Fig. 10.1
Maxillary defect after amputation in an edentulous patient. In this situation, an obturator is not favorable to function as a removable partial denture without optimal support
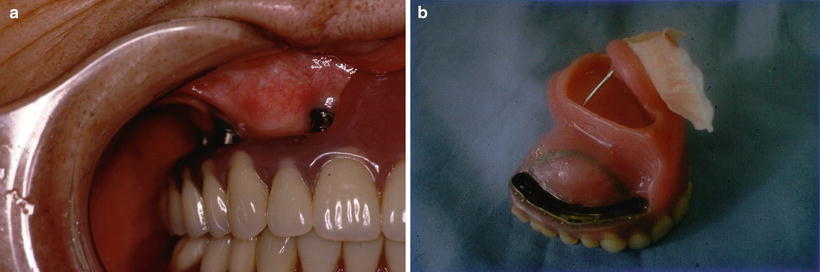
Fig. 10.2
a A maxillary implant-borne obturator supported by a milled bar attachment. b The facial prosthesis was retained by a magnetic attachment to the maxillary obturator prosthesis [9]
First Step: Basal Bone Reconstruction
Basal bone reconstruction should be considered either at the same time of mandibular amputation or after ablative surgery as a secondary reconstructive surgery. Depending on the reconstruction choice or prosthetic choice, alveolar bone reconstruction should be also considered.
Second Step: Evaluation of Oral Functions and Preparation for Prosthetic Rehabilitation
In evaluation of oral functions such as swallowing ability, tongue movement, and mouth opening, mouth opening is a most important factor to fabricate the prosthesis. Dental and oral hygiene are also important factors.
Third Step: Prosthetic Rehabilitation
After basal bone reconstruction, prosthetic rehabilitation is considered, that is, whether to use dental implants. If necessary, local soft tissue management should be performed before or after implant placement. Alveolar bone reconstruction is frequently necessary for prosthetic rehabilitation before implant placement.
10.4 Mandibular Reconstruction for Implant Placement
10.4.1 Nonvascularized Bone Graft
Harvest of free nonvascularized bone graft from the iliac crest is a well-established procedure for reconstruction of the mandible [7]. A block bone or cortico-cancellous bone harvested from the anterior or posterior iliac crest is used. Because of the nonvascular nature of these grafts, this procedure is generally performed as a secondary operation at least a year after the initial cancer ablation to avoid the high incidence of graft loss and infection when performed primarily. Indication of the nonvascularized bone graft is for the relatively short defects of the lateral mandible that do not cross the midline. This technique is especially effective following benign tumors such as ameloblastoma [7] (Fig. 10.3).
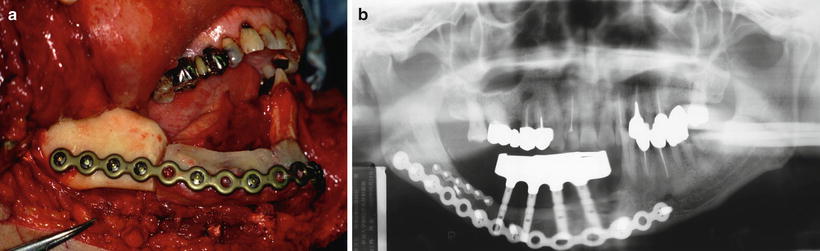
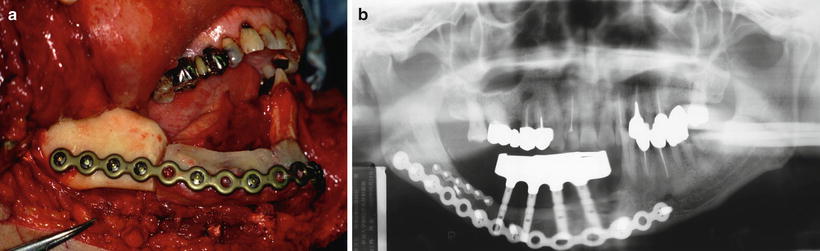
Fig. 10.3
a Use of nonvascularized free bone graft from the iliac crest for mandibular reconstruction following an ameloblastoma. b An implant-supported bridge was fabricated (at 5-year-follow-up)
10.4.2 PCBM-MESH
Another procedure similar to free bone grafting is particulate cancellous bone marrow (PCBM) combined with titanium mesh (PCBM-MESH), which was first described by Boyne [10]. Several studies report successful results with this procedure [11–13]. PCBM was taken from the anterior and posterior iliac crest, respectively, as described by the authors in a previous publication [14]. With delayed reconstruction, the remaining mandible was exposed using an extra-oral approach to avoid entering the oral cavity. Dumbach and dynamic mesh plates [Dumbach Titanium Mesh-System, Titanium Dynamic Mesh, Micro-Titanium Augmentation Mesh (M-TAM); Stryker-Leibinger, Freiburg, Germany] were then adapted to the remaining bone by cutting and bending them into the desired shape. The mesh was fixated to each side of the host bone using titanium screws. The surrounding soft tissues including muscle, fatty, and fibrous tissue was then tightly sutured to the lateral, medial, and inferior surfaces of the tray to eliminate any dead space. The PCBM was loaded into the mesh and condensed to increase graft density. After adequate subcutaneous relaxation incisions were made, the overlying skin was sutured with minimal tension. The selection of the titanium mesh depends on the length and shape of the defect. Relatively large segmental defects need Dumbach; dynamic mesh was used for small defects and large alveolar defects; and titanium micromesh was applied to alveolar defects. Prosthetic rehabilitation started 6 months after implant insertion. PCBM-MESH has advantages for the reconstruction of facial contours in relatively difficult areas (e.g., the anterior part of the mandible) and the preparation of the bony bed for the application of dental implants (Figs. 10.4, 10.5). The risk factors for infection are reconstruction length, radiation therapy, and the existence of vascularity in the peripheral soft tissue [15].

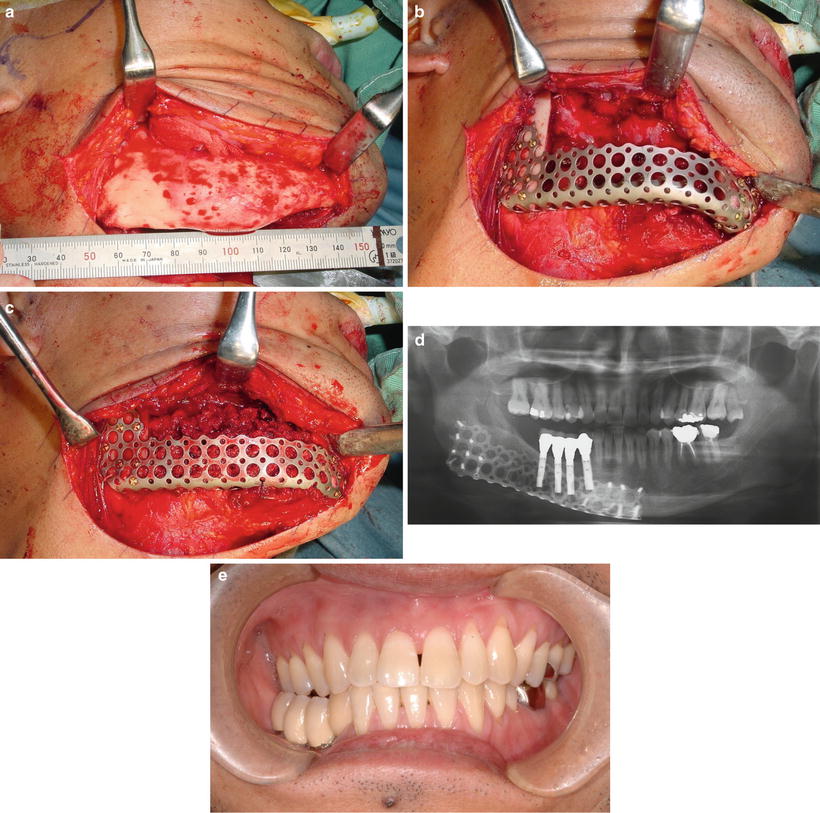

Fig. 10.4
a PCBM-MESH procedure. A Dumbach titanium mesh tray was adapted to the remaining bone. Then, particulate cancellous bone marrow (PCBM) was packed into the mesh tray. b PCBM was harvested from the bilateral posterior ilia. c Six months after bone graft. A very satisfactory amount of bone has formed in an ideal curve of the anatomical mandibular arch
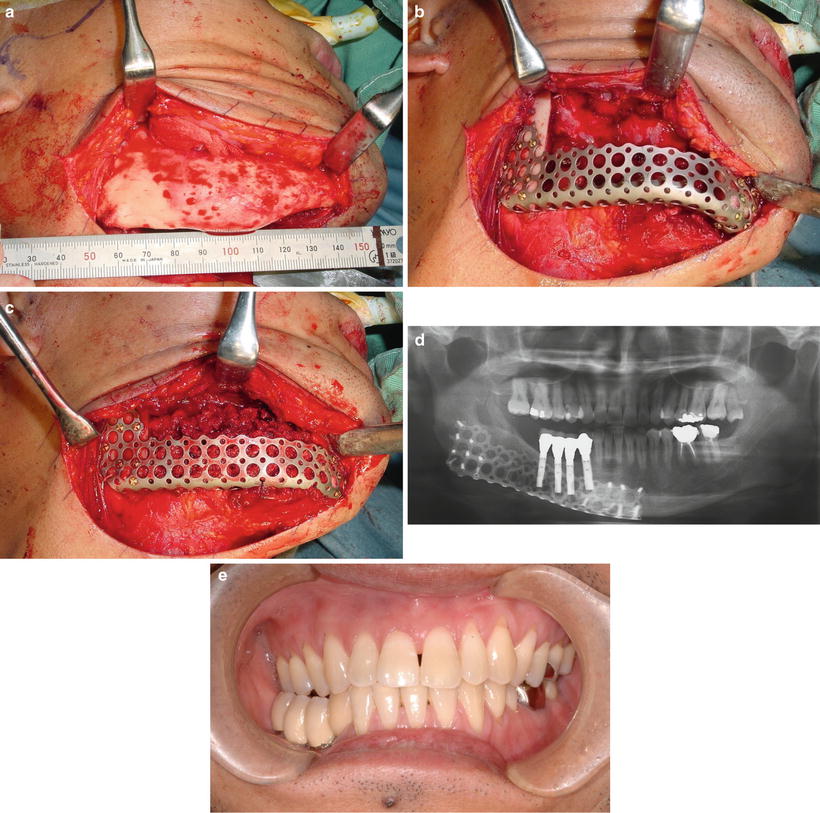
Fig. 10.5
a A case of mandibular reconstruction followed by the implant placement using PCBM-MESH method. A patient with a benign tumor (ossifying fibroma) underwent segmental resection. b A Dumbach titanium mesh tray was adapted to the remaining bone. c PCBM was packed into the mesh tray. d Implants were placed 6 months after PCBM grafting without removal of the mesh tray. e An implant-supported bridge was fabricated
10.4.3 Distraction Osteogenesis
Distraction osteogenesis (DO) is a unique technique that has been applied to the maxillofacial region. The main advantages of DO include circumventing donor site intervention for bone grafts, reducing morbidity, and elongating the soft tissues [16]. However, there are some disadvantages. First, DO is a very time-consuming technique and is burdensome for the patient to activate daily or twice daily by hand. Second, because the mandible is a three-dimensional curved structure, a curved DO is necessary [17], which is almost impossible to apply in the anterior region. Therefore, DO could only be used in the posterior mandible. Third, when the bone transport technique is applied, a bone graft may be required to obtain continuity of the mandible at the end stage of the distraction [18] (Fig. 10.6).
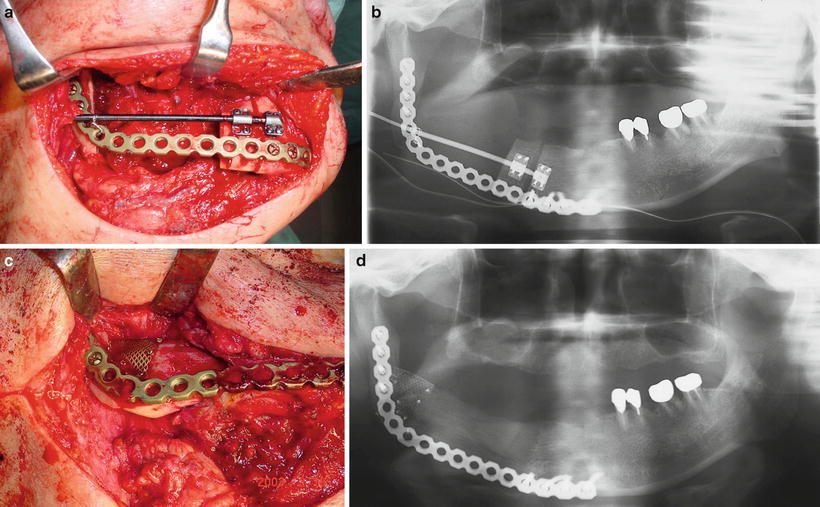
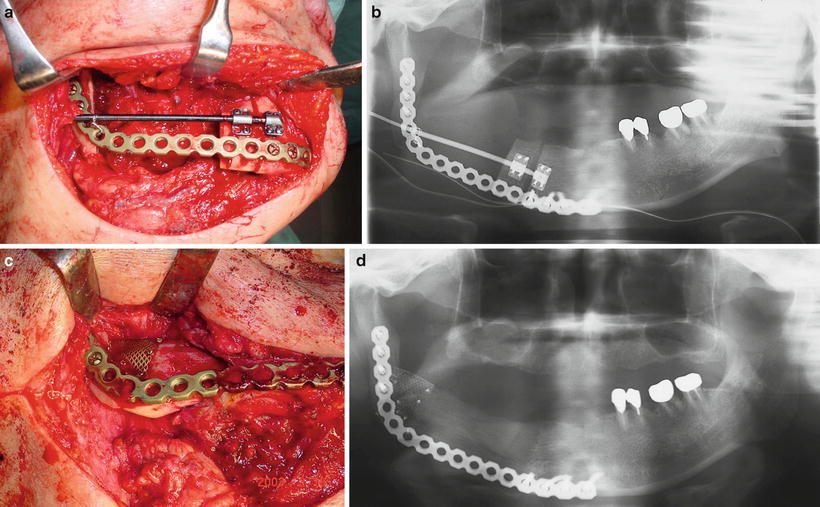
Fig. 10.6
a A case of mandibular reconstruction using distraction osteogenesis (DO). After amputation of the mandible, a reconstruction plate was placed. Simultaneously, a bone transport segment was fabricated and a distraction device was installed. b Panoramic X-ray after installation of the distraction device. c After the DO procedure, a small bone graft using a titanium mesh and autogenous cancellous bone was performed at the docking site of the transport segment and the remaining mandibular ramus. d A panoramic X-ray approximately 1 year after DO showed very good bone formation at the distracted area
10.4.4 Free Vascularized Bone Graft
Microvascular tissue transfer has revolutionized cancer reconstruction [19–22]. One of the advantages of this technique is that soft tissue can be transferred from a distant site in the same operative encounter as the ablative surgery and, in most instances, from a single donor site. There are three main donor sites for vascularized bone used in mandibular reconstruction: fibula, iliac, and scapula. Each donor site has its own advantages and disadvantages, and an ideal replacement for maxillary or mandibular bone and intraoral soft tissue does not yet exist [23] . The fibula can also be harvested as a bone-only, an osteoseptocutaneous, or a myo-osteocutaneous flap (soleus or flexor hallucis longus). The fibula flap is popular and has been the first choice for jaw reconstruction for many reconstructive surgeons because of the ease of the harvest, ability to work in two teams, availability of a long bone segment, and good pedicle length. One of the disadvantages is insufficient vertical height of the fibula. On average, the fibula’s height is between 13 and 15 mm, which is similar to that of the edentulous mandible and is insufficient for that of the dentate mandible [7]; this accounts for the unfavorable implant axis and the space between the connection of the prosthesis and abutments. Various techniques to increase the height of the fibula have been proposed, including “double-barrelling”[24] and vertical distraction osteogenesis [25]. A relatively simple technique is to simply adapt the fibula to abut the native mandible in a slightly more superior position than the inferior border. The iliac crest is the only bone that provided sufficient bone volume [7]. This volume is crucial to both implant placement and stability of the tissue-borne prosthesis. The iliac crest offered advantages in height, width, and overall strength when harvested together with the internal oblique muscle and the cutaneous paddle, based on the deep circumflex iliac artery (DCIA) and the accompanying deep circumflex iliac vein (DCIV). Although the volume of the bone is good, the length of the available bone is somewhat limited, and the volume of soft tissue that must be included with this flap can be bulky [7]. The free scapula flap can provide a large amount of soft tissue connected with the bone. However, as was the case with fibula, the bone available is not the best choice for implant length. The available bone length is a maximum of 12 cm, but may be enhanced by harvesting the whole scapular tip and using it transversally for anterior reconstruction [26]. The scapula is also available for maxillary reconstruction. For implant placement, another augmentation procedure is necessary (Fig. 10.7).
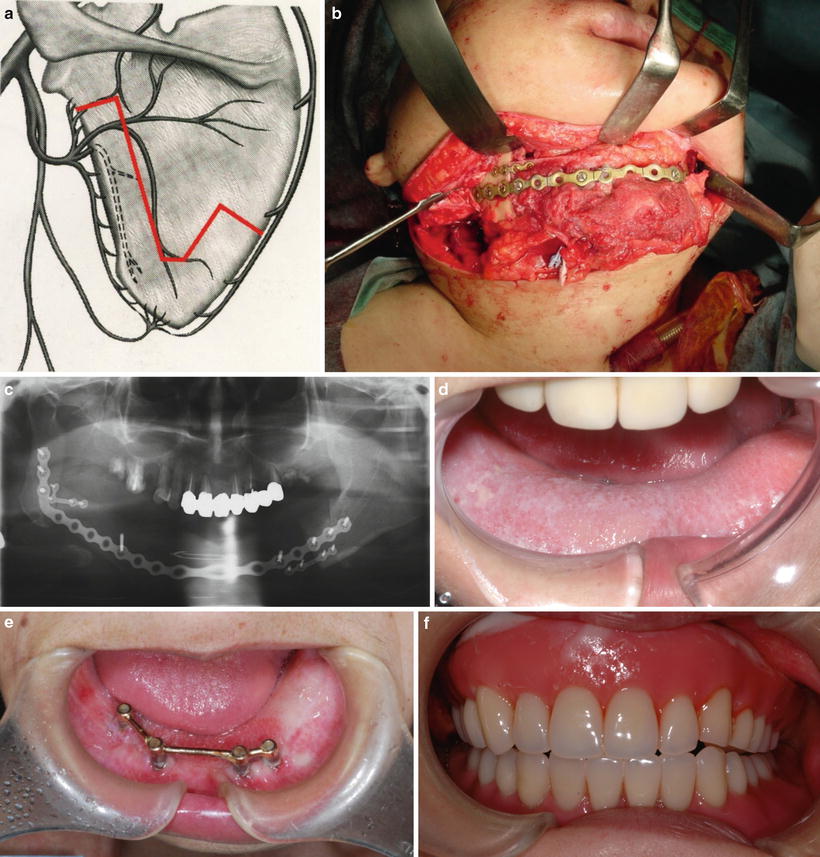
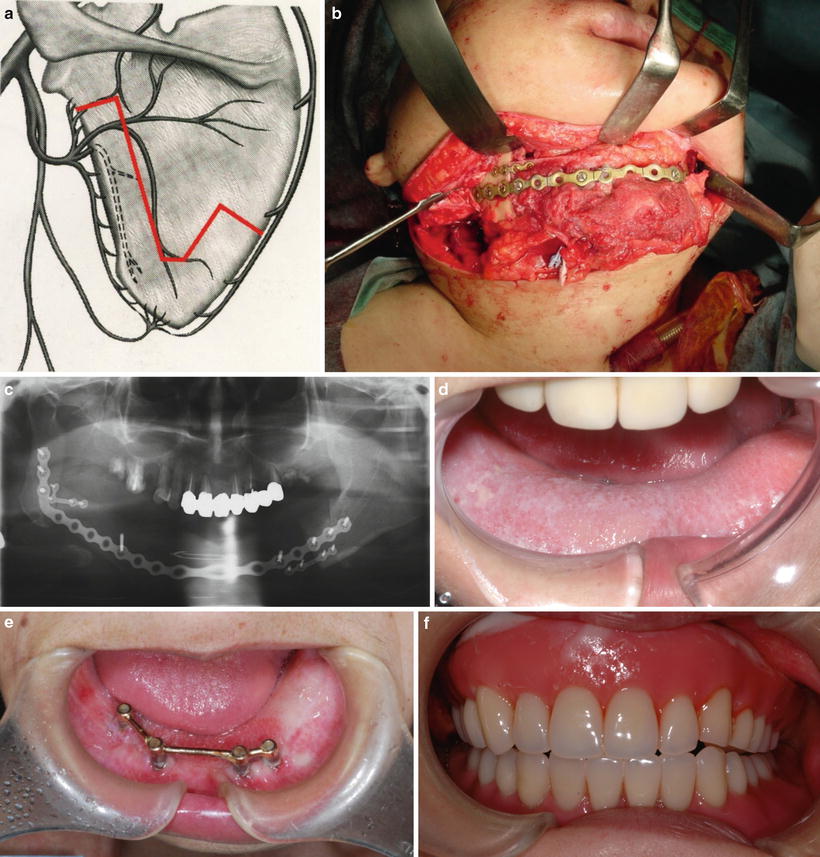
Fig. 10.7
a A vascularized scapula flap. When the bone flap is prepared as bipedicled, the bone may be cut into two or three pieces and fixed at the desired angle to simulate the contour of the mandible. b Use of a bipedicled scapula flap for the mandibular reconstruction. c Approximately two thirds of the mandible was reconstructed using a bipedicled scapula flap. d A subcutaneous flap is seen in the oral cavity. e Before the fabrication of a final prosthesis after implant placement, thinning of the skin paddle (“defatting”) was performed, and a bar attachment was fabricated. f An implant-stabilized denture was fabricated
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


