Introduction
Closure and long-term retention of anterior open bites are significant concerns for orthodontists and their patients. In this study, we investigated the efficacy of orofacial myofunctional therapy (OMT) for maintaining closure of open bites in conjunction with orthodontic treatment.
Methods
The sample included 76 subjects with dental anterior open bites referred for OMT before, during, or after relapse of orthodontic treatment. The experimental cohort consisted of 27 subjects who received OMT and orthodontic treatment or retreatment. The control cohort comprised 49 subjects who had a history of orthodontic treatment with open-bite relapse. Overbite was evaluated by an OMT professional or orthodontist 2 months to 23 years after removal of the fixed appliances. Measurements were compared with t tests.
Results
Overbite relapse means were 0.5 mm (range, 0.0-4.0 mm) in the experimental group and 3.4 mm (range, 1.0-7.0 mm) in the control group, a difference that was clinically and statistically significant ( P <0.0001).
Conclusions
This study demonstrated that OMT in conjunction with orthodontic treatment was highly effective in maintaining closure of anterior open bites compared with orthodontic treatment alone.
There is general agreement among orthodontists that patients with anterior open bites are challenging to treat, and relapse is common after treatment with orthodontics alone or combined with orthognathic surgery. The orthodontic literature describes various methods for treatment and retention aimed at decreasing the risk of open-bite relapse, including functional and fixed appliances, tongue spurs or cribs, elastics, wires, molar intrusion, orthognathic surgery, extractions, partial glossectomy, and orofacial myofunctional therapy (OMT). Investigators have cited tongue position or activity as reasons for difficulty in achieving long-term closure of anterior open bites. With this in mind, many authors have stated that OMT or other muscle training and habituation exercises might be useful; however, the benefits of OMT remain questionable to many.
The reasons cited for lack of enthusiasm for OMT in orthodontic practices include (1) limited office space for providing therapy, (2) absence of OMT providers, (3) difficulty and amount of time required, (4) inadequate training, (5) hope that function will follow form, (6) belief that there is insufficient scientific evidence to support OMT, and (7) observations that not all OMT providers have the same expertise, so successful results are unpredictable. It is clear that additional research needs to be published in the orthodontic literature to evaluate OMT for the treatment of anterior open bites. Table I lists 22 studies that have documented outcomes of anterior open-bite treatment and is divided into 3 sections. The first section shows the percentages of relapsed subjects in 11 comprehensive studies totaling 1416 subjects not using OMT. The second section represents 4 patients from case reports who received tongue training with orthodontic appliances and 5 who had orthodontic appliances only. These 9 patients were reported as having no relapse. The third section lists 4 studies that documented the amount of closure of open bites with OMT alone in 195 patients.
| Author | Method | Mean closure | Relapse | n |
|---|---|---|---|---|
| Comprehensive studies, postorthodontic treatment | ||||
| Lopez-Gavito et al | Appliances | 35% relapsed 3 mm or more | 41 | |
| Dennison et al | Surgery | 42.9% relapsed | 66 | |
| Janson et al | Non-extraction; fixed appliances | 38.1% relapsed | 21 | |
| Hoppenreijs and van der Linden | Orthodontics and surgery | 19% relapsed | ? | |
| Al Yami et al | Appliances | 33% relapsed | 1016 | |
| Lo and Shapiro | Surgery | 25% relapsed; 0.7-1.0 mm cited as insignificant | 40 | |
| Gile | Appliances | 35% relapsed more than 1 mm | 100 | |
| Katsaros and Berg | Appliances | 25% relapsed; those who could advance mandible to achieve incisor occlusion were not considered relapsed | 20 | |
| Zuroff | Appliances | 60% relapsed; maximum relapse was 2.4 mm | 64 | |
| Kim et al | Multiloop edgewise archwire | Insignificant relapses of 0.23 mm for growing and 0.35 mm for nongrowing subjects | 55 | |
| Huang et al | Cribs | 17% relapsed | 33 | |
| Case reports, postorthodontic treatment and muscle therapy | ||||
| Zimmerman | OMT and appliances | 0.0 mm | 1 | |
| Justus | Spurs | 0.0 mm | 3 | |
| Beane | Appliances | 0.0 mm | 1 | |
| Efstratiadis | Appliances | 0.0 mm | 1 | |
| Lindsey and English | Appliances and muscle therapy | 0.0 mm | 1 | |
| Lee | Appliances and muscle therapy | 0.0 mm | 1 | |
| Alexander | Appliances, muscle therapy, and extractions | 0.0 mm | 1 | |
| OMT | ||||
| Haruki et al | OMT only | 5.0 and 2.5 mm | 2 | |
| Benkert | OMT only | 1.5 mm | 90 | |
| Daglio et al | OMT only | 5.5 mm | 28 | |
| Daglio et al | OMT only | 2.1 mm | 75 | |
Characterizations of open bites have varied. Chase described open bite as a condition characterized by space discrepancies between the occlusal and incisal surfaces of the maxillary and mandibular teeth when the mandible is brought into habitual or centric occlusion. Ferguson stated that, in the United Kingdom, an anterior open bite is described as the absence of vertical incisor overlap between the maxillary and mandibular incisors, whereas an incomplete overbite has vertical overlap, but the mandibular incisors fail to make contact with either their antagonists or the palate. He also noted that, in the United States, both conditions have been called anterior open bite, but, with a true anterior open bite, it is impossible to achieve incisor contact, whereas this can sometimes be accomplished if the mandible is protruded in patients with incomplete overbites. In our study, open bites were defined as the mandibular incisors failing to make contact with their antagonist teeth or the palate when observed with the posterior teeth in maximum intercuspation and no contact of incisors with excursive movements.
In this investigation, we compared subjects who were treated with orthodontics alone vs those treated with orthodontics combined with OMT; we used retrospective data from the practice of an orofacial myofunctional therapist (J.S.). The purpose was to evaluate whether completion of an OMT program before removal of the orthodontic appliances decreases the risk of relapse of closed anterior open bites.
Material and methods
All subjects were referred by orthodontists to an OMT private practice because of dental anterior open bites and Angle Class I or Class II malocclusion. Open bite was measured to the nearest whole number as the vertical discrepancy between incisal edges of the mandibular central incisors and the lingual surface of the maxillary incisors or palate. No subject could contact the incisors by protruding the mandible, thus fitting the criterion of a true anterior open bite according to Ferguson. The experimental group of patients having orthodontic treatment and OMT was compared with the control subjects, who had received only orthodontic treatment.
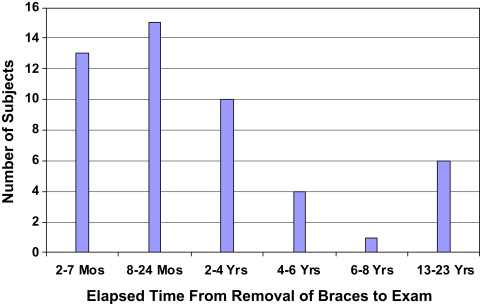
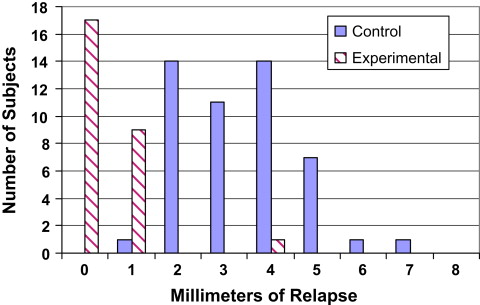
The control cohort consisted of 49 patients referred by 28 orthodontic practices for an OMT examination after orthodontic relapse. They included 15 male and 34 female subjects with a mean age of 17 years 8 months (SD, 7 years 9 months; range, 10-41 years) at the OMT examination. At debanding, 44 (90%) of the control subjects were reported by their orthodontists to have closed open bites; 3 subjects remained open from 0.5 to 2.0 mm (mean, 1.2 mm), and 2 subjects were not closed, but the amount of open bite at the time of discharge had not been recorded. Eighty-four percent of the subjects or their families noticed their bites opening within 2 years after debanding, although only 58% were professionally measured within 2 years. The time between active orthodontic treatment and the OMT examination ranged from 2 months to 23 years (mean, 3 years 11 months; SD, 5 years 11 months; Fig 1 ). The distribution of the amounts of relapse in control subjects was relatively symmetric compared with the experimental subjects ( Fig 2 ). Forty-five of the 49 control subjects were not seen again in the OMT practice, but 4 patients chose to receive OMT and orthodontic retreatment and also became part of the experimental cohort.
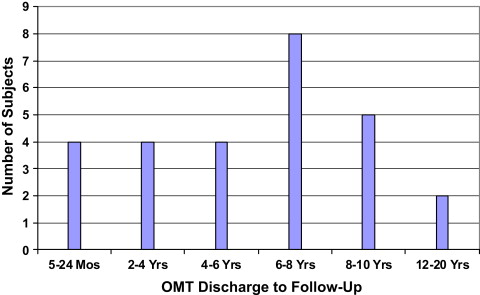
The experimental group comprised 27 subjects who had been referred for OMT from 20 orthodontic practices, either before or during orthodontic treatment. They included 5 male and 22 female subjects with a mean age of 14 years 1 month (SD, 6 years 5 months; range, 8-38 years) when OMT was completed between 1981 and 2003. Four subjects had relapsed after active orthodontic treatment (from the control group above), and 23 subjects had no previous history of fixed orthodontic treatment. The patients were treated by orofacial myologists in 1 practice, which used a standardized approach as instructed by the first author (J.S.). They were reevaluated 5 months to 20 years (mean, 6 years 2 months; SD, 4 years 2 months) after orthodontic treatment ( Fig 3 ). Their ages at the follow-up for the experimental group were 14 to 39 years (mean, 20 years 3 months; SD, 6 years 5 months); 96% of the patients were measured a minimum of 2 years after their last OMT visit. Overbite measurements were made by either an OMT therapist or orthodontist.
All initial and final examinations included a review of medical and dental histories, measurement of the amount of open bite, obtaining frontal intraoral photographs, and documentation of oral physiologic characteristics including habitual lip posture (open or closed), swallow patterns of the tongue (protruded or palatal), tongue rest posture (low forward or palatal), oral habits (digit sucking, lip licking or biting, or none), and speech articulation errors. Recitation of the alphabet and conversational speech were analyzed for accuracy of tongue and lip movements and sound production. Each item in the evaluations had a numeric value of 0 to 4; the sum categorized the subjects according to mild, moderate, severe, or profound dysfunction. For the experimental group, the OMT treatment regimen involved selectively prescribing exercises (from 49 exercise options) for normalization of orofacial muscles for rest, swallowing, eating, drinking, and speaking. Exercises, similar to the remedial program of Weiss and van Houten, were printed and videotaped for home practice. The number of OMT exercises and sessions for each patient was determined by the severity of speech errors, oral habits, medical conditions, and the patient’s motivation and response to the exercises (range, 1-32 sessions; mean, 14 ± 8). At each visit, the orofacial myofunctional therapist assessed patient compliance and motivation. At the final OMT session, the original examination was readministered.
Relapse amounts were quantified clinically and the means compared between groups. To analyze whether there was any systematic bias between the 2 professionals, measurements made by orofacial myofunctional therapists vs orthodontists were compared. Overbite measurements of the experimental subjects were compared with their original measurements and with those of the control group. In the experimental cohort, differences in open-bite reduction of subjects who had not previously received orthodontic treatment were compared with subjects who had orthodontic retreatment. Based on the model of Kim et al, suggesting that age might be a factor, subjects who were younger than 16 years after OMT were compared with older subjects. Differences in open-bite reduction and relapse were also compared between the sexes. The influence of speech errors corrected vs not corrected was investigated to determine the effect on relapse. Correlations were made between the number of OMT sessions and initial open bite, oral habits, speech errors, and relapse.
For comparison of open-bite reduction and relapse, t tests were used, with the level of significance set at P <0.05. Analysis of covariance was used for comparing the times between removal of the orthodontic appliances and the OMT examination in the control cohort, and between completion of the OMT and the follow-up in the experimental cohort. Linear regression analysis and correlation coefficients were used to identify characteristics that related to relapse in the control cohort and the amount of open-bite reduction and relapse in the experimental cohort.
Results
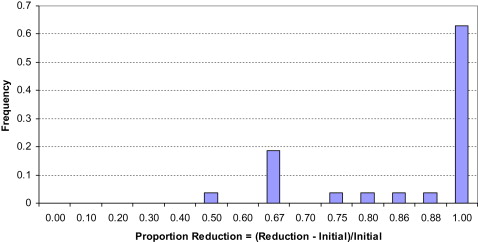
Comparison of measurements made by orofacial myofunctional therapists vs orthodontists at the follow-up showed the 2 did not differ statistically. The relapse differences between the experimental cohort (treated with orthodontics and OMT) and control cohort (treated with orthodontics alone) as shown by the t tests were highly statistically significant ( P <0.0001; Table II ). The distribution of relapse of the control subjects was relatively symmetric ( Fig 2 ; range, 1-7 mm; mean, 3.4 ± 1.3 mm). In the experimental group ( Fig 2 ), 17 of the 27 subjects (63%) had no measureable relapse; 9 had a 1-mm relapse, and 1 had a 4-mm relapse. Thus, relapse of the experimental subjects was small. Overall, the experimental group showed 0.48 ± 0.8 mm of open-bite relapse ( Table II ). The amounts of reduction in open bite were 1 to 8 mm (mean, 3.6 ± 2.0 mm), and 63% of the experimental subjects had a 100% reduction in open bite ( Fig 4 ).
| Experimental group | Control group | |
|---|---|---|
| Subjects (n) | 27 | 49 |
| Relapse range (mm) | 0-4 | 1-7 |
| Relapse mean (mm) | 0.48 ± 0.8 | 3.38 ± 1.3 |
| Standard deviation | 0.8 | 1.3 |
In the experimental cohort, the mean reduction in open bite did not differ significantly between the treated and retreated subjects ( P = 0.33). Subjects younger than 16 years of age at OMT completion had significantly greater mean reductions of open bite than did those older than 16 ( P <0.05), but the younger subjects also had greater open bites initially (mean, 4.65 vs 2.71 mm). Sex was not significantly associated with the amount of open-bite reduction. The correction of speech errors was not significantly associated with the amount of open-bite reduction ( P = 0.33) or relapse ( P = 0.16). The number of OMT sessions was associated with the severity of the orofacial myofunctional disorder, motivation, and compliance, but was not related to the stability of the overbite. There were no correlations between number of sessions, initial open bite, number of oral habits, number of speech errors, or amount of relapse. However, speech errors significantly decreased as the number of sessions increased ( P <0.01).
In the control group, the mean time between active orthodontic treatment and the OMT examination was 3 years 11 months ( Fig 1 ). In the experimental group, the mean time between completion of OMT and the follow-up OMT examination was 6 years 2 months ( Fig 3 ). Time between OMT completion and follow-up in the experimental group was significantly longer than the time between active orthodontic treatment and the OMT examination in the control group ( P <0.05). The initial measurements of open bite in the experimental group ranged from 1.0 to 8.0 mm (mean, 4.1 ± 2.1 mm). The amount of open-bite reduction at follow-up ranged from 1.0 to 7.0 mm (mean, 3.6 ± 2.0 mm). There was a high correlation between the amounts of initial open bite and open-bite reduction at follow-up (r = 0.92; P <0.001).
In the control group, 74% of the subjects had oral habits, whereas at the final evaluation of the experimental subjects, the prevalence of oral habits was reduced from 55% to 0%. For speech errors, 82% of the control group retained their speech errors, but these in the experimental group were reduced from 90% to 26% of the subjects. Typical speech sounds misarticulated by both groups were l, s, z, t, d, n, sh, ch, and j . Tongue rest posture and swallow patterns were normal at the final evaluations for all experimental subjects.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


