Over the course of the past 30 years, oral implantology has constantly evolved to become one of the main focuses of modern dentistry. Today, this treatment modality has been incorporated into the curriculum of most dental schools, which has dramatically improved the availability of professionals trained to treat patients with dental implants. Significant improvements in the success rate and longevity of dental implants have increased awareness and the interest of the public and professional community alike. For most clinical scenarios, implant-retained and implant-supported restorations provide the best alternative for the rehabilitation of partially or completely edentulous patients. When patient satisfaction and oral health–related quality of life are compared in patients treated with dental implants and those treated with conventional prosthetic techniques, satisfaction is always significantly greater in the former group. Additional benefits associated with dental implant therapy include no risk for caries, improved esthetics, maintenance of bone at the edentulous site, and decreased abutment loss ( Fig. 12-1 ).


Etiopathogenesis/Causative Factors
There are several major causes of tooth loss; among them are dental caries, periodontal disease, and trauma. The aging process has always been intuitively considered to be an important variable in tooth longevity. However, it was not until the National Institute of Dental and Craniofacial Research ran a study of surveillance of dental health in the United Sates between 1999 and 2002 that this particular point was confirmed. In this study it was found that the mean number of remaining teeth is indeed inversely correlated to the patient’s age. Conversely, young age does not necessarily correlate with maintenance of complete dentition. In this same study it was found that the population of young adults between 20 and 39 years of age averages only 27 teeth. If one makes the assumption that all individuals have their third molars removed before the age of 20 (and this is of course a big assumption), this shows that this age group is missing at least one permanent tooth. In the subset of individuals ranging between 40 and 59 years of age, the average number of remaining permanent teeth is 24. Again, not counting the third molars, this is a 15% decline in the number of remaining natural dental units. Finally, in the patient subset 60 years and older, the average number of remaining permanent teeth is just 19. This is a 32% attrition rate of the natural dentition. The same study revealed a similar trend on complete edentulism. In other words, the older the individual, the greater the chance of having natural teeth missing. To this effect, the prevalence was shown to be less than 1% for the young adult group and 25% for the group 60 years or older. If in addition one considers the current life expectancy in the United States, which is 77.9 years, it becomes immediately evident that many senior adults spend almost 25% of their life with significantly crippled dentition. Interestingly, non-Hispanic black adults have the highest prevalence of edentulism, followed by the non-Hispanic white population, with the Mexican American group having the lowest prevalence.
Education has proved to play a major role in dental health and the resulting number of remaining natural teeth. The population subgroup of individuals without a high school education has an increased prevalence of complete edentulism of 9%, followed by 4% for the group with a high school education and 3.5% for those with an education beyond the high school level. Another important factor to take into account is income level. The population that is more than 200% below the federal poverty level (FPL) has higher additional prevalence (15%) than does the group less than 100% of FPL (5%). Finally, smoking has been associated with poor dental health, with smokers having a higher prevalence of edentulism (14%) than non-smokers (4.5%).
Multiple problems have been associated with edentulism. Even though edentulous patients pursue restorative procedures with complete or partial dentures, this is rarely adequate to compensate for the missing natural structures. The bite force pressure that these individuals are able to generate is approximately 25% less than normal. As a consequence, their food selection is very limited, with significantly less intake of vegetables, carotenes, and fiber and a greater tendency to consume foods high in cholesterol and saturated fat. The combination of poor oral intake, compromised dental function, and malnutrition can lead to debilitation, illness, and potentially decreased life span. In a recent article, David Felton showed that completely edentulous patients have a higher risk for the development of multiple systemic disorders. Edentulism was found to be a global issue, with estimates of an increasing demand for complete denture prostheses in the future. Completely edentulous patients were found to be at higher risk for poor nutrition, for coronary artery plaque formation (odds ratio, 2.32), to be smokers (odds ratio, 2.42), to be asthmatic and edentulous in the maxillary arch (odds ratio, 10.52), to be diabetic (odds ratio, 1.82), to having rheumatoid arthritis (odds ratio, 2.27), and to have certain cancers (odds ratios varying from 1.54 to 2.85, depending on the type of cancer). In addition, chronic residual ridge resorption continues to be the primary intraoral complication of edentulism, and there appear to be few opportunities to reduce bone loss in these patients.
Pathologic Anatomy
According to Wolff’s law, bone remodels in direct relation to the forces applied to it. Approximately 4% of strain is required to obtain a balance between osseous formation and the resorption process. Following dental extraction, alveolar bone starts to undergo an immediate process of resorption and remodeling. Alveolar bone remodels significantly during the first few months after losing teeth, with a quick reduction of almost 25% of alveolar width and a decrease in alveolar height of 4 mm on average. A marked decrease in blood supply and increased interalveolar distance make the remodeling process appear to be more significant, approximately four-fold for the maxillary ridge in comparison to the mandible. A more recent study suggests that the alveolus may suffer 40% reduction in height and 60% in width within the first 6 months after extraction ( Fig. 12-2 ).
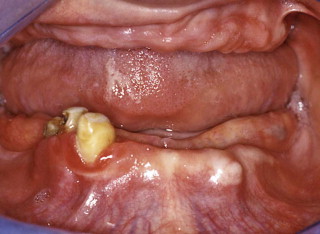
As the intraoral hard structures change, a direct and proportional alteration can be observed in the overlying soft tissues. The soft structures are affected by a progressive decrease in keratinized tissue and attached gingiva. Secondary to the bone loss and apical migration of the crest of the residual alveolar ridges, muscle insertions become more prominent. In an edentulous patient, the lack of counterpressure provided by the dentition allows the tongue to expand over the residual alveolar ridge and results in tongue hypertrophy as well.
The lack of teeth and bone resorption in edentulous patients cause multiple changes in facial architecture, which ultimately compromises the overall facial esthetics of patients and gives them the classic “old toothless face look.” This results mainly from a decrease in facial height as a result of reduced vertical dimension and improper support of the lips and cheeks. Bone resorption and the absence of mandibular teeth decrease the labiomental angle, followed by collapse of the muscular attachment and a counterclockwise rotation of the chin, which gives the patient a pseudo-prognathic appearance. At the same time, a reduction in function of the mandible causes atrophy of the orbicularis oris and buccinator muscles, with the modiolus being displaced posteriorly and medially. Consequently, the patient acquires an aged appearance with hollow cheeks and thin lips. The absence of support of the upper lip increases the columellar-philtrum angle, which increases lip length and gives the impression of a large nose. Finally, a lower attachment of the buccinators and mentalis muscles to the body and symphysis causes tissue sagging and, subsequently, jowls and a “witch’s chin” appearance, respectively.
Pathologic Anatomy
According to Wolff’s law, bone remodels in direct relation to the forces applied to it. Approximately 4% of strain is required to obtain a balance between osseous formation and the resorption process. Following dental extraction, alveolar bone starts to undergo an immediate process of resorption and remodeling. Alveolar bone remodels significantly during the first few months after losing teeth, with a quick reduction of almost 25% of alveolar width and a decrease in alveolar height of 4 mm on average. A marked decrease in blood supply and increased interalveolar distance make the remodeling process appear to be more significant, approximately four-fold for the maxillary ridge in comparison to the mandible. A more recent study suggests that the alveolus may suffer 40% reduction in height and 60% in width within the first 6 months after extraction ( Fig. 12-2 ).

As the intraoral hard structures change, a direct and proportional alteration can be observed in the overlying soft tissues. The soft structures are affected by a progressive decrease in keratinized tissue and attached gingiva. Secondary to the bone loss and apical migration of the crest of the residual alveolar ridges, muscle insertions become more prominent. In an edentulous patient, the lack of counterpressure provided by the dentition allows the tongue to expand over the residual alveolar ridge and results in tongue hypertrophy as well.
The lack of teeth and bone resorption in edentulous patients cause multiple changes in facial architecture, which ultimately compromises the overall facial esthetics of patients and gives them the classic “old toothless face look.” This results mainly from a decrease in facial height as a result of reduced vertical dimension and improper support of the lips and cheeks. Bone resorption and the absence of mandibular teeth decrease the labiomental angle, followed by collapse of the muscular attachment and a counterclockwise rotation of the chin, which gives the patient a pseudo-prognathic appearance. At the same time, a reduction in function of the mandible causes atrophy of the orbicularis oris and buccinator muscles, with the modiolus being displaced posteriorly and medially. Consequently, the patient acquires an aged appearance with hollow cheeks and thin lips. The absence of support of the upper lip increases the columellar-philtrum angle, which increases lip length and gives the impression of a large nose. Finally, a lower attachment of the buccinators and mentalis muscles to the body and symphysis causes tissue sagging and, subsequently, jowls and a “witch’s chin” appearance, respectively.
Diagnostic Studies
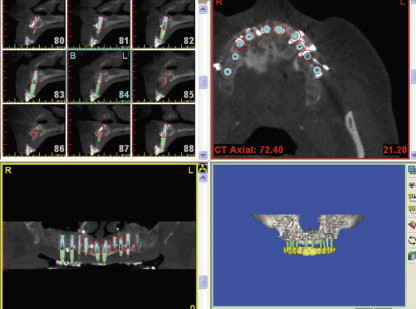
Traditionally, obtaining dental models of the patient’s mouth has been of great value in determining the residual anatomy of the patient. As expected, the information obtained is limited to the structures observed during clinical examination, which may or may not accurately represent what is happening under the surface. Therefore, radiographic imaging can provide the surgeon with valuable information about bone morphology and the position of relevant anatomic structures. Different modalities of radiographic imaging are used for implant dentistry, all of them with specific advantages over the other modalities. The traditional periapical radiograph provides detailed image quality for evaluating bone height and monitoring bone healing around the implant with minimal radiation exposure and operative time, but with very limited information on the surrounding structures. This is usually a good imaging option for individual units in the anterior maxillary and mandibular arches. In situations involving completely edentulous patients, the cephalometric radiograph helps the surgeon determine the anteroposterior implant angulations in the anterior region, as well as the intermaxillary relationships. However, the panoramic radiograph is probably the most common radiographic modality used for surgical dental implant planning because of the overall view of the maxilla and mandible that it provides; however, the image suffers from magnification and positional artifacts ( Fig. 12-3 ).

In 1973 computed tomography (CT) was developed, and advances in this technology led to the introduction of cone beam CT in 1999. This technology produces excellent three-dimensional images of the maxillofacial structures with a fraction of the radiation dose of conventional CT ( Fig. 12-4 ). When CT is used, bone quality can be determined with Hounsfield units, which correspond to the degree of attenuation of a biologic object subjected to a dose of radiation. The Hounsfield unit is also known as the CT number; the value of water corresponds to 0, air to −1000 units, and bone to values approximately higher than 400 units, depending on its density. Another way to measure radiation is by using sieverts (Sv), a unit reflecting the effect of radiation on tissue and named after the Swedish medical physicist Rolf Sievert. It has been established that a full-body equivalent dose of 1 Sv causes nausea and that 2 to 5 Sv causes epilation or hair loss, hemorrhage, and death in many cases. Higher than 3 Sv will lead to a dose that is lethal to 50% of individuals within 30 days (LD 50/30 ), and with higher than 6 Sv, survival is unlikely. Table 12-1 summarizes the radiation dose values of different imaging techniques. Notice that the doses are listed in microsieverts (µSv).
| RADIATION SOURCE | RADIATION DOSE |
|---|---|
| Daily background radiation | 8 µSv |
| 10-second cone beam CT study | 34 µSv |
| 20-second cone beam CT study | 68 µSv |
| Panoramic radiograph (average) | 10-15 µSv |
| Digital panoramic radiograph | 4.7-14.9 µSv |
| Highest film panoramic radiograph | 26 µSv |
| Full mouth series | 150 µSv |
| Medical CT study | 1200-3300 µSv |
The implant surgeon may use any of the imaging modalities just described but must strictly follow the radiation safety principle of “as low as reasonably achievable” (ALARA) to provide the patient with the best possible care.
Reconstructive Goals
The goal of implant dentistry is to restore normal dental anatomy and function while maintaining residual alveolar bone height and width. In other words, implant-supported restorations should reestablish an adequate esthetic appearance and restore the chewing capacity of the patient. At the same time, once the implant is placed under function, occlusal forces should maintain a balance to favor the alveolar bone remodeling process.
Specific Treatments and Techniques
Preoperative Considerations—Pharmacology
The use of preoperative antibiotic prophylaxis during dental implant surgery is still controversial. A study comparing preoperative or postoperative antibiotics involving almost 3000 implants demonstrated a higher survival rate in the group receiving preoperative antibiotic prophylaxis. The same results were observed in a similar study involving a similar number of implants. However, other studies have found no statistically significant benefits with the use of prophylactic antibiotics during routine implant placement.
Definitions
Dental implants are restored at different times following initial placement. The literature has multiple names describing the variety of situations involved in dental implant treatment. For this reason, Cochrane and colleagues published a consensus statement of appropriate terms and definitions of these distinctive scenarios.
- •
Immediate loading: a restoration is placed in occlusion within 48 hours of implant placement.
- •
Immediate restoration: a restoration that is not in occlusion is inserted within 48 hours of implant placement.
- •
Conventional loading: the prosthetic component is inserted during a second procedure after a healing period of 3 to 6 months.
- •
Early loading: a restoration in occlusion is placed after 48 hours of implant placement, but no later than 3 months.
- •
Delayed loading: the prosthetic component is attached in a second procedure after 3 to 6 months of implant placement.
Basic Technique
Several important considerations must be kept in mind when surgically placing osseointegrated dental implants. As an inert alloplastic device, the fixture has no ability to fight infection, which is why it is of utmost importance to perform the surgical procedures in a way that minimizes the risk for infection, particularly during the critically important immediate postoperative period. A simple but effective way to help in this effort is to carefully prepare and place the surgical fields in accordance with standard aseptic guidelines. A sterile surgical technique must be followed with strong consideration of antibiotic prophylaxis. It has been the common practice of the authors to use the same antibiotic protocol recommended by the American Heart Association for patients at risk for subacute bacterial endocarditis: 2 g of amoxicillin 1 hour before the procedure or 600 mg of clindamycin for penicillin-allergic patients. In addition, a 0.12% chlorhexidine mouth rinse twice daily is started 2 days before the procedure and continued for 5 days after surgery.
Manipulation of soft tissues must be as gentle as possible. This helps reduce the risk for tissue trauma, which translates into easier postoperative recovery. At all times during preparation of the osteotomies, copious irrigation must be used. The implant sites require the use of sharp drills with a progressive increase in size. An intermittent and precise preparation with controlled speed and torque will also assist in minimizing trauma to the bone. These concepts are not new to the field of oral implantology and have been in place since the very early developments of this discipline. All of these concepts have a direct impact on the ability of the clinician to control the temperature at the surgical site. It is of critical importance to maintain the temperature below 47° C and to keep drilling time to less than 1 minute at a time.
Finally, avoiding contact of the implant surface aids in the prevention of bacterial seeding. For this reason it is recommended that the implant be retrieved from the sterile vial and carried directly to the osteotomy site without touching the gloves, suction tip, saliva, or other tissues. Once the fixture is inserted to the correct depth, careful repositioning and manipulation of the soft tissues are performed. If sutures are to be used, fine monofilament materials are recommended to avoid entrapment by bacterial plaque as much as possible ( Fig. 12-5 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


