Odontogenic Cysts and Tumors
Odontogenic Cysts
A periapical abscess forms when inflammatory cells accumulate at the apex of a non-vital tooth. Frequently, the source of the infection is obvious and is associated with a carious lesion or is the result of a previous injury to the tooth and pulpal tissue. When purulent material accumulates at the apex of the tooth, the tooth and the surrounding tissues become tender to palpation and percussion. If the inflammation is contained within the associated bone, an epithelium-lined cyst may form. A periapical cyst consists of a lumen with cellular debris and inflammatory cells. Radiographically, a periapical cyst looks similar to a periapical abscess. There is loss of lamina dura along the associated tooth root and a round, well-circumscribed radiolucency at the tooth apex. Treatment requires removal of the source of the infection (i.e., carious tooth) and débridement of the periapical cyst. If there is an associated infection, incision and drainage of associated spaces with systemic antibiotic treatment may be necessary.
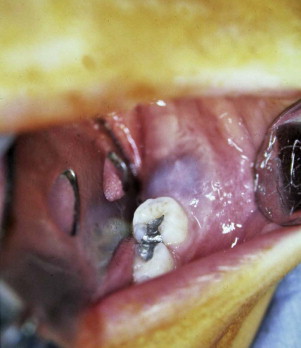
An eruption cyst results from expansion of the mucosa overlying the alveolar ridge above an erupting tooth ( Fig. 92-1 ). This lesion is often blue in color and compressible and may bleed on palpation. There is no associated distinct radiolucency, although soft tissue thickening can be visualized radiographically above the erupting tooth. Generally, no treatment is necessary because the tooth will erupt and the cyst will resolve spontaneously. However, if the cyst becomes large, removal of a portion of the overlying gingiva may be necessary to assist with tooth eruption.
A dentigerous or follicular cyst is the most common type of developmental cyst of the jaws. It develops from proliferation of the enamel organ remnant and grows in size as a result of increased osmotic pressure within the cyst lumen, which causes expansion and bone resorption. The cyst is most commonly associated with impacted third molars and maxillary canines and is frequently attached to the tooth at the cemento-enamel junction. It is usually asymptomatic and often discovered when assessing delayed eruption of a tooth but can sometimes become very large and cause cortical bone expansion and perforation. Radiographically, a dentigerous cyst is a well-defined, unilocular or occasionally multilocular radiolucency associated with the crown of an unerupted tooth. Treatment consists of removal of the associated tooth and enucleation of the cyst. However, if the lesion is associated with an unerupted permanent tooth or it affects a large portion of the jaw, decompression and irrigation allow the cyst to shrink and the teeth to erupt.
The World Health Organization has designated the odontogenic keratocyst (OKC) a type of keratocystic odontogenic tumor (KCOT). This lesion typically arises from cell rests of the dental lamina of an unerupted tooth. Radiographically, these are well-circumscribed radiolucent lesions that can be multilocular. The histopathology is characterized by (1) a well-defined basal layer with palisading cuboidal or columnar cells, (2) a keratinizing luminal surface that is mostly parakeratin but may be orthokeratin or a mixture of both, (3) an epithelial lining without an inflammatory infiltrate, and (4) a lumen full of keratinaceous debris.
Treatment depends on the size and location of the lesion. When the cyst is small, enucleation with curettage and close radiographic follow-up may be adequate. However, because of the high rate of local recurrence, ranging from 25% to 60%, some advocate peripheral ostectomy, application of Carnoy solution, or liquid nitrogen cryotherapy following curettage. The goal of these adjunctive therapies is to decrease the recurrence rate by eradication of daughter cysts or residual tumor cells in the superficial layers of the bony cavity.
When the lesion is large or there is concern that vital structures (e.g., nerves) may be injured during enucleation, cyst decompression plus irrigation is another option for treatment. After removal of a portion of the cyst wall, an irrigation port is placed into the cyst for twice-daily irrigation with 0.12% chlorhexidine gluconate solution. Depending on the cyst’s size, up to 24 months may be needed for the cyst to shrink. A residual cystectomy and peripheral ostectomy are usually required at the end of treatment. August and colleagues found that epithelial dedifferentiation and loss of cytokeratin-10 production occurs with this therapy and may be associated with lower rates of recurrence.
Nevoid basal cell carcinoma syndrome (NBCCS) is an autosomal dominant or spontaneous disorder characterized by multiple cutaneous basal cell carcinomas, odontogenic keratocysts, skeletal anomalies, and facial dysmorphology. Causative mutations for NBCCS occur in the PTCH1 gene on chromosome 9q22.3-q31, which encodes the principal receptor for the hedgehog signaling pathway. In the setting of this syndrome, the cysts are more aggressive and the recurrence rate after treatment has been reported to be as high as 82%.
Buccal bifurcation cysts develop along the buccal surface of mandibular molars where the roots bifurcate. The proposed cause of this cyst is extension of enamel onto the roots, which results in loss of periodontal attachment along the buccal root surface and extending to the root bifurcation. Radiographically, this cyst is a well-defined radiolucency in the furcation. Enucleation with periodontal scaling and root planing is the recommended treatment without tooth extraction.
Odontogenic Tumors
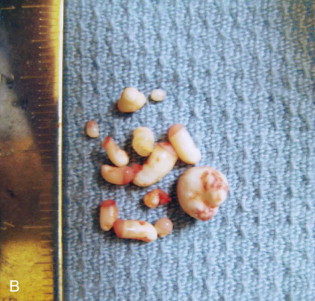
The most common odontogenic tumor is an odontoma . It arises from the odontogenic epithelium and mesenchyme that produce enamel and dentin. These tumors are usually asymptomatic, slow growing, and often are found incidentally during a routine radiographic examination. The radiographic appearance is almost always diagnostic, with the lesions consisting of densely opaque masses of varying size surrounded by a radiolucent line ( Fig. 92-2, A ). These tumors do not typically destroy surrounding bone or resorb adjacent tooth roots. A complex odontoma forms an amorphous calcified mass, and a compound odontoma is made up of multiple small tooth-like structures. Surgical excision is curative and recurrence is rare ( Fig. 92-2, B ).

An ameloblastic fibroma is a mixed tumor of epithelial and mesenchymal origin. The majority (about 80%) of these lesions occur in the posterior mandible, followed by the posterior maxilla; they rarely occur in the anterior region. These tumors are often asymptomatic and they can be associated with an unerupted tooth or may displace developing teeth. Radiographically, they appear as a well-defined unilocular or multilocular radiolucency with a smooth, well-defined margin or sclerotic rim. Histologically, the tumor is composed of mesenchymal tissue resembling primitive dental papilla. Throughout the tumor are long and narrow cords or small discrete islands of odontogenic epithelium that are typically two cells wide and resemble the developing enamel organ. Because this tumor has the potential for recurrence (10% to 20%) and malignant transformation, aggressive curettage or en bloc resection is recommended.
An ameloblastic fibro-odontoma resembles an ameloblastic fibroma, but it also contains enamel and dentin. Like an ameloblastic fibroma, it usually occurs in the posterior mandible. Radiographically, it is a well-circumscribed, unilocular mixed radiolucent/radiopaque lesion. It does not typically resorb surrounding bone or adjacent roots. Histologically, this tumor contains varying amounts of dentin-like material, enamel matrix, and even rudimentary tooth buds. This lesion separates from the bone easily, and enucleation plus curettage is curative with rare recurrence.
Non-Odontogenic Cysts and Tumors
Non-Odontogenic Cysts
A gingival cyst of the newborn is a superficial lesion located on the alveolar ridge in infants that arises from remnants of the dental lamina. It is usually smaller than 2 mm and more commonly located on the maxillary alveolus. These cysts are filled with keratin and usually disappear once they rupture.
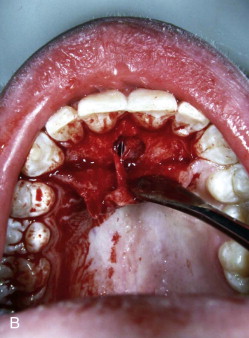
A nasopalatine duct or incisive canal cyst is the most common non-odontogenic cyst of the oral cavity and occurs in 1% of the population. During embryonic development, the nasopalatine duct connects the oral and nasal cavities. As the palatal processes elevate and fuse in the midline, epithelium that remains in the oral cavity forms this cyst. It appears as a compressible blue swelling on the palatal aspect of the maxillary central incisors ( Fig. 92-3, A ). Radiographically, it is a unilocular, heart-shaped radiolucency that rarely causes root resorption. In an asymptomatic patient, it may be difficult to distinguish between a large incisive foramen and a small nasopalatine duct cyst. If the radiolucency is smaller than 6 mm, it is generally considered a normal foramen. This lesion is treated successfully by reflection of a palatal flap and enucleation, with rare recurrence ( Fig. 92-3, B ). The nasopalatine nerve should be protected to decrease the chance for paresthesia of the anterior palate.

A traumatic bone cyst or simple bone cyst is an asymptomatic well-circumscribed radiolucency that commonly occurs in the mandible. These lesions are often found on a screening panoramic radiograph before the initiation of orthodontic treatment ( Fig. 92-4 ). Although the etiology and pathogenesis are not known, many patients have a history of trauma to the area. The diagnosis is made at the time of biopsy when an empty cavity is entered and no epithelial lining is found. Curettage of the empty cavity provides material for histologic examination and may promote bleeding and callus formation.

An aneurysmal bone cyst is similar to a simple bone cyst in that it is not a true cyst with an epithelial lining. The cause of an aneurysmal bone cyst may be a traumatic lesion, vascular malformation, or a neoplasm that disrupts the vasculature of the bone and results in a rapidly enlarging, blood-filled, anomalous vascular condition. Although it can be found in virtually any bone in the body, when it involves the craniofacial complex, approximately 40% are in the mandible and 25% are in the maxilla. In approximately a third of patients, a contiguous, simultaneously occurring bone lesion such as non-ossifying fibroma, chondroblastoma, giant cell tumor, or fibrous dysplasia is present, in which case it is known as ABC-“plus.” Radiographically, the lesion has irregular margins, displaces teeth, and can be unilocular or multilocular. Histologically, there is a fibrous connective tissue stroma with multiple multinucleated giant cells and sinusoidal blood spaces that are lined by fibroblasts and macrophages. Treatment consists of enucleation and curettage. Bleeding can be vigorous until the entire lesion is removed. Recurrence may be related to the biologic behavior of an associated lesion and may require more aggressive treatment dictated by the associated lesion rather than by the cyst.
Non-Odontogenic Tumors
Congenital epulis of the newborn is a sessile, pink, smooth lesion found on the maxillary alveolar ridge of newborns ( Fig. 92-5 ). It occurs more often in females than in males with a prevalence of 8 : 1. Histologically, the lesion has dense sheets of granular cells in the connective tissue. They are rarely large enough to interfere with feeding, sucking, or breathing but require excision because they do not regress.

A melanotic neuroectodermal tumor of infancy is a benign neoplasm of neural crest origin. It has a non-ulcerated, sessile, lobulated appearance with blue or black pigmentation secondary to melanin production by the tumor cells. It has a sudden onset, rapid growth, and a tendency to displace teeth. Radiographically, this tumor may appear as an ill-defined radiolucency with tooth buds floating in space. Histologically, it is characterized by two types of melanin-producing tumor cells in a connective tissue stroma. These cells are reactive for cytokeratin and melanoma-associated antigen (HMB-45). Because of its locally aggressive behavior, this tumor is treated by wide surgical excision with a 5-mm margin.
A myofibroma is a solitary, benign proliferation of myofibroblasts that can occur at any age. This lesion is found in soft tissue or bone with a predilection for the head and neck, particularly the mandible. Histologically, it is composed of nodules and fascicles of spindled cells with elongated, tapered, or blunt nuclei and interspersed collagen fibers. Although it can have aggressive clinical features such as rapid growth, a negative desmin stain rules out malignancy. If adjacent bony structures are involved, excision is recommended and enucleation plus curettage is curative for smaller lesions. Recurrence is rare.
Fibrous dysplasia is a benign, progressive condition in which an abnormal increase in the activity of bone protein (G protein) takes place as a result of hormonal changes such as the onset of puberty or pregnancy. Instead of normal bone, immature woven bone within a stroma of abnormal fibrous connective tissue forms and causes expansion and visible deformities. In the majority of patients, the lesions are localized in only one bone (monostotic fibrous dysplasia), whereas others have them in many bones (polyostotic fibrous dysplasia). In about 3% of patients, the condition occurs as a part of the McCune-Albright syndrome, which is caused by a mutation in the GNAS gene. Affected patients also have café-au-lait spots, pituitary adenomas, and hormonal abnormalities. Radiographically, fibrous dysplasia has a mixed radiolucent and radiopaque “ground-glass” appearance with expansion of associated bone and displacement of adjacent structures. Histologically, it has an abnormal collagenous matrix surrounding immature bone with irregular distribution and size, also known as “Chinese characters.” Treatment depends on each lesion’s biologic behavior and includes contour reduction for esthetics, en bloc resection for functional problems, or decompression of adjacent vital structures.
Cherubism is an autosomal dominant disorder with mutations in the gene SH3BP2 , which has been mapped to chromosome 4p16.3.3, but it can also appear as a part of genetic disorders such as Noonan syndrome, fragile X syndrome, and neurofibromatosis type 1. It is characterized by symmetric enlargement of the mandible, maxilla, or both, which causes rounding of the face with upturned eyes and visible sclera ( Fig. 92-6, A ), premature loss of primary teeth and impaction of permanent teeth. Though usually painless and self-limited, replacement of bone with multilocular cysts composed of fibrotic stromal cells and osteoclast-like cells may cause severe mandibular and maxillary overgrowth with respiratory, vision, speech, and swallowing problem. In adolescence the lesions progress slowly, and in late teens or early twenties the lesions regress and are replaced with normal bone. Radiographic manifestations in the mandible or maxilla consist of bilateral extensive, well-defined multilocular areas of diminished density with few irregular bony septa ( Fig. 92-6, B ). Histologically, the lesions contain numerous multinuclear giant cells in a loose fibrous stroma and eosinophilic cuffing with an increase in osteoid and newly formed bone matrix in the periphery. Because cherubism is expected to regress spontaneously, management consists of longitudinal observation with recontouring for esthetics once the disease becomes quiescent. Surgical intervention is indicated only if functional problems develop.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


