Introduction
The purpose of this study was to analyze the maximum insertion torque (MIT) and maximum removal torque (MRT) values of orthodontic miniscrews.
Methods
Two hundred eighty titanium miniscrews were placed in several sites in the maxillae and mandibles of orthodontic patients to provide skeletal anchorage. Two types of miniscrews were used: predrilling, cylindrical miniscrews, and self-drilling, conical miniscrews. A force of 50 g was applied with nickel-titanium coil springs 2 weeks after placement. MIT and MRT values were assessed with a digital torque gauge. Torque values were subjected to the paired t test, Student t test, chi-square test, and 1-way analysis of variance (ANOVA) ( P <0.05).
Results
MIT values were significantly higher for the self-drilling miniscrews (mean, 14.5 Ncm; 95% CI, 13.6-15.3) than for the predrilling miniscrews (mean, 9.2 Ncm; 95% CI, 8.6-9.9) in all implant sites. For both predrilling and self-drilling miniscrews, the highest MIT values were observed at the midpalatal suture site followed by the dentoalveolar bones of the mandible and maxilla, respectively. In contrast, MRT values were significantly higher for the predrilling miniscrews (mean, 22.6 Ncm; 95% CI, 22.0-23.3) than for the self-drilling miniscrews (mean, 17.6 Ncm; 95% CI, 16.8-18.4). Accordingly, the mean torque ratio of predrilling miniscrews was twice that of the self-drilling miniscrews.
Conclusions
An inverse relationship between MIT and MRT values was observed. The results suggest that relatively lower MIT values were more favorable to osseointegration than higher values.
Miniscrew implants have become an accepted and reliable method for providing temporary additional anchorage during orthodontic treatment. Because these miniscrews use the bone as anchorage, they have become broadly accepted as viable alternatives to extraoral devices in patients who either have insufficient dental support suitable for anchorage or are not compliant in wearing extraoral devices.
These miniscrew implants have several advantages—relatively simple implantation and removal procedures, and reduced costs—over the conventional methods of skeletal anchorage. Moreover, their small diameter allows placement into several areas of the maxilla and mandible that were previously unavailable, such as the alveolar bone between the roots of adjacent teeth.
Miniscrew implants are generally made of commercially pure titanium or titanium alloy. However, unlike conventional dental implants, miniscrews are manufactured with an untreated, smooth surface, because they are intended to be removed by the end of their clinical application. Consequently, osseointegration surrounding the miniscrew is not highly desirable, since it would complicate the miniscrew removal by increasing removal torque values.
Moreover, studies have shown that miniscrews do fracture at removal if the removal torque exceeds the limits that the miniscrew can withstand. Removal of the remnant of the miniscrew can be complex and might require additional surgical intervention with a trephine drill; this might lead to substantial bone removal and potential risks to the patient.
Application of immediate loading protocols has been suggested, when sufficient primary stability is achieved, as a practical approach to avoid the risks of osseointegration, since the loading is applied directly on the unhealed wound. However, recent clinical and experimental studies have demonstrated that even immediately loaded implants can become partially osseointegrated with various degrees of bone-to-implant contact.
Removal torque assessment has been suggested as a reliable method of determining the extent of osseointegration for conventional implants. However, only a few studies have been conducted to assess the effect of removal torque of miniscrew implants. Moreover, the findings of these studies are conflicting. Chen et al assessed the removal torque of miniscrews in several sites in the maxilla and the mandible. They concluded that the miniscrew stabilization to the bone was mainly obtained through mechanical retention rather than osseointegration, since immediate loading was used. In contrast, Favero et al, evaluating the removal torque of miniscrews in patients, concluded that the immediately loaded miniscrews were partially osseointegrated. However, in these studies, placement torque, a valid parameter to assess the primary stability of these miniscrews, was not assessed. The primary stability of miniscrew implants has been frequently associated with increased success rates of miniscrews.
The assessment of both placement and removal torque values should provide important information about the effect of the primary stability on the extent of osseointegration surrounding the immediately loaded miniscrews.
Therefore, the purpose of this study was to analyze the placement and removal torque values of orthodontic miniscrew implants in several sites in the maxilla and mandible.
Material and methods
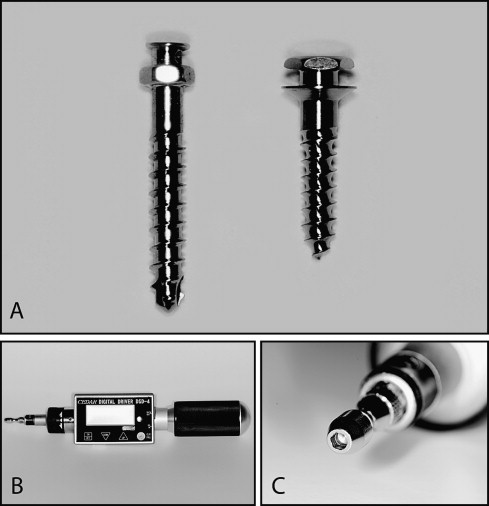
The sample consisted of 280 miniscrew implants that were systematically implanted into the bone of orthodontic patients, rigorously following the protocol of the Miniscrew Implant Group, Department of Orthodontics, Faculty of Dentistry, Chiang Mai University in Thailand, for safe miniscrew implant placement. The sample comprised 120 predrilling, cylindrical type (Sistema Nacional de Implantes, São Paulo, Brazil) and 160 self-drilling conical type (ACR Mini-Implant, BioMaterials Korea, Guro-gu, Seoul, Korea) titanium miniscrew implants ( Fig 1 , A ). All miniscrew implants were 1.5 mm in diameter and 6 or 8 mm in length. Miniscrew implants of 8-mm length were used in the dentoalveolar bone of the maxilla and the mandible, and those of 6-mm length were used in the midpalatal suture area. All miniscrew implants were used for orthodontic anchorage purposes during retraction of anterior teeth in patients who needed premolar extractions; 0.018-in slot preadjusted brackets were used in all patients. The same types of archwires and biomechanics were used for all patients.
Anterior retraction was performed with nickel-titanium closed-coil springs (50 g) attached to the heads of the miniscrew implants.
The subjects were 40 males and 55 females with ages ranging from 12.0 to 46.6 years (average age, 25.6 years; SD, 6.7 years). In accordance with the policies of the ethics committee at the Faculty of Dentistry, Chiang Mai University, we informed all patients about the risks and complications involving the use of miniscrew implants. All patients signed the informed consent form.
In this study, the planning and miniscrew placement into the dentoalveolar bone were performed by the same orthodontist (E.Y.S.), aided by a 3-dimensional (3D) surgical guide (Y&B Products, Chiang Mai, Thailand).
The 3D surgical guide was used to aid placement into the dentoalveolar bone to safely place the miniscrew implants between the roots of adjacent teeth.
Preoperative bitewing radiographs of the selected implant site were made by using the vertical bitewing technique aided by a film holder (Rinn XCP film holding system, Dentsply International, York, Pa) to ensure the precise mapping of the optimum implant site ( Fig 2 ). Radiographs were made with the 3D surgical guide in position to show the relationship of the guide to surrounding structures and available bone.
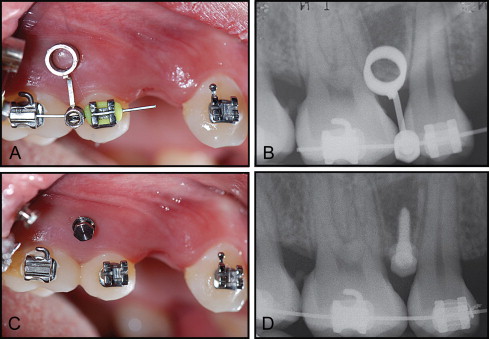
The 3D surgical guide was positioned as accurately as possible at the preselected miniscrew implant site. A radiograph was made to determine whether the image of the radiopaque tube was in the correct location. If it was not, the device was adjusted, and additional radiographs were made until a definitive implant placement position was determined that would not violate any surrounding structures. The radiographic image of the surgical guide projected onto the recipient bone oriented the ideal miniscrew implant placement position relative to the surrounding structures.
After the optimum implant position had been determined, the patients were instructed to rinse the mouth with chlorhexidine solution for 1 minute for hygiene in the oral cavity and to reduce the risks of infection during the surgical procedures. Infiltrative local anesthetic was used in all subjects. All miniscrews were placed through the attached gingiva. A high-speed diamond bur was used to expose the underlying bone. No flap elevation was performed.
For the predrilling miniscrew implants, a pilot hole was drilled with a 1.1-mm diameter spiral drill by using a manual driller with normal saline-solution irrigation to prevent excessive heat generation and to remove the bone debris from the drilling site.
The miniscrew implants were placed into the pilot hole through the surgical guiding tube with a manual screwdriver to reduce the risks of implant deviation during placement and to ensure the precise 3D placement into the preoperatively planned position.
The self-tapping miniscrew implants were placed directly through the gingival tissue into the bone, without creating a pilot hole, by using manual screwdrivers.
Maximum insertion torque (MIT) and maximum removal torque (MRT) were assessed with a torque wrench (Imada, Northbrook, Ill) ( Fig 1 , B ). The appropriate screwdriver of the corresponding miniscrew’s manufacturer was adapted into the Jacobs chuck of the torque wrench and applied to the miniscrew ( Fig 1 , C ). Placement and removal torque values of all miniscrews were assessed by the same orthodontist (E.Y.S.).
MIT was assessed simultaneously with the miniscrew placement procedures into the bone. The miniscrew implants were either placed into the prepared pilot hole (predrilling) or screwed directly into the bone (self-drilling).
The MIT was recorded at the terminal turning applied to tighten the miniscrew into the bone. The terminal turning was determined clinically, when the platform of the miniscrew gently touched the surface of the attached gingiva without provoking ischemia of the surrounding tissues.
Miniscrew implants were removed from each patient after the completion of their clinical application by using the torque device. The timing of removal was dictated by the orthodontic treatment plan. Miniscrew implants were able to function as skeletal anchorage against an orthodontic load for an average period of 44 ± 11 weeks with a minimal healing period of 2 weeks. MRT was assessed during the miniscrew removal procedures. The MRT value was considered the peak torque value necessary to unscrew the miniscrew. In general, the MRT value was the torque necessary to loosen the miniscrew at the initial turn.
The torque ratio (TR) of MRT to MIT was calculated. The TR of miniscrew implants is an important clinical criterion to determine the changes at the bone-miniscrew interface throughout orthodontic loading.
Statistical analysis
The statistical analyses were performed using the SPSS software program (version 17.0, SPSS, Chicago, Ill) on a personal computer. A paired t test statistical analysis was used to compare the MIT and the MRT of the predrilling and self-drilling miniscrew implants. The Student t test was used to compare the MIT and the MRT between the predrilling and self-drilling miniscrew implants and to determine any difference in the MIT values of the failed and successful miniscrews. Descriptive statistics and multiple comparisons between groups were performed with 1-way analysis of variance (ANOVA) and the post-hoc Tukey test to detect any differences between the locations of the miniscrews. The chi-square test was used to estimate differences in the success rates according to miniscrew type and placement site. The significance level was established at 0.5%.
Results
Failure of miniscrew implants was observed in 7 predrilling miniscrews and 12 self-drilling miniscrews. The failure rates of both groups were similar. The failures occurred 2 to 6 weeks after their placement. The most common site of failure was the dentoalveolar bone of the maxilla, followed by the mandible. No failure was observed in the miniscrews placed in the midpalatal suture ( Table I ). No statistically significant difference between the MIT values of successful and failed miniscrew implants was observed ( Table II ). Fractures during removal occurred in 4 predrilling miniscrews. One self-drilling miniscrew was fractured during placement in the midpalatal suture.
| Variables | Success (n) | Failure (n) | Total (n) | Success rate | P value | ||
|---|---|---|---|---|---|---|---|
| Miniscrew type | Placement site (n) | ||||||
| Predrilling | Maxilla | Dentoalveolar (78) | 74 | 4 | 78 | 94.9% | 0.027 |
| Midpalatal (27) | 27 | 0 | 27 | 100.0% | |||
| Mandible | Dentoalveolar (15) | 12 | 3 | 15 | 80.0% | ||
| Total (120) | 113 | 7 | 120 | 94.2% | |||
| Self-drilling | Maxilla | Dentoalveolar (98) | 90 | 8 | 98 | 91.8% | 0.161 |
| Midpalatal (30) | 30 | 0 | 30 | 100.0% | |||
| Mandible | Dentoalveolar (32) | 28 | 4 | 32 | 87.5% | ||
| Total (160) | 148 | 12 | 160 | 92.5% | |||
| Predrilling + self-drilling | Maxilla | Dentoalveolar (176) | 164 | 12 | 176 | 93.2% | 0.011 |
| Midpalatal (57) | 57 | 0 | 57 | 100.0% | |||
| Mandible | Dentoalveolar (47) | 40 | 7 | 47 | 85.1% | ||
| Total (280) | 261 | 19 | 280 | 93.2% | |||
| Variable | Torque (Ncm) | Significance | |||||
|---|---|---|---|---|---|---|---|
| Successful | Failed | ||||||
| n | Mean | SD | n | Mean | SD | ||
| Predrilling | 113 | 9.2 | 3.4 | 7 | 8.8 | 1.6 | NS |
| Self-drilling | 148 | 14.5 | 4.6 | 12 | 14.2 | 2.6 | NS |
A statistically significant difference was observed between the MIT and the MRT values of the successful predrilling and self-drilling miniscrew implants placed in the dentoalveolar bone sites of the maxilla and the mandible, and the midpalatal suture. For both predrilling and self-drilling miniscrews, the MRT values were significantly higher than the MIT values ( P <0.01). The TR of predrilling miniscrews (2.5) was twice that of the self-drilling miniscrews (1.2) ( Table III ).
| Placement site | Torque (Ncm) | P | Ratio | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | MIT | MRT | Difference | |||||||
| Predrilling | ||||||||||
| Maxilla | All sites | 113 | 9.2 | 3.4 | 22.6 | 3.4 | 13.4 | 2.8 | 0.0000 | 2.5 |
| Dentoalveolar | 74 | 7.2 | 1.4 | 21.1 | 2.5 | 13.9 | 2.8 | 0.0000 | 2.9 | |
| Mandible | Midpalatal | 27 | 14.5 | 1.6 | 26.9 | 2.0 | 12.4 | 2.7 | 0.0000 | 1.9 |
| Dentoalveolar | 12 | 12.4 | 1.2 | 24.5 | 2.0 | 12.1 | 2.7 | 0.0000 | 2.0 | |
| Self-drilling | ||||||||||
| Maxilla | All sites | 148 | 14.5 | 4.5 | 17.6 | 4.3 | 3.1 | 4.0 | 0.0000 | 1.2 |
| Dentoalveolar | 90 | 12.1 | 3.1 | 15.8 | 3.6 | 3.7 | 4.6 | 0.0000 | 1.3 | |
| Mandible | Midpalatal | 30 | 21.1 | 2.2 | 23.2 | 2.1 | 2.1 | 2.4 | 0.0001 | 1.1 |
| Dentoalveolar | 28 | 15.7 | 2.3 | 17.9 | 2.3 | 2.2 | 2.7 | 0.0001 | 1.1 | |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


