Introduction
A discrepancy exists between objective and subjective measures of orthodontic treatment need, highlighting the importance of patients’ perceptions. Limited qualitative information is available regarding patients’ perceptions and orthodontic concerns. For the first time, patient facial images and qualitative methodology were used to assess patients’ orthodontic concerns, which are incorporated into and are important in treatment planning and consent.
Methods
An interview-based, cross-sectional study of adolescent patients eligible to receive orthodontic treatment in a public dental hospital was conducted with 105 adolescents (42 boys, 63 girls) aged between 12 and 17 years. Each patient’s face was video recorded, and 3 images were selected from each recording to assess the patient’s orthodontic concerns. The initial chief concerns were compared with concerns articulated after the patients assessed their facial images. In addition, patient concerns were compared with occlusal features visible on smiling using the Dental Aesthetic Index and patient study casts.
Results
For 37% of the adolescent patients, smiling images helped to identify additional concerns. For 87%, their smiling images helped them to describe their concerns in more detail. In addition, a few patients did not articulate any concern about features measurable on the Dental Aesthetic Index that were visible on smiling.
Conclusions
Showing adolescent patients images of their face and smile helped them to identify and better describe their concerns. Adolescents are not always overly concerned about visible and quantifiable malocclusion features. This might influence orthodontic treatment planning and consent.
Highlights
- •
Discrepancies between objective and subjective treatment-need measures were studied.
- •
Smiling images helped adolescents to identify additional concerns.
- •
Smiling images helped subjects to describe their chief concerns in more detail.
- •
Adolescents were most concerned about the appearance of malaligned teeth.
- •
They were also concerned about prominent front teeth, cleaning, and diastemas.
People, in general, agree on attractiveness. Attractive people are considered to be more successful, intelligent, and socially more popular. When face-to-face conversations occur, the focus is mainly on the mouth and the eyes. Therefore, the smile is considered a dynamic feature of facial and overall attractiveness. Authors of a recent study using eye tracking demonstrated that the eyes are the most observed facial feature with regard to duration and fixation, followed by the mouth.
Desire for orthodontic treatment may be strongly influenced by the appearance of the teeth when smiling and the perceived social and psychological impact this might have on others. Poor dental appearance can negatively impact people on a day-to-day basis, and people adopt strategies to cope socially. Common strategies include avoidance of showing teeth, minimizing the importance of appearance, and seeking orthodontic treatment.
In a public-funded orthodontic system, priority is often given to the most handicapping malocclusions measured by indexes that attempt to objectively ascertain orthodontic treatment need. A commonly used occlusal index is the Dental Aesthetic Index (DAI). Briefly, the DAI is endorsed by the World Health Organisation as a cross-cultural international index because of its high reliability and validity. The DAI measures 10 occlusal features that are weighted using a regression coefficient formula based on the opinions of adolescents and adults. The total DAI score is the sum of all weighted measures plus a constant. Adolescents and adults have rated dental esthetics and the social impact of different malocclusions; therefore, an esthetic impact does not need to be measured separately. Although occlusal indexes are effective screening and epidemiologic tools, most do not incorporate patient perceptions or psychosocial impacts. Therefore, index-determined orthodontic treatment need may conflict with a patient’s desire for orthodontic treatment.
Index-determined orthodontic need does not necessarily result in treatment uptake, and some patients might have dental appearance dissatisfaction disproportionate to their malocclusion severity. Therefore, orthodontic treatment can be considered elective in most cases; this highlights the importance of patient perceptions in orthodontics.
Traditionally, most active orthodontic treatment has been carried out during adolescence, which is the transition from childhood to adulthood. During this time, persons develop their social identity, self-image (especially body image), and self-worth, and these constructs are strongly influenced by external factors such as media, family, friends, and peers. If the motive for orthodontic treatment is powered by social norms and pressures, it could explain why some adolescent patients are overcritical of certain occlusal features. Nevertheless, adolescent orthodontic perceptions are important; therefore, adolescents are a relevant group to study.
A clear understanding of patients’ orthodontic concerns is essential to obtain successful treatment outcomes and fulfil patients’ expectations. To our knowledge, this was the first time that videography has been used to explore the orthodontic concerns of adolescent patients in a clinically relevant way. Two null hypotheses were postulated in this study: (1) not all adolescent orthodontic patients can communicate their chief concerns equally well, with or without viewing their own facial images; and (2) not all adolescent orthodontic patients are sensitive to their occlusal features visible on smiling, with the DAI as an objective reference.
Material and methods
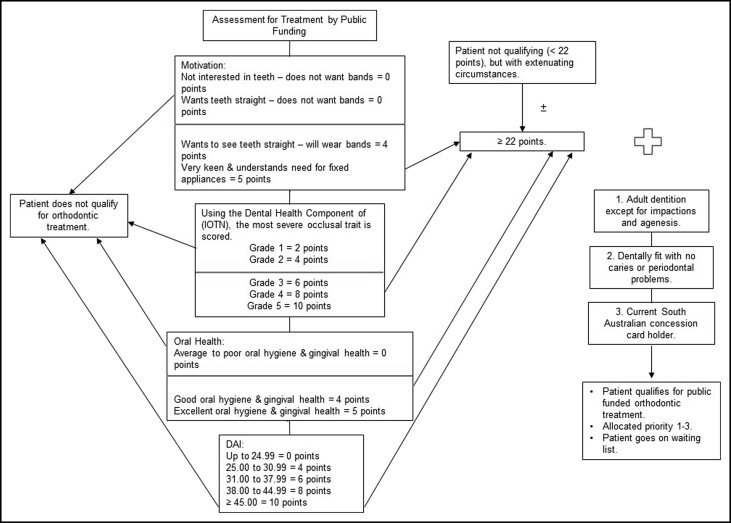
Ethics approval for this cross-sectional, interview-based study was obtained from the Women’s and Children’s Health Network, Human Research Ethics Committee (HREC/13/WCHN/133), and involved eligible adolescent patients referred for specialist orthodontic treatment at the Adelaide Dental Hospital and residing in the state of South Australia. Eligibility for specialist orthodontic treatment at this hospital depends on multiple clinical factors and a valid South Australian health care concession card. Good oral hygiene and health are prerequisites to access public-funded specialist orthodontic treatment ( Fig 1 ).
Adolescents between 12 and 18 years of age without active orthodontic appliances in place were considered for inclusion. Patient recruitment depended on consent, the availability of a researcher to conduct interviews, and the inclusion criteria.
Patients were recruited and interviewed during the consultation stages before active treatment ( Fig 2 ).The patient and the parent or guardian were verbally informed about the purpose and procedures involved in the research project. A detailed information sheet was provided, including a copy of the consent form. The patient and parent or guardian had an opportunity to ask questions about the study. Written consent was obtained from the parent or guardian of each patient, and participation was voluntary with no incentives offered. Consent included the use of existing study casts for evaluation. An unwillingness to participate did not influence a patient’s access to specialist orthodontic services.
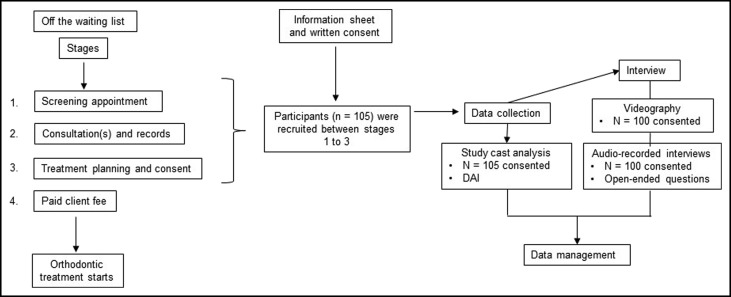
The interview consisted of 2 components and took approximately 30 minutes to complete ( Fig 2 ). All audio recordings were coded to protect the privacy of the patients for data entry and reporting. Patients could withdraw their consent at any stage.
All interviews were conducted in the same well-lit room annexed to the orthodontic clinic. Each patient’s face was video recorded, and the main objective of the video recordings was to capture the dynamic nature of the smile cycle. The goals were to provoke a natural, repeatable posed smile and to observe the teeth in the soft tissue smile frame. When a satisfactory smile could not be produced, participants were asked to say “cheese!” A digital camera (EOS 50D SLR; Canon, Tokyo, Japan) with an EF 100-mm macro lens (Canon) was used for the video recordings. The video function recorded 25 frames per second in high definition at video settings of ISO 1000, shutter speed of 1/125 second, and aperture of f 5.6. A standard tripod was erected 2.4 m from the zone in which the participants were asked to stand, and the camera was aligned parallel to the floor. Each video recording took approximately 20 to 30 seconds. A laptop personal computer with processing capacity to manage the video recordings was used to import the data. PlayMemories Home (Sony, Tokyo, Japan) was used to identify specific image frames from the video recordings, and 1 researcher (E.T.) selected 3 image frames from each video recording. The image frames that best represented the patient’s face in profile, full-frontal (nonsmiling), and full-frontal (smiling and showing teeth) views were selected. A digital audio recorder (DS 4000; Olympus, Tokyo, Japan) was used during the face-to-face interviews.
Subsequently, participants were asked about their orthodontic concerns in open-ended questions. These questions were standardized and printed in the questionnaire booklet as a template, and the participants’ answers were audio recorded for transcription. The 2 questions were the following.
Question A: “In your own words, what worries you about your teeth that makes you want orthodontic treatment like braces?”
At the end of the interviews and by showing the participants their 3 images (profile, full-frontal nonsmiling, and full-frontal smiling), one image at a time, they were asked the next question.
Question B: “Is there anything that worries you about this image?” If the participant answered “yes,” he or she was asked to explain that worry in a show-and-tell fashion. If the participant answered “no,” the interviewer moved on to the next image.
The patients’ concerns (chief concerns and concerns from their smiling image) were compared with the DAI features visible on smiling. The DAI was used to assess occlusal features seen on smiling and to evaluate objectively measured orthodontic treatment need. Six occlusal features were investigated: spacing, midline diastema, maxillary anterior irregularity, maxillary anterior overjet, mandibular anterior overjet, and vertical anterior open bite. The first author (E.T.) was calibrated in the use of the DAI by a gold standard user. Intrarater repeatability was tested on 15 study casts that were randomly selected by staff not involved with the study using an Internet-based random number generator program. The first author was blinded to the process and repeated the measurements at least 4 weeks after the initial measurements. Using a Bland-Altman plot, 12 of the 15 repeated DAI scores were within 1 SD of 1.6 (set at 1.6). The 95% confidence intervals of the differences were between –0.9 and 0.92, with a mean of 0.01.
Statistical analysis
The recorded answers to the open-ended questions were transcribed by the first author for analysis. Similar responses and ideas were distilled, grouped, and categorized using inductive content analysis. In other words, similar patient concerns were grouped and categorized until no new categories emerged from the patient responses. The 105 patients provided sufficient information for content saturation. The methodology was tested on a pilot group of 15 patients, and there was excellent agreement between the first and second (R.M.R.) authors. Associations involving sex and DAI scores were tested using the Mann-Whitney test. The statistical analyses were completed with SAS software (version 9.3; SAS Institute, Cary, NC).
Results
Patients were recruited between December 2013 and August 2014. During this period, 411 new patients between 12 and 17 years of age had an orthodontic consultation. Of them, 105 agreed to participate in the study (63 girls, 42 boys). Five participants did not consent to the video and voice recordings and were excluded for content analysis. Recruitment was limited by the availability of the first author and finding a convenient time to interview patients. Of the 105 patients, 102 consulted a specialist orthodontist or an orthodontic registrar other than the first author.
The patients’ ages ranged from 12.3 to 17.8 years. The mean ages and standard deviations were 15.5 years (SD, 1.4 years) for the boys and 15.4 years (SD, 1.5 years) for the girls.
The patients came from 48 Adelaide metropolitan post codes and 15 country post codes. They represented several ethnic groups, including Vietnamese (6%), Iraqi (3%), Greek (2%), Filipino (2%), Cambodian (2%), other (10%), and Anglo-Australian (75%).
The majority of the patients had an orthodontic treatment need defined as “highly desirable” or “mandatory” according to the DAI ( Table I ). There was no statistically significant difference between the DAI scores by sex ( P = 0.371). The DAI scores for the girls had a mean of 33.7 (SD, 5.7; median, 32.8; minimum, 23.8; maximum, 48). The DAI scores for the boys had a mean of 36.3 (SD, 9.3; median, 33.4; minimum, 23.3; maximum, 59.4).
| DAI total score (severity level) | Patients (n) | Patients (%) |
|---|---|---|
| <25 | 6 | 5.7 |
| 26-30 | 30 | 28.6 |
| 31-35 | 33 | 31.4 |
| >36 | 36 | 34.3 |
| Total | 105 | 100 |
The patients’ chief concerns (answers to question A) are categorized and summarized in Table II . Their concerns articulated and related to their facial images (answers to question B) are summarized in Table III . Some patients had more than 1 category of concern.
| Chief concern category | Patients (%) |
|---|---|
| Appearance of malaligned teeth | 73 |
| Prominent front teeth /increased overjet | 20 |
| Difficulty cleaning malaligned teeth | 11 |
| Spaces between front teeth | 10 |
| Size and shape of teeth | 5 |
| How the teeth bite together | 5 |
| Color of teeth | 4 |
| No particular concern | 4 |
| Missing teeth | 3 |
| Increased overbite | 2 |
| Grinding of teeth | 2 |
| Open bite | 1 |
| Prominent mandible | 1 |
| Temporomandibular disorder signs and symptoms | 1 |
| Concerned about speech | 1 |
| Image concern category | Patients (%) |
|---|---|
| Appearance of malaligned teeth | 73 |
| Subcategories | |
| Poor positioning, alignment, crookedness, crowding, or irregular front teeth | 43 |
| Buccal canines | 28 |
| Teeth blocked out, behind other teeth, or anterior crossbite | 22 |
| Individual tooth sticks out more without increased overjet | 13 |
| Rotated teeth | 9 |
| Apparent spaces between teeth or missing teeth, due to the positioning of teeth | 9 |
| Overlapping teeth | 8 |
| Teeth that appear tipped | 2 |
| Dental asymmetry | 2 |
| Missing front tooth (but space is closed) | 1 |
| Maxillary dental midline does not coincide with facial midline | 1 |
| Anterior occlusal cant | 2 |
| Transposition | 1 |
| Prominent front teeth (increased overjet) | 20 |
| Spaces between front teeth | 14 |
| No concerns | 10 |
| Size and shape of the front teeth | 10 |
| Prominent lower lip | 5 |
| Prominent nose | 4 |
| Tooth color | 4 |
| Retrusive mandible | 4 |
| Lip shape and form | 4 |
| Narrow maxilla | 2 |
| Prominent upper lip | 3 |
| Extra tooth | 2 |
| Prominent chin | 2 |
| Small chin | 1 |
| Open bite | 1 |
| “Unnatural” smile | 1 |
| Increased overbite | 1 |
| Prominent gums | 1 |
| Asymmetric mandible | 1 |
| Asymmetric face | 1 |
These adolescents were predominantly concerned about (1) the appearance of malaligned teeth, (2) prominent front teeth, (3) difficulty cleaning malaligned teeth, and (4) spaces between teeth. Quotes from the interviews support this.
“My teeth are crooked, and it makes it hard to brush my teeth sometimes. Food gets stuck in between them. My teeth influence my smile a bit.”
“Just the look of my teeth. It is hard to smile in photos and stuff, because my teeth look really bad in photos. They look all crooked, and I have a gap in my teeth.”
“My 2 front teeth stick out, and I just want them pushed back.”
The images provided additional information that might assist in orthodontic treatment planning. When the concerns from Tables II and III were compared, it was apparent that there were matching and nonmatching categories. The chief concern categories were mostly related to dental appearance (visible) and functional concerns (not visible from images). Alternatively, the concerns articulated after patients looked at their images were mainly about the appearance of their face and teeth. For these reasons, only concerns involving the teeth or the smile were considered for comparison for each patient. When the chief concern of “difficulty cleaning malaligned teeth” was supported by a concern with “appearance of malaligned teeth” from the smiling image, it was considered a match.
Chief concern categories and image concern categories were compared, and the results are presented in Table IV . Quotes from the interviews support the results.
| Patients (%) | Chief concern vs image concern categories | Quotes from the interviews |
|---|---|---|
| 54 | Concern categories coincided | CC: “I have gaps between them (teeth) and some are a bit smaller than the others.” |
| IC: “I do not really like the look of my teeth there … the smaller 1 there” (peg shaped 12) “and probably the gaps as well” (spaces between the maxillary incisors) | ||
| 9 | Concern categories coincided, but the chief concern provided additional concern categories | CC: “Grinding of my teeth and my teeth are not aligned properly. The alignment of my molars worries me.” |
| IC: “I am not really sure, just the alignment.” | ||
| 19 | Concern categories coincided, but the smiling image provided additional concern categories | CC: “They are not straight, and everyone else has pretty much straight teeth.” |
| IC: “They are so bad … my top teeth cover a lot of my bottom teeth”(overbite). “They are just not straight and sideways, instead of going flat, they are turned” (rotated 12, 11, 21, 22) “and there are gaps between them” (21, 22 and 22, 23). | ||
| 5 | Concern categories coincided, but the chief concerns and the smiling image concerns provided additional concerns categories | CC: “I am worried that I will be teased or bullied and people would judge the way my teeth look. I have got gaps in between my teeth, and I have an overbite; my top jaw is more forward” (refers to overjet). |
| IC: “The gaps between my teeth” (11, 21) “and my 2 front teeth are bigger” (11, 21). “Do you think they are bigger, or are the other 2 next to them smaller? I reckon they look bigger.” | ||
| 13 | The concern categories did not match | CC: “I do not have any adult teeth underneath a few of my teeth.” |
| IC: “My nose … it is sticking out … my small mouth in relation to my chin, my chin is small as well. My gums … they are pretty big.” |
The results suggest that for 37% of the patients, their smiling images were useful in identifying additional concerns; for 87% of the patients, their smiling images helped to describe their chief concerns in more detail.
Patients’ concerns (chief concerns and concerns from their smiling image) were compared with 6 DAI features visible on smiling, and the results are presented below.
Spacing
Ten patients of 100 had a chief concern of spaces between the teeth, and 8 confirmed their chief concern by looking at their smiling images. One patient had spaces in the posterior segments that were not visible on smiling and not recorded with the DAI. Another patient had no measurable spaces but perceived spaces owing to the irregular anterior teeth, which created the illusion of spaces.
Fourteen patients of 100 observed spaces in their smiling images. All had measurable spaces in 1 or 2 jaws according to the DAI. For 9 patients of 100, irregular anterior teeth created the illusion of spaces, and they were subsequently subcategorized under “appearance of malaligned teeth.”
Of the 25 patients with measurable spaces according to the DAI in either one jaw or both jaws, 11 did not notice the spaces. For 5 patients, this could be explained by the fact that the spaces were between posterior teeth, in the mandible, or not clearly visible from the smiling image. Therefore, 6 patients had measurable spaces in at least 1 jaw, according to the DAI, and the spaces were visible from the smiling images.
Midline diastema
Thirteen patients of 100 had a midline diastema of 1 mm according to the DAI. Nine of them mentioned this as a concern, but 4 did not mention it when they looked at their smiling images.
Four patients of 100 had a midline diastema of 2 mm according to the DAI. Two considered this a concern, whereas the other 2 patients were unconcerned when they looked at their smiling images.
Three patients of 100 had a diastema of 3 mm according to the DAI, and they all mentioned this as a concern.
Maxillary anterior irregularity
According to the DAI, maxillary anterior irregularity is the largest contact point displacement between the 4 maxillary incisors. Table V summarizes the results. Displaced canines are not recorded according to the DAI.



