Nerve trauma caused by dental implant placement is associated with altered sensation and chronic pain. Complete or partial loss of sensation is often reported by patients who have experienced nerve trauma during implant surgery. Some patients report persistent pain and neurosurgery disturbance long after the normal healing time has passed. In addition, neuropathic pain is reported after implant surgery. Practitioners who place dental implants must be familiar with the differential diagnosis, prevention, and management of neuropathic pain. This article provides insights into the prevention and management of neurosensory deficits and chronic persistent neuropathic pain and considerations for patient referral.
Key points
- •
Although the success rates associated with implants are good, adverse events can occur.
- •
Disruption of normal sensation and pain can be consequence of implant placement.
- •
Clinicians must be aware of these adverse consequences and avoid them whenever possible; avoidance can be best achieved by careful advanced planning before implants are placed.
- •
When neurosensory alterations or pain results, pharmacologic management can be helpful.
- •
Microsurgical repair of damaged nerve tissue should be considered.
Introduction
Nerve injury associated with implant placement may occur during injections of local anesthetic, osteotomy preparation, or implant placement. One of the most common complications associated with nerve injury during implant surgery is altered sensation. Patients often experience complete or partial loss of sensation, such as perceptions of touch, pressure, or temperature. These symptoms may seriously affect a patient’s ability to perform daily activities, such as drinking and eating, and may also lead to traumatic biting of soft tissues (lips or cheeks) during mastication. In addition to these symptoms, some patients may also experience severe pain that can be debilitating.
Persistent pain after implant placement can be neuropathic in nature. Neuropathic pain (NP) is defined as “pain initiated or caused by primary lesion or dysfunction in the nervous system.” In addition, NP may be associated with paresthesia, dysesthesia (burning, stinging, or stabbing sensations), sensory deficits, allodynia, and hyperesthesia.
As described in the article by Al-Sabbagh and colleagues elsewhere in this issue, the pathophysiology of NP is complex and has not yet been completely elucidated. Treatment is complicated by the fact that NP does not normally respond well to conventional analgesics and opioids. Currently, many therapeutic approaches are being explored, but to date none has been consistently helpful. Because NP is often intense, debilitating, and resistant to treatment, practitioners should be familiar with the basic mechanisms that contribute to NP disorders (see article by Al-Sabbgh and colleagues) so that they can plan procedure more carefully and often prevent these complications. Also, understanding that certain risk factors predispose patients to NP can help minimize its occurrence.
Introduction
Nerve injury associated with implant placement may occur during injections of local anesthetic, osteotomy preparation, or implant placement. One of the most common complications associated with nerve injury during implant surgery is altered sensation. Patients often experience complete or partial loss of sensation, such as perceptions of touch, pressure, or temperature. These symptoms may seriously affect a patient’s ability to perform daily activities, such as drinking and eating, and may also lead to traumatic biting of soft tissues (lips or cheeks) during mastication. In addition to these symptoms, some patients may also experience severe pain that can be debilitating.
Persistent pain after implant placement can be neuropathic in nature. Neuropathic pain (NP) is defined as “pain initiated or caused by primary lesion or dysfunction in the nervous system.” In addition, NP may be associated with paresthesia, dysesthesia (burning, stinging, or stabbing sensations), sensory deficits, allodynia, and hyperesthesia.
As described in the article by Al-Sabbagh and colleagues elsewhere in this issue, the pathophysiology of NP is complex and has not yet been completely elucidated. Treatment is complicated by the fact that NP does not normally respond well to conventional analgesics and opioids. Currently, many therapeutic approaches are being explored, but to date none has been consistently helpful. Because NP is often intense, debilitating, and resistant to treatment, practitioners should be familiar with the basic mechanisms that contribute to NP disorders (see article by Al-Sabbgh and colleagues) so that they can plan procedure more carefully and often prevent these complications. Also, understanding that certain risk factors predispose patients to NP can help minimize its occurrence.
Initial therapeutic considerations and prevention of nerve injury
When a nerve injury is suspected, clinicians must be able to recognize the cause, type, and extent of the injury. Local anesthetic blocks have been reported to cause trauma to nerves. It has been reported that 25% to 29% of local anesthetic injections that cause nerve injuries result in a permanent change to the nerve tissue. Avoiding multiple injections can help prevent iatrogenic nerve injury related to local anesthetics. The treatment of patients with nerve injury includes antiinflammatory medications (steroids or nonsteroidal antiinflammatory drugs [NSAIDs]) to reduce the neural inflammation, along with counseling and reassurance.
It is important to appreciate the need for local anesthetic blocks even when surgical procedures are performed with patients under sedation. Preemptive analgesia with local anesthetics, opioids, antiinflammatories, and glucocorticoids has been associated with reduced postoperative pain, less postoperative use of analgesics, and shorter hospital stays. Lee and colleagues tested whether perineural injections of dexamethasone and bupivacaine exerted preemptive analgesic effects in a nerve injury model. They found that mechanical allodynia did not develop and that preoperative infiltration of dexamethasone and bupivacaine exerted a substantially better analgesic effect than did infiltration of dexamethasone or bupivacaine alone. Bupivacaine has been shown to reduce postoperative pain and to block sensory input beyond the duration action of the local anesthetic.
Another consideration that may lead to nerve tissue injury is the heat produced by an implant drill. The pressure, speed, sharpness, time of use, and irrigation system of the drill are often directly linked to the production increased heat during implant placement. The neural tissue is sensitive and easily damaged by heat stimuli. Increased temperature has been associated with a reduction in the ability of bone tissue to repair and regenerate. It can also enhance osteoclastic activity, thereby resulting in the failure of the osseointegration process.
Continuous contact between implant drill and bony wall occurs during the implant osteotomy procedure. Sometimes the implant drill can slip because of the presence of softer bone in the direction of drilling; such slipping can cause mechanical trauma to the structures, in particular the nerves. Therefore, the risk of nerve injury can be reduced by careful evaluation of the thickness and density of the bone mass surrounding the nerve and by the use of less force during implant drilling as the bur approaches the canal.
Continuous irrigation of the bur helps reduce heat generation and prevents clogging by debris during implant osteotomy procedures. The presence of certain chemicals in the irrigating solutions has been associated, however, with chemical nerve injury, particularly when the osteotomy is prepared close to the nerve canal. The use of sodium hypochlorite solution is not recommended for irrigating the implant bed because it can result in an alkalemic nerve injury.
Both the buccal and the lingual plates play an important role in determining the reference point for all of the measurements required during the implant osteotomy procedure. Bone loss in the alveolar ridge after tooth extraction usually occurs in the buccal aspect, resulting in an uneven ridge in which the lingual side is higher than the buccal side. Clinicians should keep this in mind when establishing a reference point. The lingual side generally provides more available vertical bone measurements than the buccal. Therefore, the amount of bone available and the location of the nerve canal should be precisely measured with a cone-beam CT (CBCT) scan. As a preventive measure for nerve injury, a CBCT scan is useful for appreciating the 3-D relationship of the implant and the surrounding structures, including the nerve canals and foramina ( Fig. 1 ). This image provides 3-D measurements that help clinicians avoid unnecessary iatrogenic nerve trauma. It has been reported that nerve injuries are less likely to occur when CBCT scans are used to evaluate the site before implant placement.
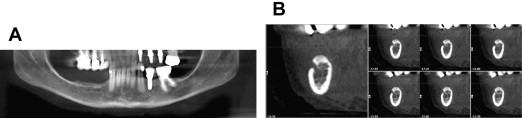
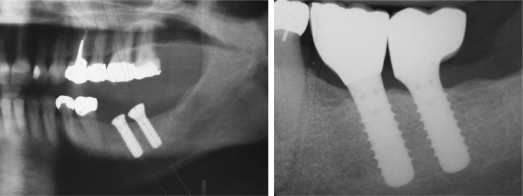
Even after careful evaluation and measurements, nerve injury can occur during implant placement. A safety zone of approximately 2 to 3 mm between implant apex and nerve canal helps minimize direct nerve trauma during implant procedures ( Fig. 2 ). Direct mechanical injury to the nerve by implant intrusion can cause either encroachment of the implant into the nerve canal or complete transection of the nerve. Such severe nerve injury induces retrograde degeneration proximally and leads to cell body degeneration. It has been reported that injuries at the ramus region (proximal site) are more serious than those that occur at the area of the mental foramen (distal site).
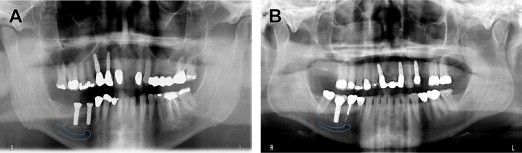
If the apex of an implant is placed close to the nerve canal, secondary injuries to the nerve may occur ( Fig. 3 ). These injuries include chipping of the roof of the inferior alveolar nerve (IAN) canal; this injury can result in the accumulation of debris and the development of compression injuries to the IAN. Compression injuries can produce altered sensation after implant placement and can be treated by immediate removal of the implant to relieve the compression. As discussed previously, the perineurium layer protects the nerve fibers from compression or stretch injuries. When pressure and elongation of more than 30% occur, however, severe damage to the axon is possible. Occasionally, severe nerve injuries can lead to anesthesia with loss of function accompanied by radiating pain. Neuropathic and myofascial pain is associated with positioning of the implant in the vicinity of the nerves. Rodríguez-Lozano and colleagues reported a patient who experienced NP 6 months after implant placement. They also reported that NP patients may not respond to implant removal and may require a consultation with a pain specialist or a multidisciplinary clinic. Such cases may result from alterations within the central dorsal horn, such as central sensitization associated with the nerve injury. When such sensitization occurs, further surgical procedures in the area, such as removing the implant, may only exaggerate the NP.
In conclusion, surgical procedures associated with the placement of dental implants have been associated with several types of nerve injuries, even when skilled clinicians use careful, well-planned procedures. Some of the common sources of nerve injuries are local anesthetic injections, flap reflection, suturing, soft tissue swelling, and pressure around nerves. Because resolution of nerve injury is unpredictable and NP is often resistant to treatment, careful planning in advance of treatment is the most effective treatment strategy.
Treatment options
Effective treatment depends not only on the nature and degree of the nerve injury but also on the ability of clinicians to evaluate the trauma. In most cases, the injury is likely related to mandibular dental implants. The treatment of patients with iatrogenic nerve injuries related to dental implants should be aimed at managing symptoms as soon as they become evident. Decisions about the type of nerve injury and the timing of treatment are vital to the outcome of patients. The management of NP involves primarily pharmacotherapy. Invasive and irreversible approaches should generally be avoided. A comprehensive evaluation should include psychological and behavioral aspects. This type of pain is often best managed by a multidisciplinary team composed of orofacial pain dentists, neurologists, neurosurgeons, psychologists, and other specialists as appropriate.
Pharmacologic Management
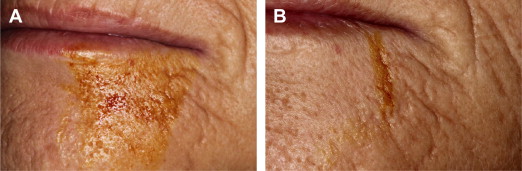
Immediately after the surgical procedure, the inflammatory process begins. This process includes the activation of several cytokines, chemokines, and inflammatory mediators, such as interleukin 1β and tumor necrosis factor α. If the nerve has been traumatized during the surgical procedure, these inflammatory mediators contribute to the development of NP by activating the neurons and their nociceptors. Therefore, antiinflammatory drugs are usually recommended for patients with nerve injuries, and case reports have recommended NSAIDs for such patients. Khawaja and Renton reported a patient who experienced paresthesia after implant placement. The clinician prescribed ibuprofen, 800 mg; amoxicillin, 500 mg (both 3 times a day); and prednisolone, 50 mg once daily, for 5 days, tapered to 10 mg for next 5 days. Although the investigators reported pain reduction, the implant was immediately removed. Therefore, it is difficult to determine the reason for the success. Misch and Resnik recommended the use of steroids in addition to high doses of NSAIDs, such as ibuprofen (600–800 mg) 3 times daily for 3 weeks, but no supportive data were presented ( Fig. 4 ).
Corticosteroids, commonly used antiinflammatory drugs, are often recommended for patients with neurosensory deficits after nerve injury. Reports have suggested that these drugs can help prevent the formation of neuromas; therefore, higher dosages have been recommended within the first week after the nerve injury. It has been suggested that patients with persistent dysesthesia after dental implant procedures should be given a series of injections containing a mixture of dexamethasone, 4 mg/mL, and 2% lidocaine with 1:100,000 epinephrine (50:50 mixture) into the most painful area. These injections should be repeated until the pain symptoms disappear. Misch and Resnik suggested that if known trauma (observed nerve injury) or compression of the nerve occurs during the implant osteotomy, 1 to 2 mL of dexamethasone (4 mg/mL) should be applied topically for 1 to 2 minutes to minimize neural inflammation and soft tissue swelling that can compress the nerve. In addition, an oral regimen of dexamethasone should be administered for 6 days.
Other pharmacologic medications that have been recommended for patients with nerve injuries are antidepressants and anticonvulsants. Park and colleagues evaluated the response of 85 patients with trigeminal nerve injury after implant surgery to antidepressive and anticonvulsant drugs. Patients reported a 24.8% reduction in pain after 12 weeks of anticonvulsant and antidepressant medications; however, the study had no control group ( Fig. 5 ).


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


