeth with MOD cavity preparations, two-thirds loss of O-C cusp height and composite resin restorations suffered 80 % catastrophic root fractures, whereas inserting a fiber post reduced catastrophic fractures to 40 %. Obviously, the use of fiber posts in this situation promoted more favorable fracture patterns that were considered retreatable. Their results seem to reinforce the main function of posts in endodontically treated teeth with major crown structure loss—retention of restorative core material and not reinforcement of the dental unit. Despite the loss of fracture resistance in teeth with major loss of crown structure, studies show that the combination of a fiber (glass or quartz) post with an adhesive restoration created a higher incidence of rerestorable failure types (Soares et al. 2008a; Akkayan and Gülmez 2002; McLaren et al. 2009; Zhi-Yue and Yu-Xing 2003). It appears that when a post is needed to retain a foundation restoration (core), the best option is a fiber-reinforced post with physical properties that resemble natural dentin, bonded to tooth structure (Dietschi et al. 2008).
 loss of occluso-cervical (O-C) cusp height + composite resin restoration and MOD cavity preparation +
loss of occluso-cervical (O-C) cusp height + composite resin restoration and MOD cavity preparation +  loss of O-C cusp height + glass fiber post + composite resin restoration) to compression loads at 30°, their fracture resistance decreased. Adding a glass fiber post to these teeth did not restore the fracture resistance significantly. However, inserting a fiber post in teeth exhibiting minor structural loss significantly reduced their fracture resistance. Although posts did not reinforce endodontically treated teeth, they were found to reduce catastrophic root fractures in teeth with major loss of crown structure. Endodontically treated teeth with MOD cavity preparations, two-thirds loss of O-C cusp height and composite resin restorations suffered 80 % catastrophic root fractures, whereas inserting a fiber post reduced catastrophic fractures to 40 %. Obviously, the use of fiber posts in this situation promoted more favorable fracture patterns that were considered retreatable. Their results seem to reinforce the main function of posts in endodontically treated teeth with major crown structure loss—retention of restorative core material and not reinforcement of the dental unit. Despite the loss of fracture resistance in teeth with major loss of crown structure, studies show that the combination of a fiber (glass or quartz) post with an adhesive restoration created a higher incidence of rerestorable failure types (Soares et al. 2008a; Akkayan and Gülmez 2002; McLaren et al. 2009; Zhi-Yue and Yu-Xing 2003). It appears that when a post is needed to retain a foundation restoration (core), the best option is a fiber-reinforced post with physical properties that resemble natural dentin, bonded to tooth structure (Dietschi et al. 2008).
loss of O-C cusp height + glass fiber post + composite resin restoration) to compression loads at 30°, their fracture resistance decreased. Adding a glass fiber post to these teeth did not restore the fracture resistance significantly. However, inserting a fiber post in teeth exhibiting minor structural loss significantly reduced their fracture resistance. Although posts did not reinforce endodontically treated teeth, they were found to reduce catastrophic root fractures in teeth with major loss of crown structure. Endodontically treated teeth with MOD cavity preparations, two-thirds loss of O-C cusp height and composite resin restorations suffered 80 % catastrophic root fractures, whereas inserting a fiber post reduced catastrophic fractures to 40 %. Obviously, the use of fiber posts in this situation promoted more favorable fracture patterns that were considered retreatable. Their results seem to reinforce the main function of posts in endodontically treated teeth with major crown structure loss—retention of restorative core material and not reinforcement of the dental unit. Despite the loss of fracture resistance in teeth with major loss of crown structure, studies show that the combination of a fiber (glass or quartz) post with an adhesive restoration created a higher incidence of rerestorable failure types (Soares et al. 2008a; Akkayan and Gülmez 2002; McLaren et al. 2009; Zhi-Yue and Yu-Xing 2003). It appears that when a post is needed to retain a foundation restoration (core), the best option is a fiber-reinforced post with physical properties that resemble natural dentin, bonded to tooth structure (Dietschi et al. 2008).
Table 6.3
Clinical results of study done by Mancebo et al. (2010) on survival rate of fiber-reinforced posts
|
3-year study of teeth with fiber posts cemented with Rely-X
|
45 teeth with ferrule of at least 2 mm
|
42 teeth without ferrule
|
|---|---|---|
|
1. Teeth restored with metal-ceramic crowns or ceramic crowns
2. Not used as a part of an FPD or RPD
|
6.7 % failure
|
26.2 % failure
|
6.1.8 Ceramic Posts
Ceramic posts are made of zirconium oxide. They are weaker than metal posts; therefore, a thicker post is necessary, which might require removal of additional root dentin. Theoretically, an intact root should permit retreatment of a tooth. However, removal of zirconia posts cemented in canal spaces with adhesive cements—normally a tedious and risky process—is not always successful. Retrieval of cemented zirconia posts often results in tooth fractures or removal of considerable remaining dentin, which might result in a nonrestorable outcome. A metallic post could produce a gray discoloration in translucent, all-ceramic crowns and in the adjacent gingiva of a patient with a thin periodontal biotype. Ceramic posts were designed originally to be used with composite resin cores for all-ceramic crowns, primarily for esthetic purposes. Research by Butz et al. (2001) on survival rate and fracture strength of endodontically treated teeth restored with four different post-core materials revealed that zirconia posts with composite cores had the lowest survival rates (63 %). When natural central incisors were restored with zirconia posts (with cores made of either composite or heat-pressed ceramic) and full-coverage cast metal crowns, and the crowns were subjected to 30 N forces (well within the normal clinical range), all zirconia posts fractured. However, tooth fractures in both groups rarely extended below the crown margin. Restoration of endodontically treated teeth with zirconia post-cores resulted in fewer vertical root fractures than prefabricated metal posts with composite cores or cast metal post-cores.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


