Benign and malignant conditions can result in the need for ablative surgery where segments of the tooth-bearing portions of the jaws require removal for adequate disease control. Aggressive cystlike lesions of the jaws may result in destruction of large areas of the alveolus and underlying structures, resulting in the loss of teeth. Tumors such as ossifying fibroma, aggressive fibromatosis, central giant cell granuloma, and ameloblastoma may lead to defects that are challenging to restore. This article examines the reconstruction of such ablative defects and those areas of deficient growth induced by radiotherapy in childhood to treat tumors such as rhabdomyosarcoma, retinoblastoma, or neuroblastoma.
Excision of benign and malignant orofacial lesions often extends into tooth bearing portions of the jaws in order to provide for adequate disease control. Aggressive cystlike lesions of the jaws may destroy large areas of the dentoalveolar process and underlying structures, resulting in the loss of teeth. Removal of tumors such as ossifying fibroma, aggressive fibromatosis, central giant cell granuloma, and ameloblastoma may create defects that are challenging to restore. This article examines the reconstruction of ablative defects and of regions of the jaws arrested in development by delivery of radiotherapy in childhood to treat tumors such as rhabdomyosarcoma, retinoblastoma, or neuroblastoma.
Odontogenic keratocysts
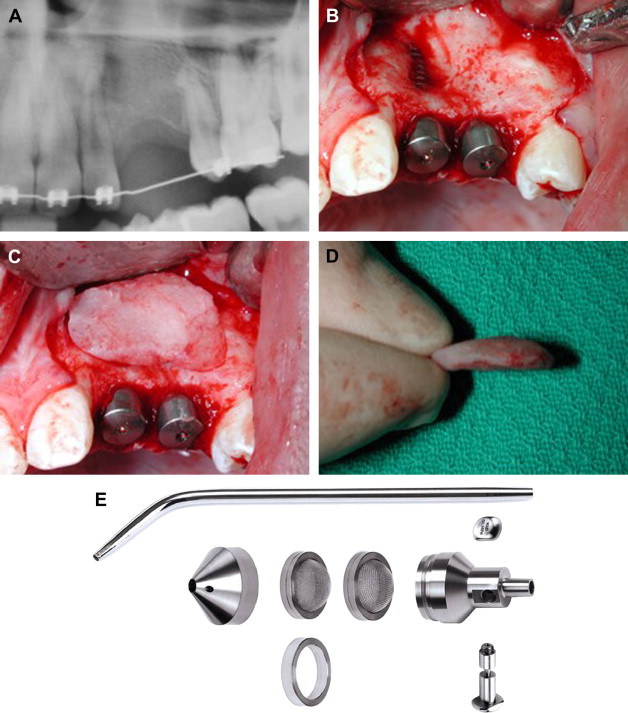
Odontogenic keratocysts can be aggressive, and their removal can lead to major dentoalveolar loss requiring future reconstruction. The management of odontogenic keratocysts is made more difficult because they tend to recur. The syndromic association of multiple odontogenic keratocysts with basal cell carcinomas is called basal cell nevus (Gorlin) syndrome. The gene responsible for this condition has been identified and is known as the sonic hedgehog gene. The management of both new and recurrent lesions in these patients is challenging. The risk of recurrences is elevated in adolescence and early adulthood so dental reconstruction should be postponed until growth has ceased ( Figs. 1 A– 1 I).
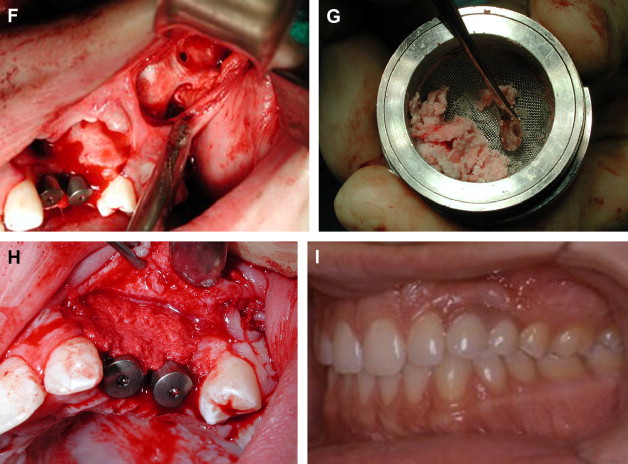
Other aggressive lesions such as the widespread recalcitrant pyogenic granulomas of the maxilla can also be challenging to manage and reconstruct ( Figs. 2 A– 2 H).
Fibro-osseous and giant cell lesions of the jaws
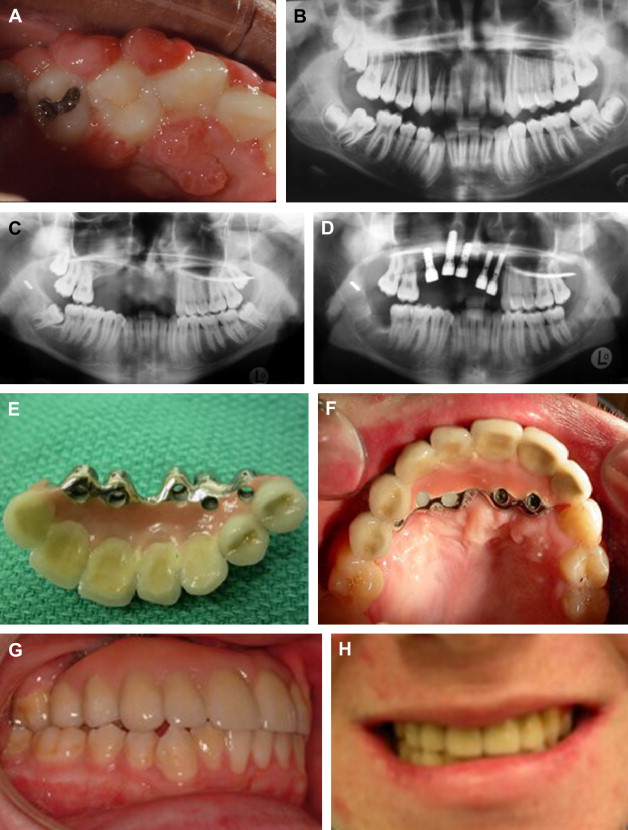
In children who are congenitally missing one or more teeth, treatment is usually postponed until after the cessation of skeletal growth in order to avoid disturbing normal dentoalveolar development. In contrast, in children with certain pathologies, the lesion must be removed irrespective of the stage of growth of the patient. If growth is incomplete at the time of surgery, then some disruption of normal development is inevitable either as a result of scarring or constraint caused by reconstruction hardware or because of failure of a free tissue transfer such as a fibula to grow. In cases such as these, where the ablative surgery itself is expected to impede or restrict growth of the jaws, and little or no further restriction would be expected to be superimposed by dental implants placed into the ablative defect, then a decision to proceed with the placement of implants may be made if there is sufficient functional and psychosocial justification to do so. Certain fibro-osseous lesions of the jaws may require resection during childhood. One such lesion is the ossifying fibroma. Large areas of the tooth-supporting alveolus may be lost when these lesions are resected ( Figs. 3 A– 3 D). Another such lesion is the giant cell granuloma when it cannot be successfully treated with serial steroid injections so that jaw resection is required to gain control of the lesion.
Placement of implants into an ablative defect reconstructed using plates and screws permits the removal of the reconstruction hardware at the time of implant placement. Removal of reconstruction hardware while the patient is still growing may in some instances permit growth of the affected areas of the jaws to resume as long as it is not further constrained by dental implants or by an implant supported prosthesis. In reconstructions involving the mandibular symphysis we have employed a prosthesis designed with a split at the midline to accommodate potential transversal growth. However, in a series of five young children reconstructed with cross-arch implant-supported fixed bridges split at the midline in vascularized free fibular grafts, we have seen no separation of the right and left sides of the bridges as might be expected were the mandibles to have grown transversally in the intercuspid regions. Implants and implant supported reconstructions are not expected to grow vertically together with the rest of the developing arch. Consequently, the implant reconstruction should be remade periodically in order to avoid distortion of the occlusal plane and overeruption of the opposing dentition.
Such reconstructions can be performed in vascularized bone grafts ( Figs. 4 A– 4 K) or in free nonvascularized bone grafts ( Figs. 5 A– 5 L). The maintenance of good oral hygiene around implant reconstructions is extremely important in young children; despite parental attempts, these patients may find it challenging to keep the tissue around the implants in a healthy state (see Fig. 4 K).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


