With the exception of those special cases of clefts associated with holoprosencephaly, wherein there exists true tissue hypoplasia, the anomalies observed in labiomaxillary clefts result essentially from displacement, deformation, and functional hypotrophy of the dentoskeletal elements and the covering soft tissues. This is particularly true with the maxillary bony segments, the dentoalveolar elements that they support, and the nasal cartilages. It is also true for the nasolabial muscles, which are all present on the cleft side but whose absence of normal insertions and the resultant dysfunctions are directly responsible for supra- and subjacent anomalies. Displacement, deformation, and functional hypotrophy also affect the mucocutaneous structures that border the labial clefts. This fact is less well known, but it has, nevertheless, great importance in the selection of incision design in the primary closure of cleft lip. The goal of primary closure is not only to re-establish normal insertions of all the nasolabial muscles but to restore the normal position of all the other soft tissues, including the mucocutaneous elements.
Surgical correction of cleft lip remains an elusive problem, principally because the fundamental surgical problem is not clearly conceptualized. This failure to define the problem accurately is attributable to the fact that the relevant anatomy is complex, poorly understood, and frequently erroneously described. Meaningful correction of cleft lip can be achieved only when the surgeon is fully appreciative of normal and pathologic spatial relations and functions of the anatomic elements, particularly the muscular elements, which cause the deformity. The treatment goal therefore is to obtain anatomic-functional balance between the soft tissues and the skeleton.
Congenital labiomaxillary clefts result from the absence of fusion or incomplete fusion of the maxillary and medial nasal processes. The superficial muscles of the face, which arise from the second branchial arch, migrate laterally and medially between the epidermis and subjacent ectomesenchyme and normally reach the midline in the week that follows fusion of the facial processes. In a complete labiomaxillary cleft, the muscles of the nasal floor and the upper lip cannot bridge the gap of the cleft and they cannot unite with their muscular counterparts on the noncleft side. The muscular integrity of the region is considerably disrupted, which has a profound effect on the underlying skeleton.
The transverse nasal muscle is the most important physiologic element in the nasolabial ring. It passes from the anterior border of the nasal bone to the incisive crest and then to the nasal septal perichondrium. Not only is this muscle responsible for nostril constriction, but, together with the external fibers of the orbicularis oris muscle, it provides support for its corresponding half of the upper lip and, indirectly, the labial commissure. The internal fibers of the oblique portion of the orbicularis oris normally extend into the columella and are connected to the anterior border of the nasal septum, its perichondrium, and the skin covering the columella. The nasal septum remains in the midline because symmetric muscles are inserted on both sides of it. The superior median interincisive suture is situated along the length of the septum and is united to it by the septopremaxillary ligament and the midline septum of the upper lip.
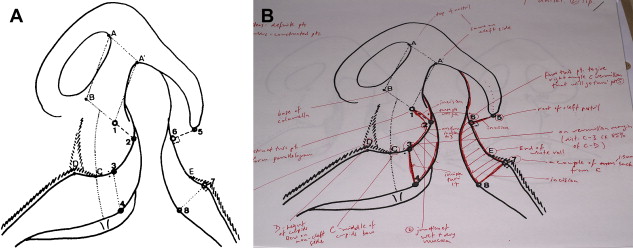
When there is a total unilateral labiomaxillary cleft, the muscles on the cleft side remain lateral to the defect; even if they are correctly formed, they cannot function normally ( Fig. 1 ). Deprived of the nasal septum and the anterior nasal spine as a point of anchorage, the system collapses much as a circus tent would do if it lost its central pole. Growth of the minor segment of the maxillofacial complex seems to be reduced as a probable consequence of absence of stimulation from the nasolabial muscles. On the noncleft side, the nasolabial muscles that are inserted on the nasal septum pull it into the noncleft nostril. Furthermore, on the noncleft side, which is frequently but erroneously referred to as the normal side, the premaxilla is also underdeveloped by an amount equal to the degree to which the median interincisive suture is bent to this side.

The lower lateral cartilage on the cleft side is flattened by divergent muscular traction corresponding to the degree of its missing normal support. The cartilaginous deformations can be considerable; however, except in rare cases, such as holoprosencephaly, there is little or no hypoplasia of the cartilage. Indeed, there is frequently no cutaneous hypoplasia, and if the skin appears insufficient, it is because it has not been distended by function ( Fig. 2 ). The sagging nasal capsule induces a retrusion of the nasal bone on the cleft side, giving rise to an internal rotation of the anterior maxillary pillar, which results in lateral displacement of the medial canthus. The resultant telecanthus is often mistaken for true unilateral hypertelorism. Early complete reconstruction of the soft palate, combined with functional reconstitution of the nasolabial musculature of the lip and the septum, provides important prerequisites for future balanced facial growth. These clinical observations suggest that the nasal septum directly influences growth of the premaxilla and indirectly influences growth of the maxilla; in so doing, it plays an active role in facial growth.

Cleft lip, with or without cleft palate, occurs more frequently than cleft palate alone and is the most common significant orofacial anomaly. Clefts of the lip and anterior maxilla have been thought to result from a deficiency of mesenchyme in the facial region attributable to failure of neural crest cell migration or proliferation of facial mesenchyme. The author believes that orbicularis oris muscle deficiency may be related more to perinatal functional dysmorphogenesis than to congenital mesenchymal deficiency.
The quality of surgical treatment of congenital clefts of the lip depends to a much lesser degree on the technical skill of the surgeon than on the appropriateness of the operative technique that is used. Surgery should reconstruct form and function of the divided face, such that balanced growth of the facial skeleton can take place. The surgeon ought to have sound knowledge of the initial faults and their postoperative sequelae, on which can be based adaptation of technique according to the needs of each case.
Schematically, the superficial muscles of the face are arranged in three interdependent rings that function normally in a manner of mutual maintenance. In the case of total labiomaxillary clefts, the vascular, nervous, and muscular elements provided by the lateral cervical blastemas remain on the lateral side of the cleft. The transverse nasal muscle, levator labii superioris alaeque nasi, levator labii superioris, depressor septi (myrtiformis), and horizontal and oblique heads of the orbicularis oris muscle thus do not insert on their corresponding elements on the medial side of the cleft. Consequently, they are prolapsed laterally against the minor maxillary segment from which they cannot solicit stimulation and normal growth. Neither can they participate, as they normally do, in growth at the interincisive suture, and the developing incisor teeth are relatively anteriorly malpositioned as a result. The nasal septum is pulled by the muscles on the noncleft side, displacing it and the anterior nasal spine in this direction. These muscular anomalies have a global, facial, ripple effect that influences mandibular equilibrium. On the cleft side, the labial commissure is deviated lateroinferiorly, influencing the depressor anguli muscle, which, in turn, favors lateral deviation of the chin to the cleft side. This accentuates the nasal asymmetry, and all the anterior part of the face is thus distorted and malformed.
If untreated, this condition persists without remarkable aggravation throughout growth, which explains why patients who are not operated on until adulthood have facial growth but with deformities of the same type as those observed at birth. In effect, at birth, the malformation is already the result of disequilibrium and muscular dysfunction that does not change a great deal unless the patient is operated on. After primary cheiloplasty, the anatomic and functional equilibria are radically transformed. Unfortunately, the anatomic reconstruction is rarely excellent, particularly with classic techniques that attribute great importance to the plastic (esthetic) aspect but less importance to the functional aspect. When this reconstruction is imperfect, it results in dysfunctions that disadvantageously affect subsequent skeletal growth of the face. If, however, the primary nasolabial reconstruction is good, anatomy, function, skeletal growth, and total facial aesthetics can be excellent ( Fig. 3 ). The fundamental goal of the surgeon is thus to achieve anatomic muscular reconstruction, particularly with respect to anchorage of the complex nasolabial muscles of the cleft side to the nasal septum and muscles on the noncleft side. The technique that allows this objective to be met, termed the primary functional cheilorhinoplasty , has been well described, particularly with respect to muscle reconstruction.
Displacement, deformation, and functional hypotrophy also affect the mucocutaneous structures that border the labial clefts. This fact is less well known, but it has, nevertheless, great importance in the selection of incision design in the primary closure of cleft lip. The goal of primary closure is not only to re-establish normal insertions of all the nasolabial muscles but to restore normal position of all the other soft tissues, including the mucocutaneous elements. Thus, one can only realize Veau’s “embryological surgery” by re-establishing at surgery all the anatomic and functional conditions that normally ought to have been present at the end of the embryonic stage.
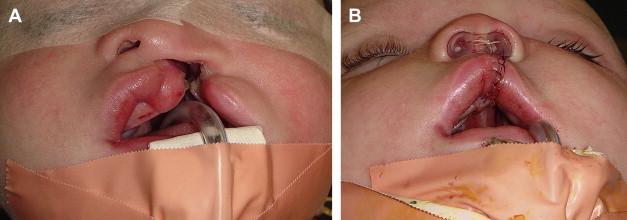
The characteristics of mucocutaneous abnormalities on both sides of the cleft include malposition of nostril skin onto the upper part of the lip, retraction of the labial skin, alteration of the white roll of the lip, and presence of a special mucosa neighboring the mucocutaneous junction on the sides of the cleft. There is malposition of nostril skin onto the upper part of the lip. As a consequence of the absence of normal muscular support of the floor and the sill of the nose, the skin of the lateral alar part and the medial columellar part of the nasal vestibule is lowered and intrudes onto the upper part of the lip. The limit between skin of nasal origin and that of the lip is usually well defined because the nostril skin is finely stippled, whereas that of the lip has more hair and is finely striated.
On the lateral side of the cleft, the skin of the lip is raised by the mass of the nasolabial head of the orbicularis muscle. In practice, the limit between nostril skin and the lip skin corresponds to a line drawn perpendicular to the mucocutaneous junction from the most external point of the border of the alar base. On the medial side of the cleft, the limit between the nostril skin and the lip skin is similarly well visualized by a line drawn oblique to the mucocutaneous junction from a point situated on the columellar border at a distance from the superointernal angle of the nostril equal to that of the noncleft side.
There is retraction of labial skin. On both sides of the cleft, the skin of the lip is less drawn out than normal by the underlying muscles. This results in a reduction in cutaneous length, which is classically thought to be attributable to primary hypoplasia. The skin, however, is actually a bit thicker as a result of the retraction.
There are alterations in the white roll. The limits of the white roll of the lip, relative to the simple “mucocutaneous junction” that it follows, are gradual. From the lateral side, the roll progressively diminishes to approximately 2 to 3 mm before it disappears. On the medial side below the inferior part of the philtrum, the limits are less clear.
There are abnormalities in the characteristics of the mucosa neighboring the mucocutaneous junction. Normally, the labial lining consists of three well-defined areas: an external cutaneous area; an internal area of wet mucosa; and an intermediate area called “the zone of Klein,” which is formed by a dry mucosa directly attached to the small compressor muscle of the lips. In labial clefts, particularly on the lateral side, the area that separates the skin from the wet mucosa is different from normal vermillion. Actually, the mucosa of this excessive area is finer than normal and is without an underlying glandular bed and the compressor muscle of the lips.
Thus, these clinical observations support the notion that disorganization of the system responsible for premaxillary growth is an important cause of dentoskeletal defects in patients who have a cleft deformity. Further, irrespective of the existence or not of a distinct human premaxilla, it retains sufficient independence to demand that the restoration of its anatomy and physiology, in addition to that of the entire medial septal system and nasolabial musculature, must be the cornerstone of successful primary and secondary cleft surgery. The author believes that this can best be achieved at approximately 6 months of age, when there has been sufficient development of muscle to permit careful identification and suturing of the relevant nasal and labial muscles to the nasal septum. Concomitant with primary lip surgery at 6 months of age, primary soft palate muscular construction must be performed to establish deep symmetric function and to aid in reduction of the width of the hard palate cleft, which provides the most favorable conditions with respect to the palatal mucoperiosteum during closure of the hard palate at approximately 12 months of age.
To re-establish the normal situation and dimensions of the mucocutaneous elements in primary closure of total, unilateral, labiomaxillary clefts, it is necessary to achieve good position of the skin of the floor and sill of the nostril, obtain good height of the skin of the cleft side, recreate good form and continuity of the white roll of the lip, establish equal vermilion height on both sides of the cleft and on both sides of the middle of the lip, and excise abnormal mucosa from both sides of the cleft ( Fig. 4 ).