The goal of replacing missing teeth while respecting otherwise untouched tooth structure and the avoidance of crown reduction in bridge preparation make the use of dental implants an ideal option for restoring dentitions ravaged by traumatic tooth loss. Patients who suffer tooth loss resulting from traumatic injuries of the dentoalveolar complex can be divided into growing and nongrowing patients. The placement of dental implants can have deleterious effects on the growing alveolar process. The authors’ philosophy is to respect growth and delay implant reconstruction until the cessation of skeletal or alveolar growth, as documented by serial lateral cephalometrics radiographs taken 6 months apart.
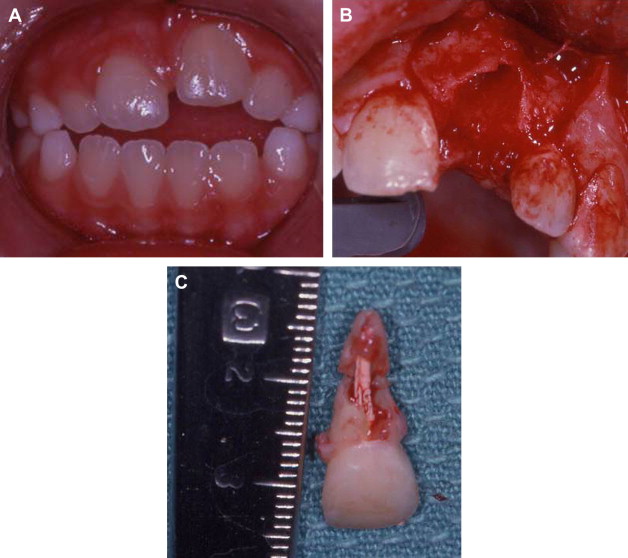
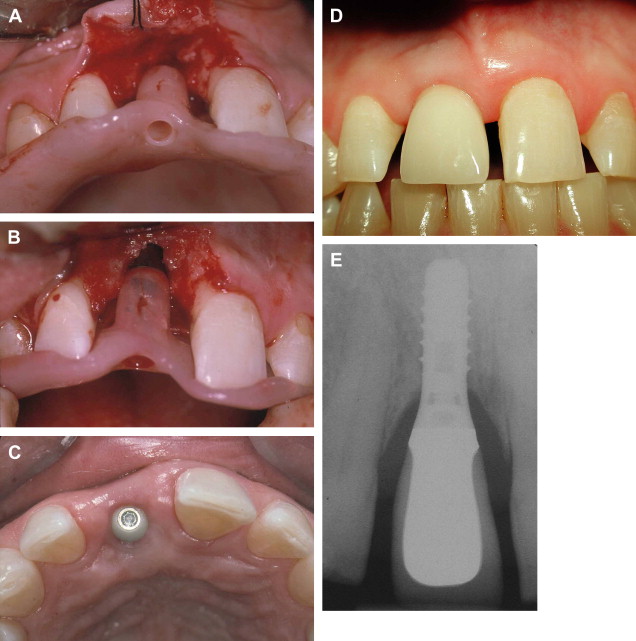
The ability to replace teeth without damaging the residual dentition makes the use of dental implants an ideal option to consider for restoring dentitions ravaged by traumatic tooth loss ( Fig. 1 ). Patients who suffer tooth loss resulting from traumatic injuries of the dentoalveolar complex may still be growing, and, in fact, certain injuries resulting in tooth loss are seen more commonly in young patients (for example, avulsions of anterior teeth). Dental implants, like ankylosed teeth, can have deleterious effects on the growing alveolar process ( Fig. 2 A–C). As a general rule, the authors’ philosophy is to respect growth by delaying implant placement until the cessation of skeletal growth ( Fig. 3 A–E), as documented by serial lateral cephalometric radiographs taken 6 months apart.

In addition to growth, a number of other factors associated with tooth loss also must be considered when assessing a traumatized dentition ( Box 1 ).
-
Cessation of skeletal growth
-
Single versus multiple tooth loss
-
Prognosis of residual dentition and likelihood of future tooth loss
-
Associated loss of alveolar bone
-
Associated soft tissue scarring and deficits
-
Associated fractures of the facial bones
Assessment of the residual dentition
No two complex fractures involving the dentition, it seems, are ever the same. The posttraumatic residual dentition must be analyzed carefully to help predict its prognosis. Teeth that have been reimplanted, suffered root fractures, or been treated endodontically will impact adversely the overall prognosis (see Fig. 2 A–C), as they may be lost in the future, necessitating further costly treatment. Considerations of potential future tooth loss will often have important medicolegal implications especially as it related to insurance liability.
Loss of hard and soft tissues
Loss of alveolar bone associated with tooth avulsion may require that ridge augmentation, perhaps using guided bone regeneration or other techniques, be incorporated into the reconstruction treatment plan ( Fig. 4 A–C). In addition, the deleterious effects of soft tissue scarring on the final esthetic outcome must be anticipated and communicated to the patient and family ( Fig. 5 A–C) and dealt with where appropriate through the use of soft tissue grafting or flaps ( Fig. 6 A–H).
Loss of hard and soft tissues
Loss of alveolar bone associated with tooth avulsion may require that ridge augmentation, perhaps using guided bone regeneration or other techniques, be incorporated into the reconstruction treatment plan ( Fig. 4 A–C). In addition, the deleterious effects of soft tissue scarring on the final esthetic outcome must be anticipated and communicated to the patient and family ( Fig. 5 A–C) and dealt with where appropriate through the use of soft tissue grafting or flaps ( Fig. 6 A–H).




