Many studies have documented the successful outcomes of dental implants, but have also reported the association of sensory disturbances with the surgical implant procedure. Postsurgical pain is a normal response to tissue injury, and usually resolves after the tissue heals. However, some patients who receive dental implants experience persistent pain even after normal healing. This article describes the basic anatomy and pathophysiology associated with nerve injury. The incidence and diagnosis of these problems, in addition to factors that result in the development of chronic persistent neuropathic pain and sensory disturbances associated with surgical implant placement, are discussed.
Key points
- •
There are multiple risk factors for the development of persistent postsurgical pain; however, the incidence of neurosensory disturbance after dental implant placement is relatively low.
- •
Many factors probably contribute to the development of a neurosensory deficit, including variations in implant techniques, the operator’s skill, the proximity to the nerve canal, and even the psychological status of patient.
- •
Some studies suggest that certain patients may be genetically more susceptible to neurosensory changes after nerve injury.
- •
Identifying the clinical features of chronic pain conditions and neuropathies after implant placement can assist in establishing a differential diagnosis.
Introduction
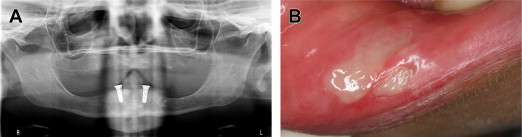
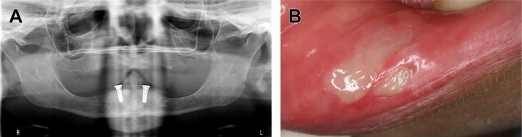
All dental structures are innervated by the trigeminal nerve, and common dental procedures can result in injury to one of the many branches of this nerve. These procedures, including the determination of local anesthesia, endodontic procedures ( Fig. 1 ), suture placement, soft-tissue manipulation ( Fig. 2 ), and third-molar extractions, can cause injury to branches of the trigeminal nerve. The nerve most commonly injured during dental procedures is the inferior alveolar nerve (64.4%), followed by the lingual nerve (28.8%). Injuries to these nerves are most often associated with dental anesthesia.

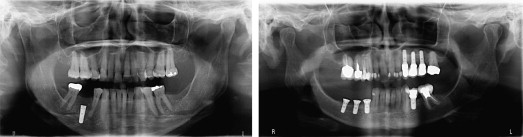
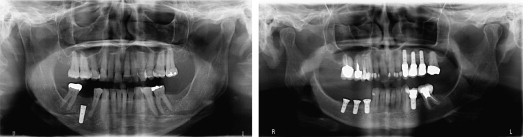
In recent years, the great success of dental implants has led to wide acceptance of such treatment. However, nerve injury and neurosensory impairment can occur after implant placement, even after accurate evaluation and careful treatment ( Fig. 3 ). A recent study found that 73% of dentists have reported that their patients have experienced neurosensory impairment after surgical implant procedures.
The published incidence of altered sensation after implant surgery is highly variable, ranging from 8.5% to 36%. In addition, published reports vary greatly in the terminology used to describe patients’ symptoms after nerve injury. Initially the term paresthesia was used to describe several forms of altered sensation reported by patients, including pain, warmth, cold, burning, numbness, and tingling.
The International Association for the Study of Pain has more clearly defined some of the most common conditions associated with neurosensory alterations ( Table 1 ). For example, anesthesia refers to complete loss of sensation; dysesthesia refers to an unpleasant form of altered sensation, such as burning, stinging, or stabbing; paresthesia refers to an altered sensation that is not necessarily unpleasant; allodynia refers to the pain produced by a nonpainful stimulus (light touch); and hyperesthesia is defined as an increased response to a painful stimuli. Although many types of neurosensory changes can occur, persistent pain after implant placement can be neuropathic. Very few data are available regarding the development of chronic persistent neuropathic pain after dental implant surgery.
| Term | Definition |
|---|---|
| Pain | An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage |
| Allodynia | Pain due to a stimulus that does not normally provoke pain |
| Analgesia | Absence of pain in response to stimulation that would normally be painful |
| Dysesthesia | An unpleasant abnormal sensation, whether spontaneous or evoked |
| Hyperalgesia | Increased pain from a stimulus that normally provokes pain |
| Hyperesthesia | Increased sensitivity to stimulation, excluding the special senses |
| Hypoalgesia | Diminished pain in response to a normally painful stimulus |
| Hypoesthesia | Decreased sensitivity to stimulation, excluding the special senses |
| Paresthesia | An abnormal sensation, whether spontaneous or evoked |
| Neuralgia | Pain in the distribution of a nerve or nerves |
| Neuritis | Inflammation of a nerve or nerves |
| Neuropathic pain | Pain caused by a lesion or disease of the somatosensory nervous system |
Injury to a major nerve or a peripheral branch during surgery can result in postsurgical neuropathic pain, some of which can be chronic and persistent. In 1991, Jemt evaluated 2199 implant-supported fixed prostheses in 384 patients, and found that only 3 mandibular implants were removed because of pain within 1 year of placement. With the increasing frequency of dental implant procedures, it is likely that more patients will experience chronic neuropathic pain and altered sensation in the future.
Patients with nerve injury can experience a slight loss or a complete loss of sensation, or even debilitating chronic pain. These symptoms can substantially hinder activities such as eating, drinking, speaking, and socializing, thereby greatly reducing the patient’s quality of life. Nerve injury and subsequent altered sensation after implant surgery may result in liability claims. Therefore, the clinician must be able to recognize and evaluate factors that can lead to nerve injury associated with implant procedures.
Introduction
All dental structures are innervated by the trigeminal nerve, and common dental procedures can result in injury to one of the many branches of this nerve. These procedures, including the determination of local anesthesia, endodontic procedures ( Fig. 1 ), suture placement, soft-tissue manipulation ( Fig. 2 ), and third-molar extractions, can cause injury to branches of the trigeminal nerve. The nerve most commonly injured during dental procedures is the inferior alveolar nerve (64.4%), followed by the lingual nerve (28.8%). Injuries to these nerves are most often associated with dental anesthesia.

In recent years, the great success of dental implants has led to wide acceptance of such treatment. However, nerve injury and neurosensory impairment can occur after implant placement, even after accurate evaluation and careful treatment ( Fig. 3 ). A recent study found that 73% of dentists have reported that their patients have experienced neurosensory impairment after surgical implant procedures.
The published incidence of altered sensation after implant surgery is highly variable, ranging from 8.5% to 36%. In addition, published reports vary greatly in the terminology used to describe patients’ symptoms after nerve injury. Initially the term paresthesia was used to describe several forms of altered sensation reported by patients, including pain, warmth, cold, burning, numbness, and tingling.
The International Association for the Study of Pain has more clearly defined some of the most common conditions associated with neurosensory alterations ( Table 1 ). For example, anesthesia refers to complete loss of sensation; dysesthesia refers to an unpleasant form of altered sensation, such as burning, stinging, or stabbing; paresthesia refers to an altered sensation that is not necessarily unpleasant; allodynia refers to the pain produced by a nonpainful stimulus (light touch); and hyperesthesia is defined as an increased response to a painful stimuli. Although many types of neurosensory changes can occur, persistent pain after implant placement can be neuropathic. Very few data are available regarding the development of chronic persistent neuropathic pain after dental implant surgery.
| Term | Definition |
|---|---|
| Pain | An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage |
| Allodynia | Pain due to a stimulus that does not normally provoke pain |
| Analgesia | Absence of pain in response to stimulation that would normally be painful |
| Dysesthesia | An unpleasant abnormal sensation, whether spontaneous or evoked |
| Hyperalgesia | Increased pain from a stimulus that normally provokes pain |
| Hyperesthesia | Increased sensitivity to stimulation, excluding the special senses |
| Hypoalgesia | Diminished pain in response to a normally painful stimulus |
| Hypoesthesia | Decreased sensitivity to stimulation, excluding the special senses |
| Paresthesia | An abnormal sensation, whether spontaneous or evoked |
| Neuralgia | Pain in the distribution of a nerve or nerves |
| Neuritis | Inflammation of a nerve or nerves |
| Neuropathic pain | Pain caused by a lesion or disease of the somatosensory nervous system |
Injury to a major nerve or a peripheral branch during surgery can result in postsurgical neuropathic pain, some of which can be chronic and persistent. In 1991, Jemt evaluated 2199 implant-supported fixed prostheses in 384 patients, and found that only 3 mandibular implants were removed because of pain within 1 year of placement. With the increasing frequency of dental implant procedures, it is likely that more patients will experience chronic neuropathic pain and altered sensation in the future.
Patients with nerve injury can experience a slight loss or a complete loss of sensation, or even debilitating chronic pain. These symptoms can substantially hinder activities such as eating, drinking, speaking, and socializing, thereby greatly reducing the patient’s quality of life. Nerve injury and subsequent altered sensation after implant surgery may result in liability claims. Therefore, the clinician must be able to recognize and evaluate factors that can lead to nerve injury associated with implant procedures.
Biology of the nerve cells and their response to injury
The basic structure of the nerve trunk consists of nerve fibers that are collectively organized into fascicles. Each fascicle is surrounded by a layer of loose connective tissue, the perineural layer, which protects the nerve fibers from compressive forces. Each nerve fiber is covered with well-organized tissue, called the endoneurial sheath, which consists of loose connective tissue and blood vessels. The most external surface surrounding the nerve trunk is composed of loose areolar connective tissue and is known as the epineurium.
A typical nerve fiber is composed of a cell body, dendrites, an axon, and axon terminals; this structure is surrounded by a myelin sheath and Schwann cells. The Schwann cells produce myelin, which plays an important role in facilitating nerve conduction. When a nerve fiber is subjected to mechanical injuries, it undergoes a series of structural and biochemical changes. Wallerian degeneration of the tissue distal to the injury begins, and macrophages then infiltrate the site to phagocytose and degrade the debris associated with the damaged myelin sheath and axons. Schwann cells proliferate to provide the metabolites needed for the regeneration of the nerve. The original neuron produces new axonal sprouts, which migrate toward the original endoneurial tube, thereby innervating the original tissue.
On occasion, collagen fiber is deposited and scar tissue forms within the endoneurial tube, obstructing the growth of a new axonal sprout and causing intermingling of the new axons. This bundle of new neural tissue is called a neuroma. In addition, the new tissue can grow toward other endoneurial tubes to establish connections and innervate other tissues. In this way certain impulses are transmitted from peripheral nerves to the central nervous system. The degree of complete nerve regeneration depends on the type and extent of the injury; therefore, recovery of sensation cannot always be expected after the nerve-regeneration process.
Classification of nerve injury
Seddon described 3 types of nerve injury: neurapraxia, axonotmesis, and neurotmesis. Neurapraxia is associated with a temporary blockade of conduction as a result of minor nerve injury. Axonotmesis is a moderate to severe type of nerve injury whereby the basic structure of the nerve tissue is still intact. However, Wallerian degeneration can occur. Neurotmesis is the most severe type of nerve injury, involving complete transection of the nerve that results in permanent nerve injury.
More recently, Sunderland described 5 types of nerve injuries; his classification is based on the anatomic structure of the nerve fibers. A first-degree nerve injury is associated with a temporary conduction block across the fiber without disruption of the anatomy of the axon. With this type of injury, nerve function usually returns to normal.
A second-degree nerve injury is associated with the loss of axon continuity; however, the endoneurial sheath remains intact. Compression or traction may cause transient ischemia, and recovery can be variable. However, regeneration of the axon within the endoneurial tube can occur.
A third-degree nerve injury results from trauma to the neural tissues that disrupts the continuity of the axon and the endoneurium, but leaves fasciculi intact. Regeneration of axons occurs after Wallerian degeneration, which is confined to within the fascicles. An intermingling of the fibers into other endoneurial tubes can occur if the endoneurial tube is occluded by scar tissue that may continue to hinder the regeneration of the axon. Complete recovery is usually not possible.
A fourth-degree nerve injury is associated with disruption of the axon, endoneurium, and fasciculi, but leaves loose connective tissue surrounding the nerve trunk. Regeneration of the axon is prevented by the development of fibrous scar tissue. Second-, third-, and fourth-degree nerve injuries are similar to Seddon’s axonotmesis, depending on the severity of the nerve injury. A fifth-degree nerve injury, the most severe form, consists of complete loss of nerve trunk continuity and is equivalent to Seddon’s neurotmesis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


