Introduction
Our objective was to determine whether total posttreatment mandibular rotation is associated with mandibular incisor crowding after retention.
Methods
Mandibular incisor irregularity (II) at least 10 years out of retention (T3) measured on dental casts from the postretention database at the University of Washington in Seattle was used to define subjects (II ≥6 mm, relapse group) and controls (II ≤3.5 mm, stable group). After matching patients and controls for the pretreatment II, the relapse group consisted of 33 subjects (17 boys, 16 girls; age at the end of treatment [T2], 15.0 years; follow-up, 16.8 years), and the stable group comprised 36 subjects (11 boys, 25 girls; age at T2, 16.0 years; follow-up, 15.1 years). On cephalograms taken at T2 and T3, facial morphology was evaluated, and total posttreatment mandibular rotation was measured with a structural method. Logistic regression analyses were used to determine the association between relapse and amount of total mandibular rotation. The models were adjusted for potentially confounding variables (age at T2, sex, length of follow-up, and intercanine width change during treatment).
Results
No association between total posttreatment mandibular rotation and relapse was found ( P = 0.515). Total mandibular rotations were comparable in the relapse and stable groups ( P = 0.386). Age at T2 was found to be correlated with long-term incisor stability ( P = 0.030). Sex and intercanine width change during treatment were not related to relapse ( P = 0.225 and P = 0.264, respectively).
Conclusions
Total mandibular rotation is not associated with relapse of the mandibular incisors. Posttreatment skeletal and dental growth changes were comparable in the relapse and stable groups.
The stability of the results of orthodontic treatment is an important clinical issue. Incisor malalignment after retainer wear stops is a particular concern because of the esthetic consequences associated with it. Not all patients are affected by this relapse, and some are more than others. Several studies have attempted to determine what factors predict which patients are most prone to relapse. Characteristics ranging from type of orthodontic treatment (extraction or nonextraction ) and quality of the orthodontic treatment results to inherent patient components (age, sex, tooth size, and initial crowding) have all been extensively evaluated. Only a few predictors have been found so far; unfortunately, they are weak at best.
One aspect that might contribute to crowding of the mandibular incisors after treatment is the continued craniofacial growth. Most patients finish treatment during the late adolescence, and some amount, albeit small, of craniofacial growth can still be expected. Most changes are in the vertical direction. If vertical growth changes have a rotational component, this can impact interincisal relationships and could influence mandibular incisor alignment. In addition, mandibular rotation (steepness of the mandibular plane angle) is correlated with mandibular arch width; this would also impact mandibular incisor malalignment. Although these effects could be envisioned in patients with extreme mandibular rotation, it is unclear whether this would also affect those with mild rotations.
The purpose of this case-control study was to determine whether posttreatment mandibular rotation is a risk factor for mandibular incisor crowding after retention.
Material and methods
A sample of subjects from various studies on long-term incisor stability after orthodontic treatment was used in this investigation. A detailed description of the methodology is reported elsewhere. The postretention collection in the Department of Orthodontics at the University of Washington in Seattle was screened, and the incisor irregularity (II) index was measured on study models taken at least 10 years out of retention (T3). Depending on the value of the II index, 2 groups were established: relapse (subjects) with II ≥6 mm and stable (controls) with II ≤3 mm.
Patient information and treatment history for all subjects were obtained from the database. Sex, Angle classification, date of birth, dates of end of treatment (T2) and follow-up (T3) records, and treatment alternative (extraction vs nonextraction) were recorded. Length of follow-up time was calculated by subtracting the T2 date from the T3 date. These data allowed matching the relapse and stable groups regarding treatment alternatives, length of follow-up, and II at pretreatment (T1).
The II was measured as the sum of the linear displacements of the anatomic contact points of each mandibular incisor from the adjacent tooth’s anatomic point on the models taken at T1, T2, and T3. Intercanine width was measured as the distance between the cusp tips of the mandibular canines on the T1 and T2 models. The measurements were made to the nearest 0.1 mm by using digital calipers.
After identifying nasion (N), sella (S), point A (A), point B (B), gonion (Go), menton (Me), gnathion (Gn), anterior nasal spine (ANS), posterior nasal spine (PNS), incisal edge and apex of the upper incisor (U1e and U1a, respectively), and incisal edge and apex of the lower incisor (L1e and L1a, respectively) on the cephalograms taken at T2 and T3, we made 10 angular and 5 linear measurements ( Fig ). Overbite (OB) was measured as the distance between U1e and L1e along the vertical plane; overjet (OJ) was measured as the distance between L1e and the maxillary incisor along the horizontal plane (eg, OJ = 0 mm meant that the maxillary incisors contacted the mandibular incisors; OJ = 1 mm meant that there was a 1-mm gap between the maxillary and mandibular incisors). Additionally, 2 ratios were calculated: % of nasal height (N-PP/N-Me ∗ 100%) and posterior to anterior facial height (SGo/NMe ∗ 100%).
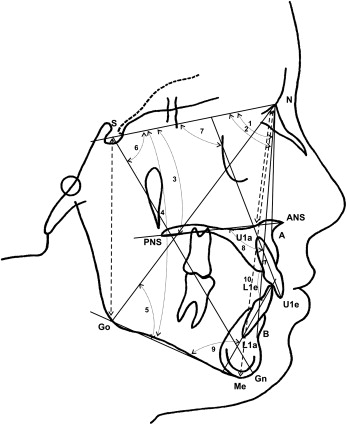
To evaluate the amount of total posttreatment mandibular rotation, the internal structure of mandibular symphysis, the mandibular canal, sella, and nasion were identified on the cephalograms taken at T2 and T3 and traced on acetate paper. After superimposition of the T2 and T3 tracings on the internal structure of the symphysis and the mandibular canal, the total mandibular rotation was calculated as the angle between the SN lines at T2 and T3. The angle was negative in anterior (counterclockwise) and positive in posterior (clockwise) total mandibular rotations. All measurements were made to the nearest half millimeter or degree.
Forty randomly selected cephalograms and 20 study models were reexamined 2 weeks later. Dahlberg’s method was used to assess random error, and paired t tests were used to evaluate the systematic error of the method.
Statistical analysis
Descriptive statistics (means and standard deviations) were computed for each measurement. T tests were performed to test the differences in measurements between the relapse and stable groups at T1, T2, and T3.
The association between relapse and total mandibular rotation was evaluated by calculating the odds ratio (OR) of relapse to stability with logistic regression analysis. Adjustments were made for confounding variables, such as II at T1, intercanine width change during treatment (T1-T2), age at T2, and length of follow-up.
Results
Characteristics of the groups are shown in Tables I and II . Subjects with stable incisor alignment were on average 1 year older at T2 and had a shorter follow-up than the relapsed subjects. However, the differences were not statistically significant. The distribution of the Angle Class I and Class II subjects was balanced in the stable group; in the relapse group, most subjects had Class II malocclusions. The II at T1 was comparable in both groups ( P = 0.163). The II at T2 in the relapse group was greater by 0.85 mm than in the stable group ( P <0.000). Intercanine width change during treatment (T1-T2) was comparable in both groups ( P = 0.284).
| Age (y) | Length of follow-up (y) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjects (n) | T2 | T3 | T2-T3 | Angle class (n) | Treatment type (n) | |||||||||
| Boys | Girls | Total | Mean | SD | Mean | SD | Mean | SD | I | II | III | Nonextraction | Extraction | |
| Relapse | 17 | 16 | 33 | 15.0 | 1.7 | 31.8 | 5.7 | 16.8 | 5.8 | 13 | 20 | 0 | 10 | 23 |
| Stable | 11 | 25 | 36 | 16.0 | 2.5 | 31.1 | 5.3 | 15.1 | 4.5 | 17 | 18 | 1 | 15 | 21 |
| P | 0.007 | 0.055 | 0.620 | 0.182 | — | — | — | — | — | |||||
| II index | Change in intercanine width | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 to T2 | |||||
| Group | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Relapse | 5.21 | 2.60 | 1.61 | 0.90 | 7.75 | 1.15 | 1.11 | 1.48 |
| Stable | 4.16 | 1.53 | 0.76 | 0.52 | 1.87 | 1.12 | 0.70 | 1.53 |
| P | 0.163 | 0.000 | 0.000 | 0.284 | ||||
Measurement errors are shown in Table III . Random errors for angular measurements ranged from 1.14° for total mandibular rotation to 3.08° for the interincisal angle; errors for linear measurements were from 0.19 mm for intercanine width to 0.62 mm for OB. No systematic measurement error was found.
| Variable | Random error | Systematic error ( P value) |
|---|---|---|
| SNA (°) | 1.47 | 0.194 |
| SNB (°) | 1.15 | 0.540 |
| SN/MP (°) | 1.39 | 0.364 |
| Y-axis (°) | 1.94 | 0.080 |
| SN/PP (°) | 1.84 | 0.619 |
| % of nasal height (°) | 1.68 | 0.583 |
| NGo/MP (°) | 1.56 | 0.171 |
| SGo/NMe ∗ 100% | 2.49 | 0.515 |
| OB (mm) | 0.62 | 0.162 |
| OJ (mm) | 0.56 | 0.125 |
| U1/PP (°) | 2.79 | 0.103 |
| U1/SN (°) | 2.31 | 0.016 |
| L1/MP (°) | 2.10 | 0.766 |
| U1/L1 (°) | 3.08 | 0.557 |
| Total mandibular rotation (°) | 1.44 | 0.216 |
| Incisor irregularity (mm) | 0.38 | 0.458 |
| Intercanine width (mm) | 0.19 | 0.762 |
Total mandibular rotation relative to the anterior cranial base in the relapse and stable groups was similar ( P = 0.386, Table IV ). On average, anterior (counterclockwise) rotational changes were seen in both groups. However, 7 subjects from the relapse group (21.2%) and 7 from the stable group (19.4%) had posterior (clockwise) total mandibular rotations.
| Total mandibular rotation from T2 to T3 (°) | ||
|---|---|---|
| Mean | SD | |
| Relapse | −2.32 | 4.30 |
| Stable | −1.51 | 3.26 |
| P | 0.386 | |
Most angular skeletal variables ( Table V ) showed few posttreatment changes, not exceeding 1°, in subjects with unstable and stable incisor alignment. Only the mandibular plane rotated by more than 1° relative to the cranial base (SN/MP angle) in the relapse and stable groups (–1.72° and –1.40°, respectively). An increase of the ratio of SGo/NMe ∗ 100% suggested that rotational changes occurred from growth of the posterior face (SGo) rather than a decrease of the anterior face (NMe). Also, small posttreatment changes of the nasion-sella-gnathion angle implied that anterior facial height in both groups was stable. All posttreatment skeletal changes were comparable in the relapse and stable groups ( P >0.05).
| Relapse | Stable | Relapse vs Stable | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T2 | T3 | Difference | T2 | T3 | Difference | T2 | T3 | T2 to T3 | |||||||
| Mean | SD | Mean | SD | P | Mean | SD | Mean | SD | P | P | P | P | |||
| SNA (°) | 79.52 | 3.99 | 79.98 | 4.4 | 0.46 | 0.170 | 82.17 | 4.54 | 81.64 | 4.54 | −0.53 | 0.154 | 0.012 | 0.130 | 0.051 |
| SNB (°) | 76.22 | 3.93 | 76.79 | 4.59 | 0.57 | 0.100 | 79.18 | 4.20 | 78.96 | 4.09 | −0.22 | 0.421 | 0.006 | 0.042 | 0.115 |
| SN/PP (°) | 7.33 | 4.06 | 7.76 | 4.28 | 0.43 | 0.364 | 7.48 | 4.02 | 7.78 | 3.93 | 0.30 | 0.074 | 0.764 | 0.984 | 0.479 |
| SN/MP (°) | 36.3 | 6.68 | 34.58 | 8.44 | −1.72 | 0.009 | 32.60 | 5.79 | 31.20 | 6.78 | −1.40 | 0.002 | 0.016 | 0.053 | 0.939 |
| NGo/MP (°) | 77.95 | 5.4 | 76.50 | 6.42 | −1.45 | 0.004 | 74.69 | 4.67 | 74.37 | 6.11 | −0.32 | 0.069 | 0.009 | 0.166 | 0.172 |
| NSGn (°) | 68.39 | 4.23 | 68.03 | 5.18 | −0.36 | 0.300 | 65.83 | 3.33 | 65.90 | 4.37 | 0.07 | 0.725 | 0.007 | 0.071 | 0.307 |
| % of nasal height (%) | 44.58 | 3.31 | 44.80 | 3.4 | 0.22 | 0.532 | 44.3 | 2.03 | 44.74 | 2.45 | 0.44 | 0.097 | 0.675 | 0.938 | 0.534 |
| SGo/NMe ∗ 100% | 64.89 | 5.39 | 66.30 | 6.81 | 1.41 | 0.022 | 66.88 | 4.87 | 68.14 | 5.11 | 1.26 | 0.066 | 0.113 | 0.209 | 0.939 |
| U1/SN (°) | 99.39 | 8.88 | 98.67 | 9.02 | −0.73 | 0.525 | 100.83 | 8.54 | 102.97 | 7.68 | 2.14 | 0.072 | 0.495 | 0.036 | 0.082 |
| U1/PP (°) | 106.30 | 8.49 | 106.24 | 8.58 | −0.06 | 0.960 | 107.75 | 8.54 | 109.97 | 6.88 | 2.22 | 0.025 | 0.483 | 0.050 | 0.135 |
| L1/MP (°) | 92.73 | 8.03 | 90.39 | 7.40 | −2.33 | 0.061 | 91.88 | 8.31 | 90.66 | 7.44 | −0.99 | 0.285 | 0.667 | 0.884 | 0.370 |
| U1/L1 (°) | 131.52 | 9.51 | 136.48 | 10.75 | 4.97 | 0.014 | 134.79 | 8.38 | 135.67 | 10.16 | 0.88 | 0.568 | 0.133 | 0.746 | 0.096 |
| OB (mm) | 2.12 | 1.73 | 3.39 | 2.09 | 1.27 | 0.002 | 2.24 | 1.22 | 3.40 | 1.69 | 1.16 | 0.000 | 0.749 | 0.985 | 0.814 |
| OJ (mm) | 0.95 | 0.95 | 1.15 | 1.58 | 0.20 | 0.507 | 0.56 | 0.63 | 0.42 | 0.72 | −0.14 | 0.269 | 0.043 | 0.014 | 0.281 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


