Implant-supported dental restorations can be screw-retained, cement-retained, or a combination of both, whereby a metal superstructure is screwed to the implants and crowns are individually cemented to the metal frame. Each treatment modality has advantages and disadvantages. The use of computer-aided design/computer-assisted manufacture technologies for the manufacture of implant superstructures has proved to be advantageous in the quality of materials, precision of the milled superstructures, and passive fit. Maintenance and recall evaluations are an essential component of implant therapy. The longevity of implant restorations is limited by their biological and prosthetic maintenance requirements.
Key points
- •
When considering implant prosthodontic treatment for rehabilitation of the partially or fully edentulous patient, the clinician has several choices to choose from including, but not limited to:
- ○
Use of fixed or removable prostheses
- ○
Use of individual attachments or bars for retention of removable overdentures
- ○
Use of screw-retained or cement-retained prostheses
- ○
Use of stock versus custom abutments
- ○
Different restorative and abutment materials
- ○
- •
Implant-supported restorations can be screw-retained, cement-retained, or a combination of both, whereby a metal superstructure is screwed to the implants and crowns are individually cemented to the metal frame. Each treatment modality has advantages and disadvantages.
- •
Survival of zirconia abutments may be influenced by:
- ○
Manufacturing methods, and clinical and laboratory handling
- ○
The abutment wall thickness; a minimum wall thickness of 0.5 mm has been recommended
- ○
Implant-abutment connection
- ○
Aging of materials (low-temperature degradation)
- ○
Implant location
- ○
- •
The use of computer-aided design/computer-assisted manufacture technologies for the manufacture of implant superstructures has proved to be advantageous in the quality of materials, precision of the milled superstructures, and passive fit.
- •
Maintenance and recall evaluations are an essential component of implant therapy. The longevity of implant restorations is limited by their biological and prosthetic maintenance requirements.
Introduction
Current tooth-replacement strategies typically consider the alloplastic-integrated replacement of missing teeth using endosseous dental implants as a primary choice among available modes of therapy. Implants may help preserve adjacent teeth from long-term biological complications. Clinical data indicate that abutment teeth of fixed or removable prostheses are at increased risk for caries, pulp injury, or even tooth loss as a result of these complications. The use of implants improves the stability and retention of removable prostheses. Of importance, the prescription of dental implants provides an alternative for patients who desire a fixed prosthesis or are psychologically unable to accept a removable prosthesis.
Despite the favorable long-term outcomes achieved with prosthetic rehabilitations with implants, biological and technical complications are frequent. Systematic reviews of the survival and complications of implants and associated prostheses identified 6 categories of complications: surgical complications, implant loss, bone loss, peri-implant soft-tissue complications, mechanical complications, and aesthetic/phonetic complications. Such complications are affected by many factors, including the operator’s skills and judgments in treatment planning, prosthesis design, materials, patient-specific factors, and local and systemic conditions and habits such as bruxism, smoking, presence of periodontal disease, and maintenance. Prosthetically driven treatment planning for implant placement that is properly communicated to the surgeon is critical to ensure adequate restorative space for the various prosthetic designs, appropriate implant angulation, and minimizing cantilevers. Ultimately, long-term success of the fabricated prosthesis also relies on the patient’s commitment to proper hygiene measures and recall appointments to ensure good-quality maintenance of restorations.
When considering implant prosthodontic treatment for rehabilitation of the partially or fully edentulous patient, the clinician has several choices including, but not limited to:
- •
Use of fixed or removable prostheses
- •
Use of individual attachments or bars for retention of removable overdentures
- •
Use of screw-retained or cement-retained prostheses
- •
Use of stock versus custom abutments
- •
Different restorative and abutment materials
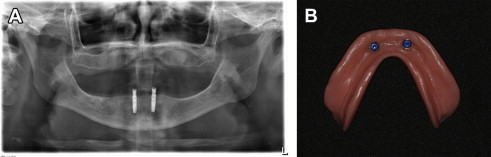
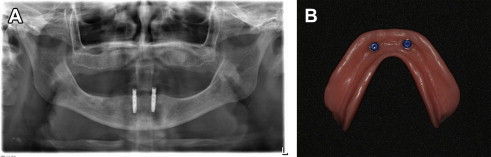
A consensus statement suggested the 2-implant–supported overdenture as the minimum standard of care for the edentulous mandible ( Fig. 1 ). In addition, maxillary removable overdentures may be considered as a satisfactory treatment option for patients with complaints about the retention and stability of their dentures. A main advantage of this treatment modality is hygiene access, in addition to providing proper lip support for patients with insufficient alveolar bone volume. Maxillary and mandibular removable overdentures are typically fabricated with acrylic resin prosthetic teeth processed on a rigid acrylic resin base that may be reinforced with a metal frame, often used for the maxillary overdentures with a horseshoe-shaped design ( Fig. 2 ). The use of metal reinforcement is advisable, owing to the frequent base fracture that may be encountered because of the reduced bulk of acrylic resin in accommodating the attachment systems. Overdentures can be retained either by bar-and-clip attachments or by nonsplinted magnets, locators, ball-and-clip attachments, or cone-shaped telescopic copings. Maintenance demands vary with the different prosthetic designs and attachments used.

The prosthodontic literature is controversial regarding the choice of splinted/unsplinted implants when used to retain maxillary overdentures. Unsplinted implant prostheses are less costly, provide easier access for cleaning, are less technique sensitive, and require less prosthetic space within the prostheses. An essential component for the use of either solitary attachments or bars is the restorative space required, which should be integrated in the treatment-planning phase to ensure the fabrication of durable restorations. The minimum vertical distance requirement from the implant platform to the incisal edges, as suggested by Phillips and Wong, is 13 to 14 mm when bars are used. By contrast, solitary attachments require only 10 to 11 mm ( Fig. 3 ). Implant angulation, however, plays a critical factor in the retention of solitary anchors, and surgeons should place implants in these cases with focused concern for parallelism.

When implant angulation is compromised, the use of either splinted designs involving bars or fabrication of custom anchors may be required. In a systematic review assessing differences between splinted and unsplinted oral implants for implant-retained overdentures. Stoumpis and Kohal reported no differences in implant survival rates or peri-implant outcome between splinted and unsplinted designs, although the bar-supported overdentures have been shown to need less prosthetic maintenance. The observed greater peri-implant mucosal inflammation beneath bar-retained overdentures indicates another important, yet manageable issue when bars are required.
The use of fixed prostheses for maxillary and mandibular complete and partial edentulism is documented in several systematic reviews and many prospective cohort investigations. The general observation of high implant survival (>90% at 5 years) is applicable to the range of applications, but reflects the careful nature of clinical investigations and the training of the investigators. When patients desire fixed prosthetic reconstruction to replace missing teeth, implants may be used. Guidelines that define the number of implants, the nature of the components, and the nature of the prosthetic construction remain incomplete and in flux.
Introduction
Current tooth-replacement strategies typically consider the alloplastic-integrated replacement of missing teeth using endosseous dental implants as a primary choice among available modes of therapy. Implants may help preserve adjacent teeth from long-term biological complications. Clinical data indicate that abutment teeth of fixed or removable prostheses are at increased risk for caries, pulp injury, or even tooth loss as a result of these complications. The use of implants improves the stability and retention of removable prostheses. Of importance, the prescription of dental implants provides an alternative for patients who desire a fixed prosthesis or are psychologically unable to accept a removable prosthesis.
Despite the favorable long-term outcomes achieved with prosthetic rehabilitations with implants, biological and technical complications are frequent. Systematic reviews of the survival and complications of implants and associated prostheses identified 6 categories of complications: surgical complications, implant loss, bone loss, peri-implant soft-tissue complications, mechanical complications, and aesthetic/phonetic complications. Such complications are affected by many factors, including the operator’s skills and judgments in treatment planning, prosthesis design, materials, patient-specific factors, and local and systemic conditions and habits such as bruxism, smoking, presence of periodontal disease, and maintenance. Prosthetically driven treatment planning for implant placement that is properly communicated to the surgeon is critical to ensure adequate restorative space for the various prosthetic designs, appropriate implant angulation, and minimizing cantilevers. Ultimately, long-term success of the fabricated prosthesis also relies on the patient’s commitment to proper hygiene measures and recall appointments to ensure good-quality maintenance of restorations.
When considering implant prosthodontic treatment for rehabilitation of the partially or fully edentulous patient, the clinician has several choices including, but not limited to:
- •
Use of fixed or removable prostheses
- •
Use of individual attachments or bars for retention of removable overdentures
- •
Use of screw-retained or cement-retained prostheses
- •
Use of stock versus custom abutments
- •
Different restorative and abutment materials
A consensus statement suggested the 2-implant–supported overdenture as the minimum standard of care for the edentulous mandible ( Fig. 1 ). In addition, maxillary removable overdentures may be considered as a satisfactory treatment option for patients with complaints about the retention and stability of their dentures. A main advantage of this treatment modality is hygiene access, in addition to providing proper lip support for patients with insufficient alveolar bone volume. Maxillary and mandibular removable overdentures are typically fabricated with acrylic resin prosthetic teeth processed on a rigid acrylic resin base that may be reinforced with a metal frame, often used for the maxillary overdentures with a horseshoe-shaped design ( Fig. 2 ). The use of metal reinforcement is advisable, owing to the frequent base fracture that may be encountered because of the reduced bulk of acrylic resin in accommodating the attachment systems. Overdentures can be retained either by bar-and-clip attachments or by nonsplinted magnets, locators, ball-and-clip attachments, or cone-shaped telescopic copings. Maintenance demands vary with the different prosthetic designs and attachments used.

The prosthodontic literature is controversial regarding the choice of splinted/unsplinted implants when used to retain maxillary overdentures. Unsplinted implant prostheses are less costly, provide easier access for cleaning, are less technique sensitive, and require less prosthetic space within the prostheses. An essential component for the use of either solitary attachments or bars is the restorative space required, which should be integrated in the treatment-planning phase to ensure the fabrication of durable restorations. The minimum vertical distance requirement from the implant platform to the incisal edges, as suggested by Phillips and Wong, is 13 to 14 mm when bars are used. By contrast, solitary attachments require only 10 to 11 mm ( Fig. 3 ). Implant angulation, however, plays a critical factor in the retention of solitary anchors, and surgeons should place implants in these cases with focused concern for parallelism.

When implant angulation is compromised, the use of either splinted designs involving bars or fabrication of custom anchors may be required. In a systematic review assessing differences between splinted and unsplinted oral implants for implant-retained overdentures. Stoumpis and Kohal reported no differences in implant survival rates or peri-implant outcome between splinted and unsplinted designs, although the bar-supported overdentures have been shown to need less prosthetic maintenance. The observed greater peri-implant mucosal inflammation beneath bar-retained overdentures indicates another important, yet manageable issue when bars are required.
The use of fixed prostheses for maxillary and mandibular complete and partial edentulism is documented in several systematic reviews and many prospective cohort investigations. The general observation of high implant survival (>90% at 5 years) is applicable to the range of applications, but reflects the careful nature of clinical investigations and the training of the investigators. When patients desire fixed prosthetic reconstruction to replace missing teeth, implants may be used. Guidelines that define the number of implants, the nature of the components, and the nature of the prosthetic construction remain incomplete and in flux.
Cement-retained and screw-retained prostheses
Implant-supported restorations can be screw-retained (see Fig. 4 ), cement-retained (see Fig. 5 ), or a combination of both, whereby a metal superstructure is screwed to the implants and crowns are individually cemented to the metal frame. Each treatment modality has advantages and disadvantages.
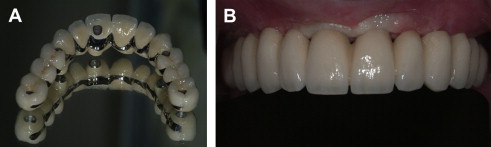
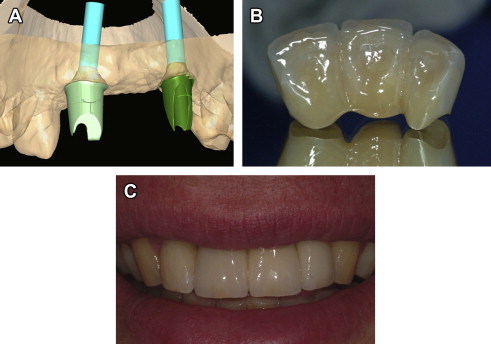
The use of screw-retained restorations provides clinicians with the accessibility of retrieving these restorations if needed for repairs, hygiene, and abutment-screw tightening. If implants are improperly positioned, screw-access holes may compromise aesthetics and occlusion because of the wear of restorative materials used to cover the screw-access channel. A possible complication of screw-retained prostheses is porcelain fracture at the screw-access channel resulting from unsupported porcelain. Ultimately, proactive planning and involvement of the restorative dentist in determining implant positions initially through the diagnostic wax-up phase, and digital planning with the use of cone-beam computed tomography, has become a critical factor in determining the feasibility of this restorative choice and its long-term success.
Cement-retained restorations may offer aesthetic advantages when access holes are visible facially and occlusally (see Fig. 5 ). These restorations may be simpler to fabricate, and provide easier insertion in posterior areas of the mouth for patients with limited jaw openings. In addition, for an implant-supported fixed-denture prosthesis (FDP), the potential for achieving a passive fit is higher with cement-retained restorations. Elements that are important for the retention of the cement-retained restorations are essentially the same as those for natural teeth; including taper of axial walls, surface area, height of the abutment, roughness of the surface, and type of cement. Most abutments are manufactured to approximately a 6° taper, which has been considered optimal for crown preparation. The minimum abutment height for use of cement-retained restorations with predictable retention was documented as 5 mm. Direct screw fixation at the implant level may be advisable in these instances when the interocclusal space is as little as 4 mm (limited interarch space) ( Fig. 6 ).
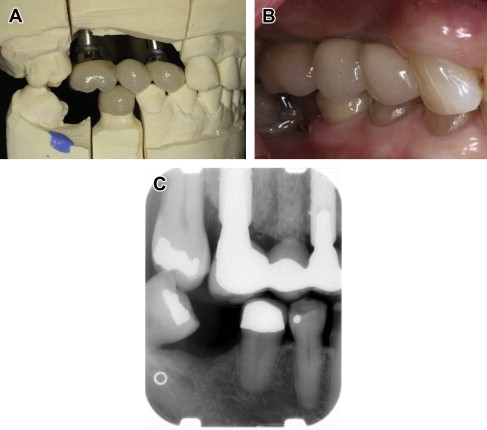
The main drawbacks of cement-retained restorations are difficult retrievability and retention of excess cement, especially when the restoration margins are placed subgingivally or the implants are deeply placed. Diligence in cement removal at time of cementation is critical. The presence of cement residue can be detrimental to peri-implant health ( Fig. 7 ). Residue can cause peri-implant inflammation associated with swelling, soreness, deeper probing depths, bleeding and/or exudation on probing, with radiographic evidence of peri-implant bone loss, and may eventually result in implant loss. A prospective endoscopic clinical study showed that excess cement was associated with signs of peri-implant disease in the majority of cases investigated (81%).
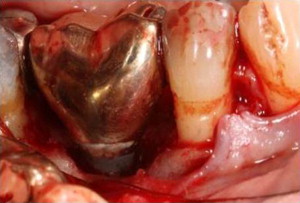
Agar and colleagues demonstrated that when the restorative margins of the abutments are placed 1.5 to 3 mm subgingival, the likelihood of leaving excess cement occurs. Use of screw-retained restorations or custom abutments for cement restorations with higher margins may be used to avoid cement-related complications in situations where implants are deeply placed.
Several techniques have been proposed to help clinicians in eliminating the presence of cement in the peri-implant sulcus, including:
- •
Using plastic scalers
- •
Reducing the amount of cement placed in the restorations
- •
Seating the restoration after placing the cement on the fitting surface on the abutment analog before cementing the restoration intraorally
- •
Creating a lingual vent hole in the implant-supported crowns
- •
Using an internal abutment space as a means of decreasing the extrusion of excess cement
Radiographic examination should only be a supplementary method for detection of excess cement. Radiographic density of many implant restorative cements is poor and depends on the thickness of the extruded cement, and radiographic examination cannot be trusted to detect residues of excess cement, especially when present on the facial or lingual aspects of the implant.
Consensus statements from the third consensus conference of the European Association for Osseointegration concluded that both types of reconstructions influenced the clinical outcomes, but none of the fixation methods was clearly advantageous. Cemented and screw-retained single-unit reconstructions had similar survival rates for their supporting implants, whereas cemented multiunit reconstructions had lower survival rates than the screw-retained multiunit reconstructions for their supporting implants. It is important to consider, however, that screw-retained single-unit and multiunit reconstructions tended to have lower reconstruction survival rates. Cemented reconstructions more frequently exhibited serious biological complications (bone loss >2 mm), which may reflect abutment design, margin location, or cement extrusion. The risk for this complication increased with the span of the reconstruction. Clinicians should weigh the advantages and disadvantages of cement-retained and screw-retained types of restorations, so as to select the most appropriate for a given clinical situation. If feasible, long-span and full-arch FDPs as well as riskier cantilever FDPs may be best treated with the screw-retained option, as the complications of these restorations are more frequent.
Selection of abutments
The main principles for selecting the appropriate abutment should be aimed to allow for:
- •
A proper biological response of the tissues
- •
Provision of the retention and resistance forms essential for cement-retained restorations
- •
Mechanical strength adequate enough to tolerate fatigue and loading
- •
Accurate fit with their mating implants
- •
Achievement of an adequate aesthetic result using the proper emergence profile and abutment material
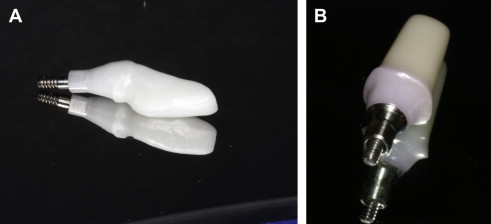
Abutments used in cement-retained implant restorations maybe either stock prefabricated abutments or customized abutments. Several materials have been used, including metal cast with gold alloys, titanium, alumina, and zirconia. In contrast to stock abutments, customized abutments, either cast or built using computer-aided design/computer-assisted manufacture (CAD/CAM), can be made to approximate natural tooth morphology, thereby increasing the total surface area, improving crown retention, and providing a form that supports peri-implant gingival tissue. Moreover, CAD/CAM abutments have advantages over cast abutments including their reduced cost, elimination of the dimensional inaccuracies associated with the casting process, and elimination of the need for additional reductions in stock zirconia abutments that may compromise their strength.
Available clinical data presume that metal abutments made of titanium represent a ‘benchmark’ with few technical complications the exception being loosening of the abutment screw. One limitation often encountered with the use of metal abutments is the gray discoloration of the peri-implant mucosa in patients with thin tissue biotype. This phenomenon affects aesthetically sensitive areas, especially for patients with a high smile line. In addition, soft-tissue recession in some patients can yield the gray titanium color, which could lead to aesthetic failure of the reconstruction. Ceramic abutments made of high-strength alumina and, more recently, zirconia were developed in efforts to overcome the graying phenomenon associated with metal abutments.
In a spectrophotometric analysis of the color change of the peri-implant soft tissue with different materials, Bressan and colleagues demonstrated that while the color of the soft tissue around titanium implants differed significantly from the gingival color around natural teeth, no significant differences were present in the color performance of abutments made of gold and zirconium oxide. Ultimately, manufacturers developed titanium abutments with nitride coatings that have a gold-shaded hue. These abutments can best be used as an alternative to ceramic abutments in cases with high aesthetic demands.
Analysis of the data collected from clinical settings using ceramic abutments demonstrated a poor performance for alumina abutments; they exhibited a high failure rate, with fracture in 7% of single-implant cases and 1.9% of implant-supported FDPs. Hence, the higher-strength zirconia with a bending strength of 900 MPa (574 MPa for alumina) and fracture toughness of 9 MPa m 1/2 (3.55 MPa m 1/2 for alumina) may be considered a better choice when ceramic abutments are to be used.
Survival of zirconia abutments may be influenced by :
- •
Manufacturing methods, and clinical and laboratory handling
- •
The abutment-wall thickness; a minimum wall thickness of 0.5 mm has been recommended
- •
Implant-abutment connection
- •
Aging of materials (low-temperature degradation)
- •
Implant location
In internal-connection implants, the zirconia abutments can be connected either internally to the implant as one piece by the abutment itself or via a secondary titanium metallic component ( Fig. 8 ). Preliminary in vitro data suggested that superior strength maybe achieved by means of internal connection via a secondary metallic component. However, in vivo data are still lacking.