It is universally agreed that maxillofacial trauma is rare in children. Several retrospective reviews have highlighted that the pediatric population accounts for 5% of all facial fractures, with a reported range in the literature of 1.5-15%. Mid-facial fractures, in particular, make up an even smaller percentage of fractures, 0.2%-8%, depending on one’s anatomic delineation of the middle third of the face. It is postulated that the lower incidence of mid-facial injury is related to the anatomic protection of the face afforded by the prominent calvaria of children, as well as the incomplete development of the paranasal sinuses, the flexibility of their osseous suture lines, and their thicker facial adipose tissue. In addition, it has been suggested that the lower incidence of mid-facial fractures might be the result of under-reporting or outright exclusion of certain injuries, such as dentoalveolar injury and isolated nasal bone fractures as part of the mid-face complex. Nasal and dentoalveolar injuries can often be treated in an outpatient setting and are therefore often presumably excluded from hospital logs. For the purposes of this text, we include in our discussion of fractures of the mid-facial skeleton the following: orbital floor, nasal and naso-orbito-ethmoid complex (NOE), zygomaticomaxillary complex, and Le Fort fractures.
Epidemiologic characterization of facial fractures in children began with the work of Rowe in the 1960s and continued with the work of Kaban and Posnick in the decades that followed. Since that time, several authors in varied socioeconomic and geographic situations have broadened our understanding of this process, and some significant trends have emerged from their work and should be mentioned in the foregoing discussion of mid-facial injuries. With respect to pediatric facial trauma in general, children aged 6 to 12 years are most commonly afflicted, with males being more prone to injury than females. Moreover, although there is no consistent etiologic front runner in the retrospective surveys examined, road traffic accidents (RTAs) and falls are among the major causes, depending on the setting of the study. Additionally, the majority of mid-face fractures require operative intervention. Open reduction plus internal fixation appears to be advocated more and more by contemporary surgeons. Several authors have expressed the need for accurate reduction and stable internal fixation for complex pediatric facial trauma. This management philosophy is based on the understanding that the secondary reconstruction of residual traumatic deformities can be difficult, as well as a better understanding of the impact of surgery on the growing facial skeleton.
Developmental Anatomy and Its Surgical Considerations
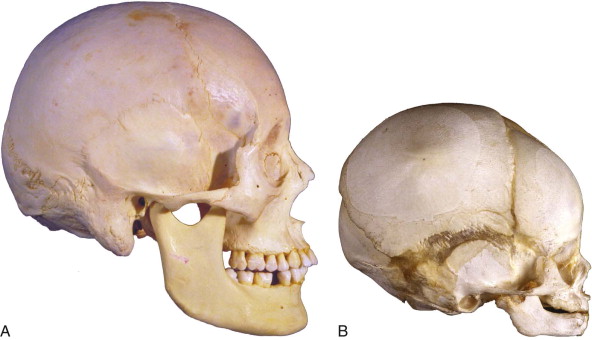
A thorough understanding of craniofacial development will not only aid in appreciating the epidemiologic data presented but also help guide the management of injuries in the pediatric population. During infancy and early childhood there is a significant increase in head circumference to accommodate brain growth. By the end of the sixth year of life, 90% of cranial growth has occurred, the sutures are well articulated, and orbital maturity is almost reached. This provides the characteristic facial appearance in early childhood of a prominent forehead and orbits with a relatively underdeveloped (and protected) lower facial skeleton ( Fig. 97-1 ). Palatal, premaxillary, and midline maxillary suture growth is complete, with obliteration of sutures by the age of 8 to 12. The lower two thirds of the face exhibits downward and forward growth, which exposes the bones of the face to injury. Eruption of deciduous teeth occurs in the first 2 years of life, and eruption of the permanent dentition is complete by the age of 12 to 13. Permanent tooth eruption accounts for much of the vertical growth of the lower two thirds of the face. The primary- and mixed-dentition period, or the time between eruption sequences, poses a challenge in terms of pathogenesis and treatment modalities, specifically with respect to fracture patterns and fixation techniques, because of anatomic differences in primary tooth morphology and the presence of tooth buds in the facial skeleton. Permanent tooth buds in the maxilla and mandible create areas of structural weakness in the bone. The presence of tooth buds limits the placement of certain plates and screws for fear of damaging the developing dentition. Furthermore, eruption of the permanent teeth and exfoliation of the primary teeth can also make maxillomandibular fixation (MMF) quite difficult. On the other hand, ongoing growth and eruption of the permanent dentition can often compensate for minor inaccuracies in reduction and fixation. Other general anatomic differences between the adult and pediatric patient populations are that children have a thinner cortex and greater thickness of medullary bone, a higher cranial-to-facial ratio (8 : 1 in infants versus 2 : 1 in adults), more facial adipose tissue (the buccal and labial fat pads), more elastic bone (lending to greenstick fracture), and underdeveloped paranasal sinuses.
Airway Assessment and PeriOperative Management
Thorough airway assessment of injured pediatric patients is critical, and this cannot be overemphasized in those with facial trauma. The advent of fiberoptic intubation has resulted in a significant decline in the use of tracheostomy for patients with craniofacial trauma, particularly mid-face trauma. Additionally, the use of rigid internal fixation has helped expedite postoperative extubation by minimizing the use of MMF. Despite these advances, one must be cognizant of the smaller-caliber airway, shorter trachea, floppy epiglottis, and flaccid oral and pharyngeal soft tissues in younger children, all of which increase the rate of obstruction and airway resistance and thus make intubation more difficult.
Resuscitative efforts in children should center on maintaining the airway and avoiding bradycardia. Hypercapnia (and the resultant hypoxemia) depress central nervous system and cardiac function. Because cardiac output is rate-dependent in pediatric patients, bradycardia can result in severe circulatory compromise and should be treated aggressively. The lower total body volume in children must also be considered during initial management surveys. Hemorrhage from scalp lacerations and other injuries may lead to clinically significant hypotension and result in precipitous decompensation. It would also behoove the surgeon to have an awareness of associated injuries, particularly after high-velocity blunt trauma, such as those seen with RTAs. Posnick and co-authors reported that 33% of patients who suffered maxillofacial injuries had concurrent injuries to other anatomic sites/organ systems (head, 42%; extremities, 24%; eye, 22%; thorax, 10%; and abdomen, 2%). Kaban reported concurrent injuries in 20% of patients ; however, the predominant mechanism of injury was not RTA, as in the sample of Posnick and colleagues.
Airway Assessment and PeriOperative Management
Thorough airway assessment of injured pediatric patients is critical, and this cannot be overemphasized in those with facial trauma. The advent of fiberoptic intubation has resulted in a significant decline in the use of tracheostomy for patients with craniofacial trauma, particularly mid-face trauma. Additionally, the use of rigid internal fixation has helped expedite postoperative extubation by minimizing the use of MMF. Despite these advances, one must be cognizant of the smaller-caliber airway, shorter trachea, floppy epiglottis, and flaccid oral and pharyngeal soft tissues in younger children, all of which increase the rate of obstruction and airway resistance and thus make intubation more difficult.
Resuscitative efforts in children should center on maintaining the airway and avoiding bradycardia. Hypercapnia (and the resultant hypoxemia) depress central nervous system and cardiac function. Because cardiac output is rate-dependent in pediatric patients, bradycardia can result in severe circulatory compromise and should be treated aggressively. The lower total body volume in children must also be considered during initial management surveys. Hemorrhage from scalp lacerations and other injuries may lead to clinically significant hypotension and result in precipitous decompensation. It would also behoove the surgeon to have an awareness of associated injuries, particularly after high-velocity blunt trauma, such as those seen with RTAs. Posnick and co-authors reported that 33% of patients who suffered maxillofacial injuries had concurrent injuries to other anatomic sites/organ systems (head, 42%; extremities, 24%; eye, 22%; thorax, 10%; and abdomen, 2%). Kaban reported concurrent injuries in 20% of patients ; however, the predominant mechanism of injury was not RTA, as in the sample of Posnick and colleagues.
Diagnostic Methods
A thorough history and physical examination are critical in both determining a definitive diagnosis and guiding further diagnostic tests, namely, imaging. Determination of the cause, as well as the amount and direction of traumatic force, helps guide the diagnostic evaluation. Particular attention to and documentation of the child’s mental status, visual examination, airway status, facial proportions, and occlusion are essential in arriving at a diagnosis. Often by the history and physical examination alone, the type and extent of maxillofacial injury can be characterized. Confirmation of the presence and severity of facial fractures is, however, imperative. Computed tomography (CT), when available, has largely replaced plain film radiography as the modality of choice for the evaluation of trauma patients, both pediatric and adult. With the exception of perhaps panoramic radiographs for evaluation of mandibular fractures, CT is superior to conventional radiography in diagnostic accuracy, anatomic localization of fractures, and detection of occult or greenstick fractures, especially in the context of fractures among tooth buds. Coronal reformatted images are particularly useful in mid-facial trauma for evaluating changes in facial volume and width, data essential in the evaluation of orbital fractures and NOE fractures. With the advent of multiplanar reformatting and three-dimensional (3D) rendering of CT image data, very precise depiction of anatomic details can be obtained, which will help guide accurate surgical reduction of fractures, as well as fixation. In response to the obvious disadvantage of CT (exposure to radiation), ultrasound (US) has emerged as a safe, inexpensive, and in certain anatomic regions, accurate alternative or adjunctive diagnostic modality. In the depiction of orbitozygomatic complex fractures, US reportedly has a sensitivity and specificity similar to that of CT. It should be noted, however, that edema and soft tissue emphysema both dramatically decrease the sensitivity of US, thus making its broad application less than ideal for a significant proportion of trauma patients. Moreover, US should not be performed on open wounds. That said, US is less widely established, and currently there are not enough data available to support its use as a primary method of diagnosis.
Orbital Floor Fractures
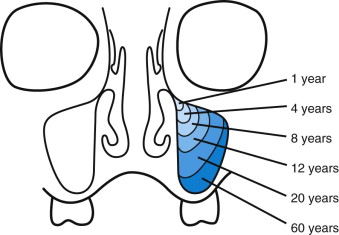
Whether seen in isolation or in association with complex facial trauma patterns, orbital floor fractures are rare in children. The frequency of such fractures does, however, increase with increased pneumatization of the maxillary sinuses. Maxillary sinus development begins between the first and second trimesters, and growth continues until completion of pneumatization after puberty ( Fig. 97-2 ). The usual mechanism of orbital fractures is a direct blow to the eye transmitted through soft tissue down the thin bone of the orbital floor or medial wall. Findings on physical examination may include periorbital edema and ecchymosis, subconjunctival hemorrhage, enophthalmos, diplopia or restriction of ocular movement, and anesthesia or paresthesia along the distribution of the infraorbital nerve. All pertinent physical findings should be documented, and ophthalmologic consultation is suggested in most cases. Aside from actual injury to the globe (which occurs in up to 24% of orbital fractures), entrapment of extraocular muscle and periorbital tissue is always a concern. Forced duction tests can be difficult on an adult, let alone a pediatric patient, and sedation or even general anesthesia may be required to perform such tests if there is clinical suspicion of entrapment. Other signs should alert the clinician to entrapment, including vagally mediated nausea and vomiting or sinus bradycardia, a phenomenon referred to as the oculocardiac or oculovagal reflex.
Fine-cut, 1-mm CT slices with 3D reconstruction provide the most accurate anatomic assessment of the bony orbit. Sagittal and coronal views enable accurate views of the orbital floor and sinus below and highlight changes in volume better than conventional radiography does. Findings on CT may include blow-out or blow-in fractures of the orbit, soft tissue and muscle entrapment, and even retrobulbar hematoma. Retrobulbar hematoma can lead to acute orbital compartment syndrome—a treatable ocular emergency. Clinical signs of concern are pain, diplopia, proptosis, loss of pupillary response, and progressive visual deficit. Surgical treatment consists of lateral canthotomy and inferior cantholysis. The diuretics acetazolamide and mannitol might be useful in medical management as well. Intraocular pressure should be monitored before and after treatment.
The most classic (though rare) orbital fracture seen in the pediatric population is the trapdoor fracture ( Fig. 97-3 ). This is a greenstick fracture in which a bone fragment is displaced into the sinus but is attached by a hinge of bone and rebounds toward its premorbid position. The hinge is usually located on the ethmoidal side of the orbital floor. If the fracture segment springs back into its normal anatomic position, any prolapsed orbital contents can become entrapped on the maxillary sinus side of the orbital floor. Of all orbit fractures, these might not exhibit overt signs of trauma, the so-called white-eyed blow-out. In either event, ocular muscle entrapment is an urgent matter that requires surgery as soon as possible to avoid ischemic necrosis of the entrapped muscle. When entrapment has been ruled out, orbital floor repair of large defects can be delayed 7 to 10 days to allow resolution of edema. Once ready for definitive treatment, the orbital floor can be approached in a number of ways; the retroseptal transconjunctival approach is advocated by the authors whenever the injury allows. This approach, when combined with lateral canthotomy or transcaruncular extension, provides access to nearly the entire orbital surface area. Exploration enables the surgeon to free entrapped tissue from under the trapdoor or through the continuity defect and either reduce it again or reconstruct it. Endoscopy has been reported as a means of evaluating and even treating orbital floor fractures as well. An endoscope is introduced through the maxillary sinus and the sinus is explored. The orbital floor is then approached and repaired via the anterior maxillary antrostomy. This enables treatment of the fracture without the esthetic concerns associated with other approaches. It also might afford a better approach to the posterior ledge. In cases of trapdoor fracture, once the orbital floor is reduced, no further treatment is indicated. This technique might be of limited value in some pediatric patients because of the limited size of the maxillary antrum or the position of unerupted teeth with respect to the planned antrostomy site.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


