Introduction
Management of mandibular condylar fractures is difficult in children with their inherently dynamic and unstable deciduous and mixed dentitions. We present a variation of the conservative fixed orthodontic approach that was used as an adjunct to aid in the reduction of a bilateral condylar fracture in a pediatric patient.
Methods
A boy, aged 10 years 9 months, came with clinical signs and symptoms of mandibular fracture after being involved in a motor vehicle accident. A computed tomography scan showed a vertical fracture on the left condylar head, a displaced fracture of the right condylar neck, and a mandibular symphysis fracture. The patient was treated with an orthodontic fixed appliance instead of an arch bar splint, followed by elastic traction to achieve a proper occlusion and condylar remodeling. Follow-up appointments were made 2 weeks and 1, 2, 20, 37, and 49 months after treatment.
Results
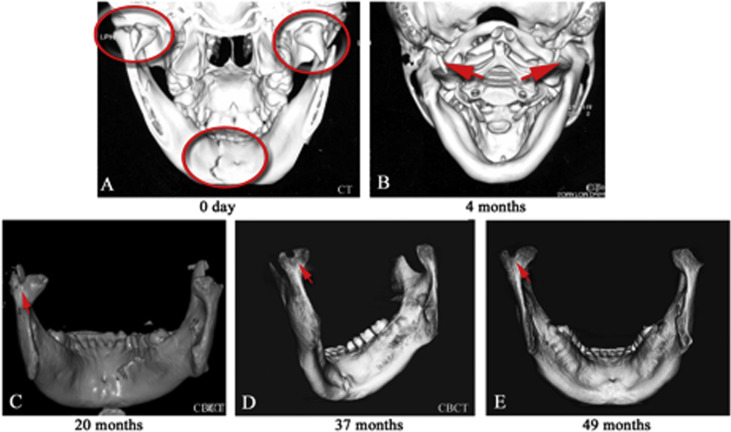
Clinical recovery was observed 2 months after treatment. At the follow-up appointments at 20, 37, and 49 months, jaw function and occlusal relationship remained stable, and no ankylosis was observed. The computed tomography scans showed that the right condyle had remodeled, and the left condyle exhibited a slight curve in the head at 49 months posttreatment. The patient’s satisfaction with these treatment results was high.
Conclusions
Conservative treatment of a mandibular fracture by fixed orthodontic means is a viable treatment option that is relatively straightforward and cost-effective and has a high level of patient acceptance and comfort.
Highlights
- •
A fixed orthodontic approach was used to treat a pediatric mandibular bilateral condylar fracture.
- •
This new conservative method is easy to handle by the orthodontist.
- •
The outcomes of jaw function, occlusion, and facial esthetics were good.
- •
No mandibular ankylosis was observed after 49 months of follow-up.
- •
This is a viable treatment option for mandibular condylar fractures.
The mandibular condyle is an important secondary growth center in the craniofacial region, adapting to different functional needs and maintaining the normal integrity of the joint during growth. In children, about 16% and 40% of facial and mandibular fractures, respectively, involve the condyle. Pediatric condylar fractures, if not properly managed, can easily lead to problems such as mandibular deficiency, facial asymmetry, and temporomandibular joint (TMJ) disorder on both the injured and the noninjured sides.
The degree of displacement of the condyles is determined by the direction, degree, magnitude, and precise point of application of the force, the state of the dentition, and the occlusal position. Most condylar fractures are caused by indirect forces transmitted to the condyle from a blow elsewhere, and traffic accidents, including bicycle crashes, are the main causes of these fractures in children. With adequate molar support and the teeth in occlusion, little or no displacement is likely to be sustained, whereas the full force will be transmitted to the condyles if the mouth is wide open.
Ongoing controversy exists on the management of pediatric mandibular condylar fractures. One approach is splint therapy. Two other approaches, differing in whether surgery is performed at the fracture site, are currently the treatments of choice. The conservative approach focuses on fixating the maxillomandibular relationship of the dental occlusion to place the fractured parts in a good relationship, leaving the fracture site untouched. To aid in healing, 2 to 4 weeks of intermaxillary fixation is usually initiated, followed by guiding elastics to bring the mandible into habitual occlusion, or by exercises aimed at restoring normal movement and occlusion. The second approach is to perform open reduction followed by rigid internal fixation to reposition and create a favorable condition for restoration of normal function. Open reduction and internal fixation may cause a growth disturbance from either the surgical manipulation of the fracture segments or the placement of rigid hardware across the condylar growth center and nerve. Because pediatric mandibular condylar fractures have a greater ability to remodel than do adult fractures, a conservative approach is often recommended. Here, we present a conservative approach whereby orthodontic treatment was used as an adjunct in the reduction of a bilateral condylar fracture in a 10-year-old boy.
Diagnosis
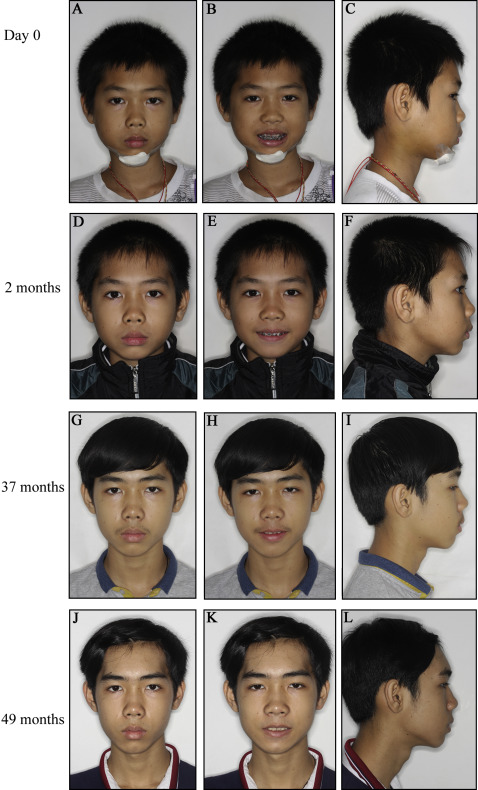
A boy, aged 10 years 9 months, came to the Affilicated Stomatology Hospital of Kunming Medical University in Kunming, China, 4 days after being injured in a car accident. He was transferred to the orthodontic department after he was seen at the Department of Oral and Maxillofacial Surgery of the hospital. He complained of facial pain and inability to chew and sleep well during the preceding 4 days. There was facial swelling on both sides and a shift of the mandibular facial midline to the left of about 2 mm ( Fig 1 , A – C ). Mouth opening was limited to 31 mm, with a mandibular deviation during opening and closure to the left. A chin laceration ( Fig 1 , A – C ) and fractures of both maxillary incisors were also observed ( Fig 2 , A – C ).

A computed tomograpy scan, known for its diagnostic accuracy, sensitivity, and specificity, was taken. It showed a vertical fracture on the left condylar head, a displaced fracture of the right condylar neck, and a mandibular symphysis fracture ( Fig 3 , A ). A total of 5 scans were taken; the first was at the time of diagnosis (day 0). The 4 subsequent scans were taken at 4, 20, 37, and 49 months after the initial treatment ( Fig 3 , B – D ) to monitor the healing of the fracture.
Treatment
The first goal of the treatment was to provide symptomatic relief and prevent infection. A therapy that consisted of antibiotics, anti-inflammatory analgesics, and a soft diet was immediately instituted. Lacerations on the chin were cleaned and sutured.
Two treatment options were presented to the parents: (1) open reduction and rigid maxillomandibular fixation, and (2) conservative treatment with an arch bar and intermaxillary fixation. The plan to use an arch bar included a 0.025-mm steel wire ligature on the surfaces of the maxillary and mandibular teeth and gingiva or screws inserted into the alveolar process between the roots of the canines and first premolars in both jaws. Guiding interarch elastics that would allow for some functional activity would subsequently be used for fixation for at least 2 weeks to guide the occlusion.
The family opted for a conservative approach with the goal of allowing condylar remodeling and the reestablishment of normal mandibular growth and occlusal development. However, during the consultation appointment when the treatment plan was presented, the patient exhibited severe anxiety about the arch bar. He was then referred to the orthodontic department for an alternative, less-invasive approach.
The patient’s facial analysis showed a convex profile and facial asymmetry with a mandibular shift of 2 mm to the left side ( Fig 1 , A – C ). He was in the early permanent dentition, with a Class II relationship that was more Class I in the molars and slightly Class II in the canines ( Fig 2 , A – C ). The maxillary incisor midline coincided with the facial midline, and the mandibular midline was shifted to the left by approximately 2 mm ( Fig 2 , B ).
As an alternative to arch bars, an orthodontic treatment option was presented and accepted by the patient and his family. Without local anesthesia or sedation, brackets (0.022-in slots) were placed on the maxillary second premolars (excluding the partially erupted canines) and the mandibular molars (excluding the partially erupted second premolars) from left to right ( Fig 2 ). An 0.018-in Australian wire was bent slightly to match the bracket level in each arch, and ligature wire loops or hooks on the brackets were used for elastic wear ( Fig 2 , A ). Intermaxillary elastics (1/8-in outer diameter, 3.5 oz; 3M ESPE, Monrovia, Calif) were then used from the maxillary to the mandibular teeth from 11 to 41, 12 to 42, 14 to 44, 15 to 45, 21 to 32, 22 to 33, 24 to 35, and 25 to 36 (Fédération Dentaire Inernationale tooth numbering system). Four rubber bands per side were found to be sufficient to provide a secure intermaxillary fixation. The rubber bands were changed at least once 1 day. The elastics were worn for 4 weeks. The patient was told not to open his mouth except for cleaning. A liquid diet was advised for the first 2 weeks.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


