Treatment of mandibular fractures in pediatric patients is a challenging, yet rewarding endeavor. Because pediatric patients are experiencing active facial growth and dental development, special considerations must be taken. These complexities require an emphasis on proper planning and conservative treatment. Fundamentally, understanding of complex facial injuries has evolved through experience, both good and bad, with adult patients. Over time, various techniques, such as rigid fixation, were introduced into the pediatric population as well. However, one must carefully consider that children are not simply “small adults” and that the application of adult-type treatment can be inappropriate in many circumstances. Furthermore, evolving methods and materials that are impractical for use in adult patients may be better suited for use in the pediatric population.
Etiopathogenesis/Causative Factors
For a number of reasons, facial fractures have a lower incidence in children than in adults. For the most part, children reside in a very protective social environment. In the early years of life, parental supervision and a child-friendly environment mitigate the likelihood of serious injury. Although falls during these years are common, their low center of gravity ensures that little harmful force is generated that might cause injury. As children age, they are granted more freedom from the watchful eyes of their parents and begin to engage in activities, such as school and athletics, that increase the risk for injuries.
A number of studies have been conducted over the years to investigate the cause of mandibular fractures in the pediatric population. The Imahara study undertook an extensive review of the National Trauma Data Bank to analyze the incidence and etiology of facial fractures in pediatric patients ( Fig. 96-1 ). The National Trauma Data Bank contains information obtained from more than 600 U.S. trauma centers. This study analyzed 277,008 patients 0 to 18 years of age admitted during the years 2001 to 2005. Of these patients, 12,739 (4.6%) sustained facial fractures. Males were affected about twice as frequently as females. Fractures were progressively more common as patients aged, with a 2.4% incidence in toddlers and infants and increasing to a 6.9% incidence in teens aged 15 to 18 years.
The most common cause of facial fractures in this cohort was motor vehicle accidents (55.1%), followed by assaults (14.5%) and falls (8.6%). Although motor vehicle accidents were the number one cause of facial fractures in all age groups, falls were more common than violence in children aged 0 to 9 years and bicycle accidents were more common than violence in children 5 to 14 years of age. Indeed violence, as a mechanism of injury, was proportionally most common in the 0- to 1-year and 15- to 18-year age groups.
One particular source of injury that any oral and maxillofacial surgeon should always be aware of is child abuse. By its very nature, child abuse is a traumatic act with consequences for the child lingering far beyond healing of the affected soft tissue and bone. Unfortunately, most epidemiologic surveys of physical abuse in children show that the abuser is often an immediate family member. Head, neck, and facial injuries account for more than a third of physical abuse–related trauma. Injuries such as burns, lacerations, punctures, and fractures are all seen in abuse cases. Maxillofacial trauma surgeons who care for children should always keep the possibility of child abuse in mind when the history and clinical evaluation of an injury are not consistent. In addition, the discovery of multiple documented injuries at various stages of healing is a very concerning finding. Health care providers are mandated by law to report suspected child abuse in all 50 states.
Diagnostic Studies
Although there is no substitute for a thorough history and physical examination, modern imaging has provided significant assistance in the detection and treatment-planning stage of mandibular fractures, both in adults and children. Historically, a mandible series consisting of lateral oblique, posteroanterior, and Towne views were obtained to assess mandibular trauma. Later, panoramic radiographs were added by many centers because they were found to have sensitivity and specificity superior to that of the traditional mandible series. Even though the panoramic radiograph is still widely used because of its low cost and widespread availability to maxillofacial surgeons, computed tomography (CT) has replaced plain film radiography as the “gold standard” for the detection of facial trauma.
In a prospective study, confirmed by surgical exploration, Wilson and colleagues found helical CT to have a sensitivity of 100% versus a sensitivity of 86% for panoramic radiography in the detection of mandible fractures. Furthermore, Chacon and associates found the accuracy, sensitivity, and specificity of CT to be superior to that of panoramic radiography for the detection of condylar fractures in a pediatric population.
In addition to improved sensitivity, CT offers other advantages over panoramic radiography as well. Because CT is performed in the supine position, it is ideal when imaging a polytrauma patient who cannot be placed upright for panoramic radiography. Furthermore, this positioning facilitates the use of sedation, which is sometimes necessary in the pediatric population to acquire adequate imaging.
Diagnostic Studies
Although there is no substitute for a thorough history and physical examination, modern imaging has provided significant assistance in the detection and treatment-planning stage of mandibular fractures, both in adults and children. Historically, a mandible series consisting of lateral oblique, posteroanterior, and Towne views were obtained to assess mandibular trauma. Later, panoramic radiographs were added by many centers because they were found to have sensitivity and specificity superior to that of the traditional mandible series. Even though the panoramic radiograph is still widely used because of its low cost and widespread availability to maxillofacial surgeons, computed tomography (CT) has replaced plain film radiography as the “gold standard” for the detection of facial trauma.
In a prospective study, confirmed by surgical exploration, Wilson and colleagues found helical CT to have a sensitivity of 100% versus a sensitivity of 86% for panoramic radiography in the detection of mandible fractures. Furthermore, Chacon and associates found the accuracy, sensitivity, and specificity of CT to be superior to that of panoramic radiography for the detection of condylar fractures in a pediatric population.
In addition to improved sensitivity, CT offers other advantages over panoramic radiography as well. Because CT is performed in the supine position, it is ideal when imaging a polytrauma patient who cannot be placed upright for panoramic radiography. Furthermore, this positioning facilitates the use of sedation, which is sometimes necessary in the pediatric population to acquire adequate imaging.
Pathologic Anatomy
Critical examination of the stages of gross anatomic craniofacial development leads to several particular issues that have an impact on both the epidemiology and management of pediatric mandibular fractures. First, during infancy and early childhood, rapid brain growth causes a significant increase in head circumference. Head circumference attains greater than 90% of its adult size between 3 and 5 years of age. In addition, the orbits also reach skeletal maturity early in life (5 to 7 years of age). This provides the characteristic appearance of a very prominent forehead and orbits seen in infancy and early childhood. The later-maturing lower facial skeleton remains relatively protected behind these prominent facial features during this time frame. Consequently, the mid-face and orbits are relatively more prone to injury in early childhood. The bone itself during the early years of development has very high osteogenic potential and is characterized by thick medullary space and thin bony cortices, which results in the bone having a greater likelihood of greenstick fracture. The teeth in the primary dentition have particularly short, bulbous crowns that can make it difficult to achieve stable maxillomandibular fixation (MMF) during fracture reduction and stabilization with traditional techniques.
Development of the craniofacial skeleton during the later childhood years into the mixed-dentition period also yields further insight. During this time the lower two thirds of the face becomes more prominent as a result of forward and downward growth of the face, thus exposing these bones to more injuries. As per the functional matrix theory espoused by Moss and now widely accepted, facial bone growth is guided by the functional requirements of the overlying soft tissue envelope. Accordingly, the mandibular body is lengthened by deposition of bone at the posterior ramus and resorption of bone at the anterior ramus. Downward mandibular growth occurs as the result of endochondral replacement at the mandibular condyles. Skeletal maturity of the maxilla and mandible is attained by approximately 14 to 16 years of age in females and 16 to 18 years of age in males.
Early childhood is also characterized by development of the permanent tooth buds, which occupy space in the maxilla and mandible. These unerupted teeth create areas of structural weakness in the bone with a greater probability of sustaining a fracture through them. Furthermore, they must be taken into account when attempting open reduction and internal fixation. In addition, eruption of the permanent teeth in conjunction with loose, exfoliating primary teeth make maxillomandibular wiring and thus fracture reduction and stabilization more difficult. The permanent teeth erupt in a predictable sequence starting with the mandibular central incisors and first molars around 6 years of age. The maxillary incisors and mandibular lateral incisors erupt over the next 2 years or so. Finally, between the ages of 9 and 12, the canines and premolars erupt, followed by the second molars. In most cases the mandibular teeth erupt before their maxillary counterparts, and the teeth erupt from the midline posteriorly with the notable exception of the maxillary first premolar, which often erupts before the maxillary canine. As the permanent dentition becomes fully erupted at about 12 years of age (with the exception of the third molars) and growth continues through the early teenage years, the craniofacial skeleton becomes more adult-like in its form, thereby allowing treatment consistent with that used in adults.
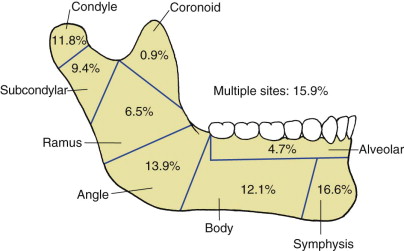
Many times, treatment of pediatric mandibular fractures is dictated by the pattern of injury. In descending order, the most common fracture sites in 4169 patients aged 0 to 18 years with mandibular fractures were the symphysis (16.6%), multiple sites (15.9%), angle (13.9%), body (12.1%), condyle (11.8%), subcondyle (9.4%), ramus (6.5%), alveolus (4.7%), and coronoid (0.9%). When considering these findings, one may group condylar and subcondylar fractures together, which will probably be treated identically, and note that one or the other accounted for more than 20% of the mandibular fractures in that cohort (especially given the propensity for a condylar component in patients with fractures at multiple sites). Similar results have been reported in studies of a smaller scale as well.
Treatment/Reconstructive Goals
The goals of treatment for all patients with mandibular fractures are a return to pre-injury function and appearance. This requires attention to facial symmetry and dental occlusion. Concerns specific to pediatric fractures are the effects of the injury or the treatment on subsequent facial growth and dental development. Finally, whenever possible, patients and surgeons alike prefer to minimize morbidity by shortening the course of treatment.
Pediatric mandibular fractures require thoughtful consideration to avoid further injury to the developing dentition and significant growth disturbance. Most are quite amenable to closed reduction with MMF or the use of splints with skeletal fixation (or both). With the rapid healing and remodeling characteristic of growing pediatric patients, even significant alterations in occlusion and discrepancies in alignment are resolved rapidly. Indications for the use of rigid fixation are not common but do exist. Infants (<1 year of age) with mandibular fractures should be treated by observation. Diet modification is not usually necessary in this age group, and most of these patients will heal in due course with expectant management alone ( Fig. 96-2 ).

Symphyseal and Parasymphyseal Mandibular Fractures
For anterior mandibular fractures, closed treatment is usually preferred for a number of reasons. First, these fractures, in isolation, are usually easily reduced, physiologic occlusion is reproduced, and the tremendous bone-healing potential of pediatric patients has an opportunity to take over. Furthermore, open reduction and internal fixation by traditional methods subject the patient to potential damage to unerupted teeth, as well as the possible need for a second surgery to remove the hardware. Finally, in growing patients, postoperative soft tissue scarring may lead to altered or restricted growth in the future.
When MMF alone may not be feasible, two alternative treatments exist. First, construction of a lingual splint from dental models is an elegant but time-consuming technique for reduction and fixation ( Fig. 96-3 ). This technique is completed as follows: (1) alginate dental impressions are taken of both the upper and lower arches, but good-quality impressions may not easily be obtained without significant cooperation from the injured child, and it is therefore sometimes necessary to use an additional anesthetic to take the impressions; (2) stone models are created with the impressions; (3) model surgery is performed on the mandibular model to recreate the pre-injury occlusion; and (4) a lingual acrylic splint is fabricated with holes placed interdentally to hold the splint in place. Once construction of the splint is complete, the patient’s mandible is manually reduced and the lingual splint is wired into place. In addition, circum-mandibular wires are sometimes required to further secure the splint. This type of fixation allows anatomic stabilization of the fracture while permitting movement of the mandible, which encourages rehabilitation of condylar fractures, if present. It also avoids the need for an incision and subperiosteal dissection, thus lessening soft tissue scarring.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


