Introduction
In this study, we sought to assess the perception of changes in soft-tissue profile after Herbst appliance treatment by comparing facial profile silhouettes before treatment, immediately after treatment, and 2 years after treatment, as examined by orthodontists, general dentists, and laypersons.
Methods
The sample comprised 21 patients (mean age, 9.5 ± 0.5 years), who were treated with the Herbst appliance for a mean period of 12 (±1.1) months. Three lateral cephalograms were obtained at different times: baseline, immediately after removal of the Herbst appliance, and 2 years after removal of the appliance. The 63 resulting profile silhouettes were evaluated by 120 examiners divided into 3 groups: orthodontists, general dentists, and laypersons. The examiners were instructed to choose their preferred profile and note how much change they perceived across profiles using a visual analog scale.
Results
All groups of examiners preferred the posttreatment profiles. However, on quantitative assessment, the magnitudes of changes in the profile were found to be variable and rather small, with laypersons quantifying the greatest magnitude of change.
Conclusions
Early Herbst appliance treatment produced positive changes in the facial profile that were visually appreciable both immediately after removal of the appliance and 2 years after treatment.
Highlights
- •
Early treatment with the Herbst appliance promoted positive changes on the profile.
- •
These changes were noticeable by orthodontists, general dentists, and laypersons.
- •
The laypersons group quantified the greatest changes in the profiles.
Facial esthetics is a key objective of orthodontic treatment, as cited by both dentists and patients. Several studies have noted that esthetics and improved quality of life are among the leading motivations for seeking orthodontic care. Class II skeletal malocclusions are some of the most frequent conditions that prompt this search.
Class II Division 1 malocclusions caused by mandibular deficiency are associated with soft-tissue characteristics that involve a high degree of facial convexity, with a normal nasolabial angle, decreased mentolabial angle, recessed chin and lower lip, lip incompetence, and a short chin-to-neck length. These characteristics can have a negative emotional impact on the developing child and may even hinder social interactions. Treatment of these malocclusions depends on several factors, such as patient age, esthetic compromise, and severity of malocclusion. It may be performed in 2 phases (orthopedic and orthodontic with a fixed appliance) or in 1 phase (fixed appliance alone).
The possibility of stimulating mandibular growth with orthopedic appliances as a treatment strategy for Class II malocclusions remains highly controversial in the literature. Due to its continuous mechanism of action, the Herbst appliance has aroused great interest in the orthodontic community since the late 1970s. Several studies have evaluated its effects on skeletal, dentoalveolar, and soft tissues, both immediately and in the long term. A recent meta-analysis concluded that the Herbst appliance is effective in the treatment of Class II malocclusions.
Protocols for early treatment with the Herbst appliance advocate its use in the prepubertal stage—ie, before the adolescent growth spurt. These protocols are indicated for patients with severe Class II malocclusion with substantial esthetic and psychosocial impacts. Patients are usually at the end of the first transitional period or the start of the intertransitional period of the mixed dentition at the time of treatment. This means that prolonged retention—until the permanent premolars and canines erupt and reach the occlusal plane—is needed to maintain the stability of correction. Therefore, nighttime use of a removable bionator appliance is recommended for retention in the orthopedic phase, in preparation for future placement of a fixed appliance once the permanent dentition has erupted completely.
Some cephalometric studies have evaluated the effects of Herbst appliance treatment on the soft-tissue profile. These effects are characterized by a reduction in facial convexity due to anterior displacements of the chin and lower lip, as well as some upper lip retrusion, resulting from the dental and skeletal changes induced by the appliance. However, the magnitudes of these changes are variable; this questions whether the impact of this treatment strategy is clinically perceptible and stable over time.
Although profile silhouette studies have been used to evaluate perceived changes after several orthodontic treatment modalities, no studies with this method have been conducted to assess early treatment with the Herbst appliance. In this context, we sought to assess the perception of changes in soft-tissue profile induced by treatment with a Herbst appliance, by comparing facial profile silhouettes before treatment, immediately after treatment, and 2 years after treatment, as evaluated by orthodontists, general dentists, and laypersons.
Material and methods
This study was approved by the research ethics committee of Centro Universitário Uninovafapi (protocol CAAE 0175.0.043.000-07). Written informed consent was obtained from all patients, and consent forms were stored on file.
The sample size calculation was based on a pilot study conducted with 12 examiners. Using the StatsToDo software environment ( http://www.statstodo.com , StatsToDo Trading Pty, Queensland, Australia), for statistical power of 80% and significance of 0.05, we obtained an effect size of 0.75 and found that a sample size of 40 examiners per group would be sufficient.
Assessments of changes in soft-tissue profiles after Herbst appliance treatment were conducted on a sample of 21 patients (12 girls, 9 boys; mean age, 9.5 years ± 6 months) who were treated consecutively with the device for a mean period of 12 months (±1.1 months).
The inclusion criteria were as follows: (1) Class II skeletal pattern, as determined by an ANB angle of 5° or greater and a Wits appraisal of 2 mm or greater; (2) full-step Class II Division 1 dental relationship; (3) overjet of 6 mm or greater; (4) mixed dentition (intertransitional period), with transverse maxillary deficiency and no significant crowding in the mandibular arch; transverse maxillary deficiency was assessed by manipulating models until a Class I molar relationship was obtained; 8 subjects had a posterior crossbite in maximum intercuspation; (5) no previous orthodontic treatment; and (6) bone age corresponding to cervical vertebral maturation stage I (initiation), as determined by morphologic analysis of the second, third, and fourth cervical vertebrae.
The exclusion criteria were vertical facial growth pattern, developmental syndromes or abnormalities, missing teeth, and anterior open bite. The dental and skeletal characteristics of the included patients are described in Table I .
| Cephalometric parameter | Mean | SD |
|---|---|---|
| SNA (°) | 81.4 | 2.6 |
| SNB (°) | 74.5 | 2.9 |
| ANB (°) | 6.9 | 1.6 |
| Wits (mm) | 3.5 | 1.2 |
| NAPg (°) | 13.4 | 4.0 |
| SN.GoGn (°) | 33.4 | 4.3 |
| 1.PP (°) | 114.4 | 7.2 |
| IMPA (°) | 94.3 | 6.0 |
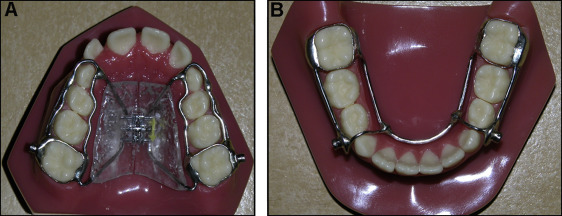
The anchorage system used for the maxillary arch was a modified Haas-type palatal expander with buccal and lingual connecting bars ( Fig 1 , A ). For the mandibular arch, a modified lingual arch with a connecting bar in the canine region was used ( Fig 1 , B ).
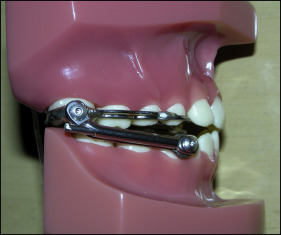
A telescoping mechanism, which essentially limited motion to opening and closing and greatly restricted lateral excursions ( Fig 2 ), was used to connect the maxillary and mandibular anchorage appliances. Patients wore the Herbst appliance for a mean period of 12 months. This was followed by nighttime use of a bionator retainer until eruption of the permanent premolars and canines.
Changes in soft-tissue profile were assessed on lateral cephalograms obtained at 3 distinct time points: T1, at baseline, before placement of the Herbst appliance; T2, immediately after removal of the appliance, after 12 (±1.1) months of use; and T3, 2 years after removal of the Herbst appliance. Since the length of follow-up was 3 years, using an untreated control group would have been ethically unjustifiable.
Cephalometric tracings were done manually by a previously calibrated examiner (R.M.I.C.) and scanned without magnification. The silhouettes were then made with CorelDraw X6 (Corel, Ottawa, Ontario, Canada) by a technician with no knowledge of the study ( Fig 3 ).
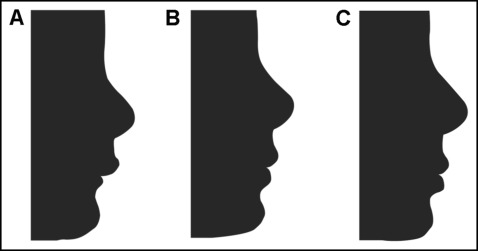
Two photo albums were made with these images, each of which contained 2 printed profile silhouettes in 10 × 15-cm format per page. Image organization (T1 and T2 or T1 and T3) and placement (left or right) on the pages were random.
A total of 120 examiners (all from Teresina, Piauí, Brazil) participated in the study. The examiners were divided into 3 groups of 20 men and 20 women each: orthodontists, 40 specialist orthodontists; dentists, 40 general dentists with no orthodontic training; and laypersons, 40 persons with no knowledge of dentistry.
The examiners received the photo albums containing all 63 profiles and were given 1 minute to analyze each page. The examiners’ first impressions were final; they were not allowed to revise their findings. Along with each album, the examiners were also given instructions on how to assess images and a grading sheet on which to record their findings. The category of each examiner (orthodontist, general dentist, or layperson) was noted on the header of the grading sheet. The examiners were instructed to choose their preferred profile (A or B) and note how much change they perceived between the 2 images by marking on a visual analog scale (VAS).
The VAS consisted of a 10-cm line. A score of zero on the VAS (left end) denoted that the compared profiles looked the same to the examiner, whereas a mark on the opposite (right) end of the scale denoted that the 2 profiles looked very different.
Method error was evaluated by the intraclass correlation coefficient, on the basis of VAS scores assigned by the examiners to 2 duplicates (1 in each album). These duplicates were shown randomly, mixed with the other pages. The result (0.79) was consistent with good reliability.
Statistical analysis
Statistical analysis was performed with SPSS software (version 20.0; IBM, Armonk, NY). To test for associations between examiner groups for T1 and T2 profiles, and T1 and T3 profiles, we used the chi-square test and the contingency coefficient. The significance level was set at 5% ( P ≤0.05). The Kolmogorov-Smirnov test confirmed that the VAS data were normally distributed. The perceived changes from T1 to T2 profiles and from T1 to T3 profiles on the VAS were assessed by analysis of variance (ANOVA) with the Tukey post hoc test ( P ≤0.05).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


