The clinical success and longevity of indirect restorations depend on the careful and accurate completion of several procedures. One of the challenging procedures is management of the gingival tissues and gingival esthetics. The goal for management of gingival tissues and gingival esthetics is to maintain the normal appearance of healthy gingival. Achieving this goal requires optimal health before treatment and minimal trauma during treatment. The best way of optimizing health and minimizing trauma is to avoid contacting the gingiva with restorative materials.
Key points
- •
Periodontal health and biotype needs to be evaluated and respected in order to preserve gingival position and form.
- •
Care must be taken not to violate the biologic width during definitive impression making.
- •
Tissue displacement must be gentle.
- •
Several techniques for tissue displacement are available.
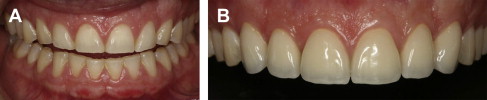
The clinical success and longevity of indirect restorations depend on the careful and accurate completion of several procedures. One of the challenging procedures is management of the gingival tissues and gingival esthetics. The goal for management of gingival tissues and gingival esthetics is to maintain the normal appearance of healthy gingiva ( Figs. 1 and 2 ). Achieving this goal requires optimal health before treatment and minimal trauma during treatment. The best way of optimizing health and minimizing trauma is to avoid contacting the gingiva with restorative materials. However, for esthetic or functional reasons, restoration margins are frequently located within the gingival sulcus. One disadvantage of subgingival margins is that they have the tendency to increase the potential for periodontal problems (gingival inflammation). However, periodontal health can be maintained in the presence of subgingival margins but it requires careful execution of the clinical procedures and well-fitting, properly contoured crowns. Appropriate, reversible, gingival displacement and tissue management are required, which facilitates making the final impression so it accurately records the prepared finish line and some unprepared tooth structure apical to the finish line. The dies will thereby be true replicas of the prepared tooth. This article reviews the factors governing the preservation of gingival position and form along with contemporary and traditional techniques and materials available to obtain a minimally invasive and tissue friendly gingival displacement that preserves periodontal health while facilitating impression making.

Factors governing the preservation of gingival position and form
Pretreatment Periodontal Health/Periodontal Biotype
Before attempting to perform any gingival displacement technique, it is important to assess the periodontal health of the tooth or teeth involved. Healthy, firm, nonbleeding tissues should be present so there is an optimal intrasulcular environment. Gingiva that is damaged or inflamed is more susceptible to bleeding, which makes it more challenging to obtain optimal accuracy in the impression, especially when a hydrophobic impression material is being used.
The first step in periodontal evaluation of teeth should include an examination of the periapical and/or bitewing radiographs to determine the position of the alveolar crestal bone height and to rule out any pathologic abnormality. Undetected defects in the bone, such as angular bone loss or infrabony pockets, may lead to increased hemorrhage during the procedure and future tissue instability as a result of tissue manipulation in these areas. Therefore, a thorough radiographic examination is an integral component of a pretreatment periodontal evaluation.
The second step is to evaluate the periodontium visually. The color, contour, consistency, position, surface texture, and presence of pain should be evaluated to determine if the gingiva is healthy. The gingival index is a valuable tool in gauging tissue condition. Studies found an elevated gingival index in sulci where displacement cords were packed, suggesting injury of the periodontium. All tissue displacement techniques produce trauma to the gingival tissue caused by mechanical or chemical trauma that creates an inflammatory response. In vitro studies found that displacement cords combined with chemical displacement agents were cytotoxic to the gingival fibroblasts. However, the injury inflicted by displacement cords is self-limited and reversible.
The oral environment of some patients resists the trauma of prosthodontic procedures better than other patients. Slight trauma will usually not produce lasting effects if the gingiva is healthy before the treatment, whereas existing periodontal abnormalities cause exaggerated responses to the slightest tissue insults.
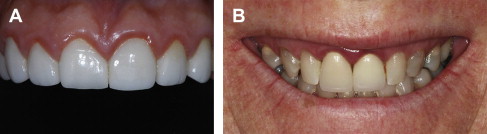
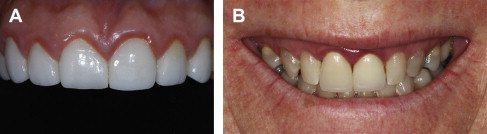
The third step in the pretreatment evaluation is to measure the sulcus depth. Teeth that require gingival displacement procedures will typically have their preparation finish lines located approximately 0.5 to 1.0 mm subgingivally and ideally within the sulcus. An attempt should be made to control the apical extension of the gingival manipulation so as to avoid placing the finish line apical to the base of the gingival sulcus, into the epithelial and connective tissue attachments. Therefore, careful measurement of sulcus depth with a periodontal probe should be made and recorded to calculate how deep the finish line should be placed and how much displacement is possible or necessary to maintain the harmony of the periodontium. Accelerated bone loss could not be documented in a critical evaluation of available evidence because commonly reported changes in probing depths were less than 1 mm, a dimension smaller than the probing accuracy of clinicians. Therefore, subgingival margins most commonly result in negative esthetic changes in the gingiva rather than accelerated bone loss ( Fig. 3 ).
When choosing a displacement technique, it is also important to identify the type of tissue being manipulated. Periodontal biotypes were first described by Ochsenbein and Ross in 1969. Two biotypes have been described, the thick, flat biotype and the thin, scalloped biotype. They are terms that have been used to describe the tissue thickness and the amount of scalloping of the interdental papilla in different individuals.
In the thick, flat biotype, there is minimal to moderate distance between the location of the midfacial gingival crest and the height of the interproximal papilla (one-half or less of the incisocervical crown dimension). The gingiva is thicker, more fibrotic with an increase in quantity and quality of masticatory mucosa. There is also a greater probing depth and the gingival margin is usually located on enamel. The distance between the cemento-enamel junction (CEJ) and the bony crest is about 2 mm. In addition, the underlying bone has limited scalloping and there are usually no bony dehiscences or fenestrations ( Fig. 4 ).

The thin, scalloped biotype presents with thin, delicate gingiva, a limited amount of attached gingiva, and the quality of that present is not ideal. The probing depth is shallow and the gingival margin is frequently not on enamel. It is located at the CEJ or on the root surface with pretreatment recession. There is an increased distance (approximately 4 mm) between the CEJ and the bone. The underlying bone is scalloped, and bony dehiscences and/or fenestrations are often present. One of the characteristics of the thin biotype is that there is a substantial difference between the location of the midfacial gingival crest and the height of the interproximal papilla (a dimension that can equal more than one-half of the incisocervical crown dimension). Thin biotypes present with an acute “gingival angle.” This angle is formed by lines connecting the most apical location of facial gingiva and the most coronal papillae heights. In the thin biotype there may be recession present in the absence of any dental restorations, indicating that subgingival restorations are likely to create further recession. It is more difficult to have interdental papilla that fills spaces around both teeth and implants ( Fig. 5 ).

A clinical study by Olsson and colleagues evaluated photographically the periodontal characteristics in 113 individuals with varying forms of the maxillary central incisors. They found that individuals with tapered coronal outline forms of maxillary central incisors experienced more gingival recession on facial surfaces. They also determined that maxillary central incisor crown outline form can be used to differentiate between biotypes.
In another study on the relationship between form and clinical features of the gingiva, Olsson and Lindhe examined 108 adolescents between the ages of 16 and 19 lacking any signs of destructive periodontal disease. They found the tapered crown form had greater papilla height and more acute gingival angle (75°–78° vs 87°–97°) than square teeth. Square maxillary central incisor crown forms had significantly wider zones of keratinized gingiva and probing depths were significantly greater. However, they found no significant difference between free gingival thickness and the cervical crown convexity. In the presence of a susceptible environment due to the presence of a thin, scalloped periodontal biotype, it is especially important that oral hygiene be optimized before the initiation of prosthodontic procedures.
Biologic Width
To understand the nature of gingival displacement techniques fully, first the natural state of the periodontium and its relationship with the dentition must be appreciated. To accomplish this, one must understand the components of the physiologic dentogingival complex. It is a proportional relationship between the alveolar bone crest, connective tissue attachment, the epithelial attachment, and the sulcus depth. The alveolar bone crest describes the most coronally positioned portion of the alveolar process. Many connective tissue fibers attach to this portion of bone and it serves as the main bony housing for the teeth. The connective tissue attachment is also referred to as gingival connective tissue and the lamina propria. It consists of 2 layers. The first is the reticular layer, which lies adjacent to the periosteum that connects to the alveolar bone. The second is a papillary layer that is characterized by papillary projections that are woven in between the epithelial rete pegs. The epithelial attachment is the zone of attachment that contains the junctional epithelium and usually ranges from 0.25 to 1.35 mm in length. This type of epithelium regenerates after surgical interventions. It is connected to both enamel and cementum by relatively weak adhesions called hemidesmosomes. The gingival sulcus is the thin, V-shaped space that is found between the free gingiva and the surface of the tooth. The depth of the sulcus is susceptible to change, dependent on the amount of inflammation of gingival tissue. It has been reported that a normal depth of the sulcus falls in the range of 0.5 to 1 mm.
The concept of “biologic width” began with Gargiulo and colleagues in 1961 when they described findings after examining the physiologic dentogingival complex in 30 human cadavers for a total of 287 teeth. It was reported that the average measurement for sulcus depth was 0.69 mm, the epithelial attachment was 0.97 mm, and the connective tissue attachment was 1.07 mm. Thus, it has been commonly stated that based on this research, the biologic width is 2.04 mm. However, other studies have also shown that there is a wide variance in the length of the epithelial attachment, ranging from 1.0 to 9.0 mm. Based on Gargiulo’s concept, Cohen coined the term “biologic width” for a lecture discussing the periodontal preparation of the mouth for prosthodontic procedures. Although the exact dimensions of the “biologic width” can be different from person to person, it is widely accepted that restorations should not extend beyond 0.5 to 1.0 mm into the gingival sulcus. It is of integral importance to the maintenance of the healthy periodontium that no restorative effort violates the junctional epithelium or connective tissue fiber apparatus. Furthermore, the authors also suggested maintaining a 3.0-mm safety zone between the crest of the alveolar bone and the margin of a crown. Because it is not possible to detect clinically, through tactile sensation, where the sulcus ends and the junctional epithelium begins, the authors suggested that this zone of safety be recommended.
The consequences of violating the biologic width have been described in the dental literature. If the margins of dental restorations were to extend into the junctional epithelium or beyond, marginal and papillary gingivitis can be observed. Furthermore, this condition can lead to chronic inflammation and progress to periodontitis.
Displacement Cord Positioning Force
Minimally traumatic tissue displacement is necessary to maintain a healthy periodontium that plays an important role in the survival rate of fixed restorations. Exerting heavy force to position gingival displacement cord can cause injury to the crevicular epithelium, the junctional epithelium, and the supra-alveolar connective tissue fibers ( Fig. 6 ). Heavy forces might also injure the periodontal fibers and disturb the blood supply. Löe and Silness showed that heavy forces during positioning of displacement cord could destroy the uppermost Sharpey fiber. As a result, gingival recession can be observed, and occasionally, loss of attachment. Only one study measured the amount of pressure generated by displacement cords or cordless displacement. They found that the pressure generated by displacement cords (5396 KPa) is significantly higher than the one generated by cordless displacement (143 KPa) when using a thick, firm, and viscous paste, containing chloride. Clinicians have the tendency to apply more force when the patient is anesthetized and does not feel any pressure and/or pain during cord placement.

Displacement Time
The amount of time that a cord should be allowed to remain in the sulcus is an important factor. The goal of the clinician is to leave the cord long enough to create adequate displacement of the gingiva for impression making. However, to preserve periodontal health, it is also important not to leave the cord in the sulcus too long. Studies demonstrated no prolonged harmful effects of the epithelial attachment when the cords are placed in the sulcus in a careful manner for a reasonable time, and healthy gingival tissues will heal in a few days. Anneroth and Nordenram showed that dry cords placed in the sulcus adhere to the crevicular epithelium. When the cord is removed before impression making, the crevicular epithelium is torn and removed, thereby inducing a wound-healing reaction.
The amount of time needed for cords to remain in the sulcus has been evaluated by several authors and was found to range from 1 minute to 30 minutes. Fischer recommended the use of a cord impregnated with ferric sulfate (FS) for 1 minute to provide the amount of displacement needed. Baharav and colleagues tested a 2-cord technique for tissue displacement and concluded that the cords need to stay in the sulcus for 4 minutes before impression-making to produce sufficient crevicular width expansion. Benson and colleagues found that 10 to 20 minutes of gingival displacement will allow the clinician enough time (30 minutes) to make multiple impressions. In a dog study, Harrison concluded that nonmedicated cord was safely used for up to 30 minutes. There is no long-term damage to the periodontal tissue when short placement times are used, provided the healing process is not disturbed. Ramadan and colleagues showed that cords placed no longer that 3 minutes in the sulcus will allow the clinician to get adequate healing. Several studies demonstrated that displacement cords cause destruction of the junctional epithelium that takes between 5 and 14 days to heal. Although precise time recommendations are not available, the above studies reveal the importance of reducing gingival displacement as much as possible.
Based on the total time of retraction, it is important to consider the protocol to be used carefully when a large number of teeth are being prepared in the presence of a thin biotype. It might be prudent to prepare one tooth to completion with cord present, then remove the cord and move to the next tooth. After all the teeth are prepared, then repack the previously prepared teeth rather than leave the cord in the sulcus of the first prepared teeth while the remainder is being prepared.
Factors governing the preservation of gingival position and form
Pretreatment Periodontal Health/Periodontal Biotype
Before attempting to perform any gingival displacement technique, it is important to assess the periodontal health of the tooth or teeth involved. Healthy, firm, nonbleeding tissues should be present so there is an optimal intrasulcular environment. Gingiva that is damaged or inflamed is more susceptible to bleeding, which makes it more challenging to obtain optimal accuracy in the impression, especially when a hydrophobic impression material is being used.
The first step in periodontal evaluation of teeth should include an examination of the periapical and/or bitewing radiographs to determine the position of the alveolar crestal bone height and to rule out any pathologic abnormality. Undetected defects in the bone, such as angular bone loss or infrabony pockets, may lead to increased hemorrhage during the procedure and future tissue instability as a result of tissue manipulation in these areas. Therefore, a thorough radiographic examination is an integral component of a pretreatment periodontal evaluation.
The second step is to evaluate the periodontium visually. The color, contour, consistency, position, surface texture, and presence of pain should be evaluated to determine if the gingiva is healthy. The gingival index is a valuable tool in gauging tissue condition. Studies found an elevated gingival index in sulci where displacement cords were packed, suggesting injury of the periodontium. All tissue displacement techniques produce trauma to the gingival tissue caused by mechanical or chemical trauma that creates an inflammatory response. In vitro studies found that displacement cords combined with chemical displacement agents were cytotoxic to the gingival fibroblasts. However, the injury inflicted by displacement cords is self-limited and reversible.
The oral environment of some patients resists the trauma of prosthodontic procedures better than other patients. Slight trauma will usually not produce lasting effects if the gingiva is healthy before the treatment, whereas existing periodontal abnormalities cause exaggerated responses to the slightest tissue insults.
The third step in the pretreatment evaluation is to measure the sulcus depth. Teeth that require gingival displacement procedures will typically have their preparation finish lines located approximately 0.5 to 1.0 mm subgingivally and ideally within the sulcus. An attempt should be made to control the apical extension of the gingival manipulation so as to avoid placing the finish line apical to the base of the gingival sulcus, into the epithelial and connective tissue attachments. Therefore, careful measurement of sulcus depth with a periodontal probe should be made and recorded to calculate how deep the finish line should be placed and how much displacement is possible or necessary to maintain the harmony of the periodontium. Accelerated bone loss could not be documented in a critical evaluation of available evidence because commonly reported changes in probing depths were less than 1 mm, a dimension smaller than the probing accuracy of clinicians. Therefore, subgingival margins most commonly result in negative esthetic changes in the gingiva rather than accelerated bone loss ( Fig. 3 ).
When choosing a displacement technique, it is also important to identify the type of tissue being manipulated. Periodontal biotypes were first described by Ochsenbein and Ross in 1969. Two biotypes have been described, the thick, flat biotype and the thin, scalloped biotype. They are terms that have been used to describe the tissue thickness and the amount of scalloping of the interdental papilla in different individuals.
In the thick, flat biotype, there is minimal to moderate distance between the location of the midfacial gingival crest and the height of the interproximal papilla (one-half or less of the incisocervical crown dimension). The gingiva is thicker, more fibrotic with an increase in quantity and quality of masticatory mucosa. There is also a greater probing depth and the gingival margin is usually located on enamel. The distance between the cemento-enamel junction (CEJ) and the bony crest is about 2 mm. In addition, the underlying bone has limited scalloping and there are usually no bony dehiscences or fenestrations ( Fig. 4 ).

The thin, scalloped biotype presents with thin, delicate gingiva, a limited amount of attached gingiva, and the quality of that present is not ideal. The probing depth is shallow and the gingival margin is frequently not on enamel. It is located at the CEJ or on the root surface with pretreatment recession. There is an increased distance (approximately 4 mm) between the CEJ and the bone. The underlying bone is scalloped, and bony dehiscences and/or fenestrations are often present. One of the characteristics of the thin biotype is that there is a substantial difference between the location of the midfacial gingival crest and the height of the interproximal papilla (a dimension that can equal more than one-half of the incisocervical crown dimension). Thin biotypes present with an acute “gingival angle.” This angle is formed by lines connecting the most apical location of facial gingiva and the most coronal papillae heights. In the thin biotype there may be recession present in the absence of any dental restorations, indicating that subgingival restorations are likely to create further recession. It is more difficult to have interdental papilla that fills spaces around both teeth and implants ( Fig. 5 ).

A clinical study by Olsson and colleagues evaluated photographically the periodontal characteristics in 113 individuals with varying forms of the maxillary central incisors. They found that individuals with tapered coronal outline forms of maxillary central incisors experienced more gingival recession on facial surfaces. They also determined that maxillary central incisor crown outline form can be used to differentiate between biotypes.
In another study on the relationship between form and clinical features of the gingiva, Olsson and Lindhe examined 108 adolescents between the ages of 16 and 19 lacking any signs of destructive periodontal disease. They found the tapered crown form had greater papilla height and more acute gingival angle (75°–78° vs 87°–97°) than square teeth. Square maxillary central incisor crown forms had significantly wider zones of keratinized gingiva and probing depths were significantly greater. However, they found no significant difference between free gingival thickness and the cervical crown convexity. In the presence of a susceptible environment due to the presence of a thin, scalloped periodontal biotype, it is especially important that oral hygiene be optimized before the initiation of prosthodontic procedures.
Biologic Width
To understand the nature of gingival displacement techniques fully, first the natural state of the periodontium and its relationship with the dentition must be appreciated. To accomplish this, one must understand the components of the physiologic dentogingival complex. It is a proportional relationship between the alveolar bone crest, connective tissue attachment, the epithelial attachment, and the sulcus depth. The alveolar bone crest describes the most coronally positioned portion of the alveolar process. Many connective tissue fibers attach to this portion of bone and it serves as the main bony housing for the teeth. The connective tissue attachment is also referred to as gingival connective tissue and the lamina propria. It consists of 2 layers. The first is the reticular layer, which lies adjacent to the periosteum that connects to the alveolar bone. The second is a papillary layer that is characterized by papillary projections that are woven in between the epithelial rete pegs. The epithelial attachment is the zone of attachment that contains the junctional epithelium and usually ranges from 0.25 to 1.35 mm in length. This type of epithelium regenerates after surgical interventions. It is connected to both enamel and cementum by relatively weak adhesions called hemidesmosomes. The gingival sulcus is the thin, V-shaped space that is found between the free gingiva and the surface of the tooth. The depth of the sulcus is susceptible to change, dependent on the amount of inflammation of gingival tissue. It has been reported that a normal depth of the sulcus falls in the range of 0.5 to 1 mm.
The concept of “biologic width” began with Gargiulo and colleagues in 1961 when they described findings after examining the physiologic dentogingival complex in 30 human cadavers for a total of 287 teeth. It was reported that the average measurement for sulcus depth was 0.69 mm, the epithelial attachment was 0.97 mm, and the connective tissue attachment was 1.07 mm. Thus, it has been commonly stated that based on this research, the biologic width is 2.04 mm. However, other studies have also shown that there is a wide variance in the length of the epithelial attachment, ranging from 1.0 to 9.0 mm. Based on Gargiulo’s concept, Cohen coined the term “biologic width” for a lecture discussing the periodontal preparation of the mouth for prosthodontic procedures. Although the exact dimensions of the “biologic width” can be different from person to person, it is widely accepted that restorations should not extend beyond 0.5 to 1.0 mm into the gingival sulcus. It is of integral importance to the maintenance of the healthy periodontium that no restorative effort violates the junctional epithelium or connective tissue fiber apparatus. Furthermore, the authors also suggested maintaining a 3.0-mm safety zone between the crest of the alveolar bone and the margin of a crown. Because it is not possible to detect clinically, through tactile sensation, where the sulcus ends and the junctional epithelium begins, the authors suggested that this zone of safety be recommended.
The consequences of violating the biologic width have been described in the dental literature. If the margins of dental restorations were to extend into the junctional epithelium or beyond, marginal and papillary gingivitis can be observed. Furthermore, this condition can lead to chronic inflammation and progress to periodontitis.
Displacement Cord Positioning Force
Minimally traumatic tissue displacement is necessary to maintain a healthy periodontium that plays an important role in the survival rate of fixed restorations. Exerting heavy force to position gingival displacement cord can cause injury to the crevicular epithelium, the junctional epithelium, and the supra-alveolar connective tissue fibers ( Fig. 6 ). Heavy forces might also injure the periodontal fibers and disturb the blood supply. Löe and Silness showed that heavy forces during positioning of displacement cord could destroy the uppermost Sharpey fiber. As a result, gingival recession can be observed, and occasionally, loss of attachment. Only one study measured the amount of pressure generated by displacement cords or cordless displacement. They found that the pressure generated by displacement cords (5396 KPa) is significantly higher than the one generated by cordless displacement (143 KPa) when using a thick, firm, and viscous paste, containing chloride. Clinicians have the tendency to apply more force when the patient is anesthetized and does not feel any pressure and/or pain during cord placement.

Displacement Time
The amount of time that a cord should be allowed to remain in the sulcus is an important factor. The goal of the clinician is to leave the cord long enough to create adequate displacement of the gingiva for impression making. However, to preserve periodontal health, it is also important not to leave the cord in the sulcus too long. Studies demonstrated no prolonged harmful effects of the epithelial attachment when the cords are placed in the sulcus in a careful manner for a reasonable time, and healthy gingival tissues will heal in a few days. Anneroth and Nordenram showed that dry cords placed in the sulcus adhere to the crevicular epithelium. When the cord is removed before impression making, the crevicular epithelium is torn and removed, thereby inducing a wound-healing reaction.
The amount of time needed for cords to remain in the sulcus has been evaluated by several authors and was found to range from 1 minute to 30 minutes. Fischer recommended the use of a cord impregnated with ferric sulfate (FS) for 1 minute to provide the amount of displacement needed. Baharav and colleagues tested a 2-cord technique for tissue displacement and concluded that the cords need to stay in the sulcus for 4 minutes before impression-making to produce sufficient crevicular width expansion. Benson and colleagues found that 10 to 20 minutes of gingival displacement will allow the clinician enough time (30 minutes) to make multiple impressions. In a dog study, Harrison concluded that nonmedicated cord was safely used for up to 30 minutes. There is no long-term damage to the periodontal tissue when short placement times are used, provided the healing process is not disturbed. Ramadan and colleagues showed that cords placed no longer that 3 minutes in the sulcus will allow the clinician to get adequate healing. Several studies demonstrated that displacement cords cause destruction of the junctional epithelium that takes between 5 and 14 days to heal. Although precise time recommendations are not available, the above studies reveal the importance of reducing gingival displacement as much as possible.
Based on the total time of retraction, it is important to consider the protocol to be used carefully when a large number of teeth are being prepared in the presence of a thin biotype. It might be prudent to prepare one tooth to completion with cord present, then remove the cord and move to the next tooth. After all the teeth are prepared, then repack the previously prepared teeth rather than leave the cord in the sulcus of the first prepared teeth while the remainder is being prepared.
Materials for tissue displacement
Displacement Cords
The use of displacement cord is the most popular method for tissue displacement in fixed prosthodontics. In a 1985 survey of North American dentists, Donovan and colleagues showed that 95.55% of them use displacement cords routinely in their practice. A more recent survey of 1246 prosthodontists regarding their current methods used to expose their margin preparation revealed that 98% of respondents use displacement cords and 48% use a 2-cord technique for more than half of their impressions.
Different types of cords have been advocated for tissue displacement (unwaxed floss, 2/0 untreated surgical silk, twisted cords, synthetic material). However, 2 types have become the primary ones used clinically: braided and knitted cords ( Fig. 7 ). There is a lack of standardization in cord size and clinical efficacy, making the choice of displacement cord based on the personal preference of the clinician. The cords can be dispensed from a container (which could lead to cross-contamination), a clicker, or precut and individually wrapped (which eliminates guessing the length of the cord needed for each tooth) ( Fig. 8 ).
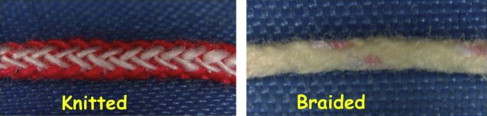

Braided cords have been described as having a consistent and tight weave. The braiding makes them resistant to separation during placement and therefore they are considered to be easy to manipulate and pack into place. Regardless of the configuration, these cords absorb the medicaments efficiently and do not split or tear during placement. A clinical study aimed at comparing the performance of 3 types of displacement cords found that the braided cords were ranked better than the twisted ones. Both serrated or smooth packing instruments can be used with braided cords without any concern to the clinician. Several packing instruments are available to purchase from manufacturers and vary in design and angulation. The choice of the instrument depends on the clinician’s preference.
Knitted cords have substantially increased in popularity in recent years due to their ease of placement and their ability to expand when wet, making them easy to insert in the sulcus. They are also available in different diameters and colors and similarly to the braided cords they lack standardization among manufacturers. Their design requires the use of thin, smooth, and nonserrated instruments. Serrated instruments can lift loosely woven cords out of the sulcus. It is suggested to start the cord placement in the interproximal area where tissue is more easily displaced. The authors think that a periodontal probe can be effectively used when the gingiva is thin and delicate and there is minimal sulcus depth ( Fig. 9 ).

Hemostatic Medicaments
Questionnaires (1246 of 2436) reviewing the current methods used by prosthodontists to expose the finish line showed that 81% of prosthodontists soak their cords in a hemostatic agent before placing them into the sulcus. Fifty-five percent used aluminum chloride (AC), 23% used FS or ferric subsulfate, and 70% used an additional agent after the cord is placed. For that purpose, FS in an infuser syringe was most commonly used. Several medicaments (aluminum potassium sulfate [Alum], aluminum sulfate, AC) have been shown to provide sufficient tissue displacement without any iatrogenic effect on the soft tissue.
Several hemostatic medicaments are available to be used in conjunction with displacement cords and many have been substantially studied.
Epinephrine
In the 1980s it was determined that 55% to 79% of dentists used displacement cords impregnated with epinephrine. A recent survey indicated that the percentage of dentists using epinephrine for tissue displacement decreased when compared with previous years. Epinephrine is known to cause adverse cardiovascular problems (hypertension, increased heart rate) and/or other symptoms such as anxiety, increased respiratory rate, tachycardia, and, in rare instances, death.
Human and animal studies evaluating the effect of epinephrine absorbed from displacement cords packed in the gingival sulcus expressed some concerns about the adverse health effects of this medicament. There is approximately 50 times more epinephrine in 1 inch of displacement cord than in 1 carpule of 1:100.000 epinephrine. Under certain conditions, epinephrine is absorbed systematically when used in conjunction with a displacement cord. Reducing the concentration and the contact time of epinephrine with the gingiva seemed to reduce the adverse effects. Of 495 surveyed dentists, 396 used displacement cords with epinephrine. Twenty percent of these dentists had patients with significant systemic side effects. A 3% increase in their patient’s pulse and 9% increase in blood pressure were recorded. They concluded that dentists have equally effective agents available on the market for them to use with no systemic side effects. A histologic study on the effect of several displacement materials on the gingival sulcus epithelium showed that an extended contact of epinephrine with the crevicular epithelium could cause necrosis. The use of epinephrine can expose the underlying connective tissue and setup a wound-healing response that could result in a less that ideal gingival response for some patients.
Other studies showed that a low concentration of epinephrine could safely be used in displacement cords without concerns for side effects. However, there is a general consensus that epinephrine should be avoided for tissue displacement given the significant number of complications that can occur specifically in patients with cardiovascular problems in addition to a pronounced vasoconstrictor effect.
Several studies compared the effectiveness of epinephrine to other medicaments available for tissue displacement. In a blind study, Jokstad found that neither the students nor the faculty members that participated in the experiment could tell the difference between gingival displacement obtained by epinephrine or aluminum sulfate. He concluded that no clinical benefit could be recognized between an epinephrine- or an AC-containing cord. Similarly to the previous study, Weir and Williams found that epinephrine did not produce superior displacement to AC. In another study, no practical difference was found between potassium aluminum sulfate, epinephrine, and AC. In addition, Pelzner and colleagues found that epinephrine-impregnated cords produce an unsatisfactory amount of tissue displacement and lead to 60% of impression remake.
Astringents
Astringents are metal salts that cause contraction of the gingival tissue by contracting small blood vessels. They precipitate tissue and blood proteins that physically inhibit bleeding by decreasing exudation and making the surface of the gingival tissue tougher. These hemostatic agents do not penetrate the cells; they only affect the superficial layer of the mucosa. However, an extended duration of contact with the gingival tissues can cause delayed healing or tissue damage. The pH of the hemostatic agents differs from one company to the other. Some studies demonstrated that they are highly acidic and their use removes the smear layer, a potential cause of postoperative sensitivity and an adverse effect on the bonding mechanism of adhesive cements.
Hemostatic agents are available in liquids or gels and the most commonly used are aluminum sulfate, AC, Alum, FS, and nasal and ophthalmic decongestants. Recently, manufacturers introduced hemostatic agents in the form of pastes or foam (Expasyl, Gingitrac, Magic foam cord, Racegel, Traxodent).
Liquids/Gels
One of the popular hemostatic agents is AC with a concentration ranging from 20% to 25% ( Fig. 10 ). Studies showed that a 5% to 10% AC solution along with a displacement cord is safe and effective. However, if used with in concentrations higher that 10%, AC can be irritating and may cause damage to the gingival tissue. Buffered AC was introduced to prevent irritation of the gingival tissue. Reiman found that AC is least irritating with no permanent damage to gingival tissue when the solution is left in the sulcus for up to but not exceeding 15 minutes. Several authors recommend soaking the displacement cords in AC to enhance hemostasis and avoid laceration of the gingival tissue. Runyan and colleagues studied the effect of soaking displacement cords in AC on moisture absorption. They concluded that doing so has no effect on the cord’s ability to absorb fluid.