An impacted mandibular first molar tends to cause serious bone defects of the adjacent teeth. When choosing between the 2 typical treatment options—extraction or orthodontic relocation of the impacted tooth—the decision should be based on assessment of the prognosis. A 22-year-old man with severe mesioangulation and impaction of the mandibular first molar and a related vertical bone defect on the distal side of the second premolar was treated with extraction of the second molar and orthodontic relocation of the first molar with a retromolar miniscrew. Comprehensive orthodontic treatment involving premolar extraction was conducted. Strategic extraction of the molar and adequate orthodontic movement helped to restore the bone structure on the affected side. This case report suggests the effectiveness of restoration of bone defects by using viable periodontal tissues around the impacted tooth for the longevity of the periodontium.
Highlights
- •
Alveolar bone defect has to be assessed before making an extraction decision.
- •
Orthodontic eruption can recover an infrabony defect caused by an impacted tooth.
- •
A miniscrew is a valuable tool for therapeutic diagnosis of possible ankylosis.
Impaction of permanent teeth is frequently found in adult patients. The prevalence of impaction of permanent molars excluding the third molar has been reported to be 1.8% to 9.2%. Ectopic eruption of the mandibular first molar, however, is relatively rare, with prevalence rates of 0.01% to 0.36%. One major etiologic factor was the mesioangular eruption path of the mandibular first molar for an unknown reason. Eruption failure of mandibular posterior teeth, once it occurs, leads to complicated clinical consequences including tipping of the adjacent teeth, space loss in the dental arch, supraeruption of opposing teeth, and reduced alveolar bone height, which may necessitate not only correction of the impacted tooth but also reconstruction of the overall dentition. Early detection of the impaction may be the key to prevention of those events. Impacted teeth in adults may well have caused the majority of the complications.
There are 2 conventional treatment options for impacted teeth in adults: extraction or orthodontic relocation. Extraction is often preferred in adults mainly because of the possibility of ankylosis and the prolonged treatment time. In contrast, extraction of a severely impacted molar tends to leave a serious periodontal defect at the adjacent tooth, particularly when the impacted tooth is mesially angulated. On the other hand, orthodontic relocation of the impacted tooth may benefit the surrounding structure by bringing the bone along as the tooth erupts. Therefore, the uncertainty of the prognosis, the risk of tooth ankylosis, and the possible periodontal defect after the extraction should be comprehensively evaluated before making the decision.
In this case report, we present an adult patient with a severely mesioangulated impaction of the mandibular first molar who was treated with orthodontic traction to induce alveolar bone formation at the bone defect of the adjacent second premolar.
Diagnosis and etiology
A 22-year-old man was referred to the orthodontic department of Yonsei University in Seoul, South Korea, for treatment of an impacted mandibular right first molar. His facial photographs showed a slightly convex profile with mild lip protrusion, and the maxillary and mandibular midlines were deviated 1 and 3 mm, respectively, to the right side relative to the facial midline, with no notable facial asymmetry. The intraoral examination showed Class I canine and molar relationships on the left side and a Class II canine relationship on the right side. Maxillary and mandibular arch-length discrepancies were 5.5 and 1 mm, respectively, and overjet and overbite were 3.5 and 2.0 mm, respectively ( Figs 1 and 2 ).
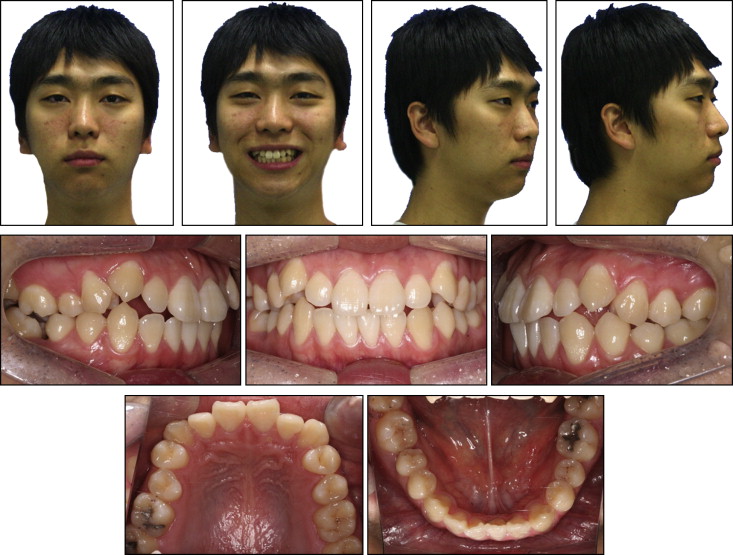

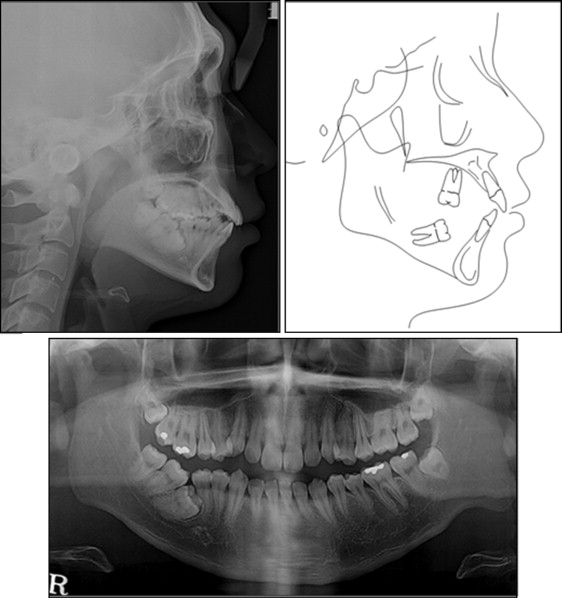
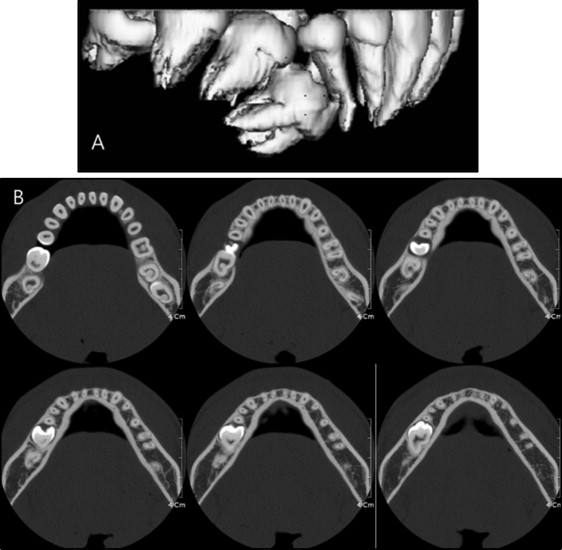
The panoramic radiograph showed a severely mesioangulated and impacted mandibular right first molar and a mesially tilted second molar into the first molar space. The mandibular right third molar was fully erupted with normal size and shape, but the other third molars were impacted ( Fig 3 ). Three-dimensional computed tomography images confirmed the impacted first molar without visible evidence of ankylosis and notable bone defect at the distal side of the second premolar ( Fig 4 ). The cephalometric analysis demonstrated a skeletal Class I jaw relationship (ANB angle, 4.3°; Wits appraisal, −4.4 mm) with a hyperdivergent facial profile (SN-MP angle, 43.1°), linguoversion of the maxillary incisors (U1-SN angle, 93.2°), and labioversion of the mandibular incisors (IMPA, 100.7°) ( Fig 3 , Table ).
| Measurement | Pretreatment | Posttreatment |
|---|---|---|
| SNA (°) | 74.0 | 73.9 |
| SNB (°) | 69.7 | 69.6 |
| ANB (°) | 4.3 | 4.3 |
| Wits appraisal (mm) | −4.4 | −4.7 |
| Mandibular body length (mm) | 85.9 | 85.9 |
| SN-GoMe (°) | 43.1 | 42.9 |
| Björk sum (°) | 403.1 | 402.9 |
| SN-occlusal plane (°) | 30.6 | 31.1 |
| U1 to facial plane (mm) | 14.2 | 11.8 |
| L1 to facial plane (mm) | 10.9 | 8.1 |
| U1 to SN (°) | 93.2 | 92.8 |
| IMPA (°) | 100.7 | 98.1 |
| Upper lip to Ricketts’ E-line (mm) | 1.9 | −0.9 |
| Lower lip to Ricketts’ E-line (mm) | 2.9 | −0.4 |
Based on these findings, this patient was diagnosed as having a skeletal Class I malocclusion with an impacted mandibular right first molar, crowding, and midline deviations.
Treatment objectives
The treatment objectives were to (1) establish proper occlusion in the right posterior segment, (2) restore the bone defect distal to the mandibular right second premolar, (3) relieve the crowding, (4) correct the maxillary and mandibular dental midlines, (5) obtain proper inclination of the maxillary and mandibular incisors, and (6) improve the soft tissue profile by resolving the lip protrusion.
Treatment objectives
The treatment objectives were to (1) establish proper occlusion in the right posterior segment, (2) restore the bone defect distal to the mandibular right second premolar, (3) relieve the crowding, (4) correct the maxillary and mandibular dental midlines, (5) obtain proper inclination of the maxillary and mandibular incisors, and (6) improve the soft tissue profile by resolving the lip protrusion.
Treatment alternatives
To relieve the crowding of the teeth, correct the dental midlines, and improve lip protrusion, the maxillary first premolars and the mandibular left first premolar were extracted, resulting in a Class I molar relationship on the left side and a Class II molar relationship on the right side after treatment.
With regard to the impacted tooth, there were 3 options about the choice of teeth to be extracted. The first option was to extract the impacted first molar and protract the second and third molars with root movement. This option would simply eliminate the need for orthodontic traction of the impacted tooth, but the extraction would immediately leave a severe bone defect distal to the second premolar, compromising the periodontal health. Since the bone defect was confined to the distal side of the second premolar rather than the mesial side of the second molar, mesial root movement of the second molar would not be promising for restoration of the bone in that area. Moreover, mesial root movement of 2 molars requires not only precise control of the force system including anchorage control, but also a long orthodontic treatment.
The second and third options were to extract the second and third molars, respectively, to provide space for repositioning of the impacted tooth. Extraction of the second molar was considered a better option because it could minimize the required tooth movement and allow immediate traction of the impacted tooth. Traction of the impacted tooth, either orthodontically or surgically, would resolve the bone defect distal to the second premolar because bone formation follows the eruption of the tooth. On the other hand, there was the possibility that the first molar was ankylosed and would not respond to the orthodontic force. Unfortunately, clinical and radiographic examinations cannot be used to rule out ankylosis. However, Varpio and Wellfelt reported that unlike vertical impactions that are frequently associated with ankylosis, mesioangulated and distoangulated impactions are mostly caused by lack of space. It was also reported that a mesioangulated impaction could be treated most successfully, whereas distoangulated and vertical impactions tended to resist treatment. Therefore, considering the eruption path of the impacted tooth and the lack of space, a mechanically disturbed eruption was more likely, which would respond positively to an orthodontic force.
Repositioning of the impacted first molar can be performed either surgically or orthodontically. There have been reports and clinical guidelines on the successful surgical uprighting and repositioning of impacted mandibular second molars. This patient was not a good candidate for surgical repositioning, however, because the root apex was completely mature, and the required movement of the apex was considerable, increasing the risk of devitalization.
Consequently, extraction of the second molar followed by orthodontic traction of the impacted tooth was chosen as the treatment plan with special attention to restoration of the bone defect.
Treatment progress
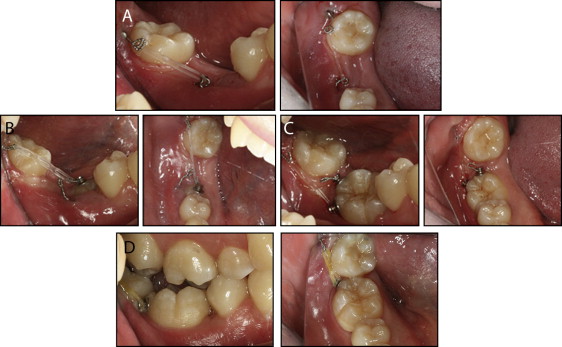
The orthodontic treatment was divided into the first phase, orthodontic traction of the impacted tooth, and the second phase, comprehensive treatment with extraction of 3 premolars, since the prognosis of the impacted first molar was uncertain. The patient was referred to an oral surgeon for extraction of the mandibular right second molar and surgical exposure of the impacted first molar. At the surgery, a metal button with a wire extension was bonded to the first molar for traction, and a miniscrew (7.0 mm length and 1.8 mm diameter; OrlusR; Ortholution, Seoul, Korea) was placed on the right retromolar pad area to provide a single orthodontic force to the first molar. Before bonding on the exposed area of the first molar, clinical percussion did not produce a metallic sound ( Fig 5 , A ).