In this article, five variations in orthognathic surgery procedures used to gain bone mass for implants are discussed: Le Fort I downgrafting, Le Fort I distraction, sub–Le Fort I interpositional sandwich grafting, segmental sandwich grafting, and the island osteoperiosteal flap approach.
The use of vascularized osteotomies, particularly in orthognathic surgery is well founded in the literature.
Edentulous total mandibular and maxillary osteotomies have also been reported. In the last 10 years, the use of segmental osteotomies done with edentulous segments, including sandwich osteotomies, alveolar split osteotomies, and island bone flap approaches, have begun to be studied both in the laboratory and clinically.
The advantage of alveolar osteotomies is that bone grafting is done interpositionally and crestal mucosal reflection is avoided, which generally leads to crestal bone stability, maintenance of gingival architecture, and a relatively uneventful recovery.
Although only 2 long-term clinical studies have been reported using sandwich osteotomy bone grafting for implants, it seems that volumetric stability of the bone around later-placed implants is nearly equal to that of the native bone when implants are placed after osteotomy healing has occurred.
In this article, 5 variations in orthognathic surgery procedures used to gain bone mass for implants are discussed: Le Fort I downgraft, Le Fort I distraction, the sub–Le Fort I interpositional sandwich graft, the segmental sandwich graft, and the island osteoperiosteal flap (i-flap) approach.
Le Fort I downgraft
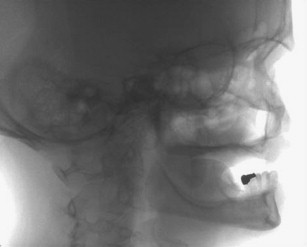
The use of iliac bone grafting for the Le Fort I downgraft is used to gain not only vertical dimension but also horizontal width. The sinus floor can also be grafted such that after healing, usually 6 months for graft consolidation and up to 6 months for implant healing, implants can be placed for a fixed restoration as shown in Figs. 1–10 .



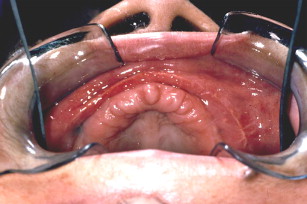

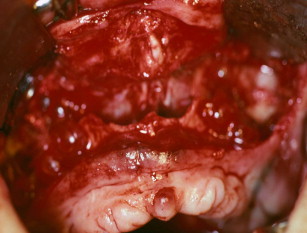


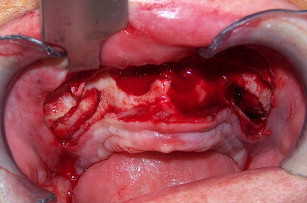
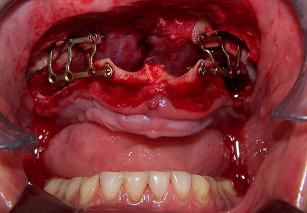
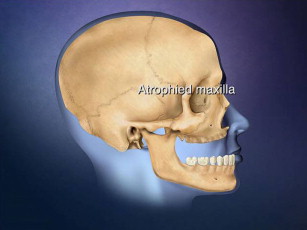
The technique involves making a vestibular incision and horizontal osteotomy cuts after elevation of the sinus membranes bilaterally through lateral window access (see Fig. 5 ). The pterygoid sutures and nasal septum are freed, and the maxilla is downfractured in a standard manner. However, because of severe atrophy, the maxilla often spontaneously fragments, so care must be taken when compared with younger dentate patients undergoing the Le Fort I procedure.
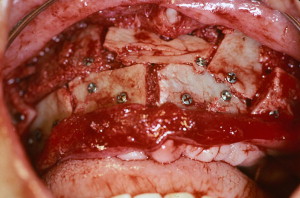
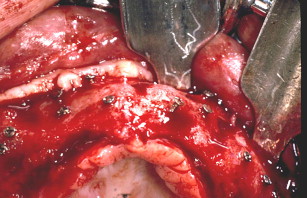
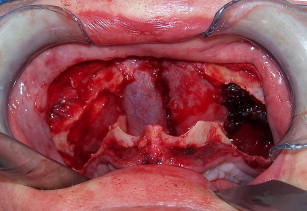
Following downfracture, the maxilla is mobilized forward using disimpaction forceps and then repositioned and bone plated in down and forward positions (see Fig. 6 ). A general rule of thumb is ten mm forward and ten mm downward. Fixation provides a very large interpositional graft zone for bone grafting. Grafting proceeds by first grafting the sinus floor with particulate marrow and then the anterior nasal floor, followed by block mortising and overgrafting the bone-plated regions to gain width (see Fig. 7 ). Consideration should be given to using resorbable bone plates, so that when implants are placed later, there will be no fixation screw interference. Once the graft is in place, which entails the combination of particulated bone marrow deep and corticocancellous blocks fixed with screws as overgraft, the wound is closed in 2 layers with slowly resorbing suture material. There should be no tension on the wound. Placement of a provisional denture at this time is a matter of judgment. When a denture is flangeless and borne only by the palate and crestal bone, and the confidence in the fixation is good, most often a denture can be placed early without risking wound dehiscence. On the other hand, when the Le Fort fixation is tenuous or the augmentation procedure opposes natural dentition, perhaps in a patient with bruxism, the use of a provisional denture should be curtailed.
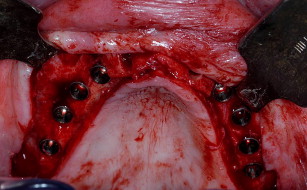
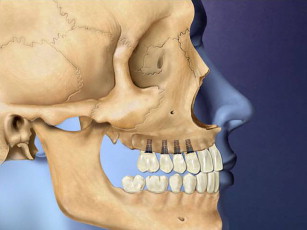
Six months later, an incision is made 3 to 4 mm palatal of the alveolar crest around the arch (see Fig. 8 ). The flap is developed and lateralized to gain fixed connective tissue buccally after implants are placed and abutments are connected (see Fig. 9 ). Often, because implants are placed at this time, the bone is still not completely consolidated, although there is great variation between patients. When implants are firmly torqued into place, a 1-stage protocol is used; if not, a staged method.
Following osseointegration, the final fixed denture prosthesis is inserted, which is needed to support the lip and make up for still remaining jaw bone deficiency despite bone graft augmentation (see Fig. 10 ).
The advantage of the Le Fort I downgraft is a greatly increased bone mass available for osseointegration; but the disadvantage is that alveolar height may not be achieved and the position of the maxilla is never ideal, often being 5 to 10 mm retropositioned, despite advancement. Also, these cases require a lot of bone graft material, often necessitating posterior hip harvest. Grafts can be expanded with allografts or alloplasts, but this may add additional risk for infection if the graft site becomes exposed. The greatest disadvantage is the need for a secondary harvest site, which is not always possible in the elderly or in patients with back and extremity osteoarthritis.
Therefore, the procedure may be relatively contraindicated in those older than 60 years, unless the patient is in excellent health, which suggests a great need to treat these not uncommonly found atrophic findings with an alternative method such as the use of bone morphogenetic protein 2 (BMP-2).
The use of BMP-2 for the Le Fort I procedure, however, is still in development. Figs. 11–21 show a case in which BMP-2 was placed following downward and forward maxillary repositioning using a Le Fort I osteotomy in which sinus elevation was done. Although a large amount of BMP-2 on collagen sponge (only) was used, the resultant bone mass gain with this technique was much less than that found with iliac graft reconstruction, although sufficient to place 10-mm implants (see Fig. 20 ). The bone quality was excellent and osseointegration uneventful.

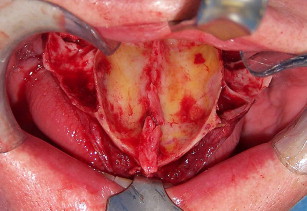
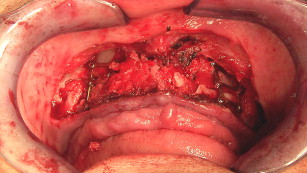

The grafting technique using BMP-2 is similar to iliac graft placement with the fragmented collagen sponges packed into the sinus floor first and then into the nasal floor, laterally around the osteotomy site, and into the wound closed primarily (see Fig. 18 ). When expansion of the graft is needed, the use of 20% to 30% demineralized freeze-dried bone allograft is advised. A large graft of BMP-2 requires 6 to 9 months for consolidation (see Fig. 19 ), although implants can be placed earlier into what feels like osteoid in a submerged approach. Exposure of implants is done with a palatal crestal bias to gain fixed connective tissue, and then the case may be restored with a fixed denture prosthesis.
Once again, the use of BMP-2 does not generally create an ideal reposition of the maxilla but does gain sufficient bone mass for dental implantation (see Fig. 21 ). The use of allograft as an expander has recently been shown to preserve the volume of the BMP-2 graft and should be considered in large graft sites.
Le Fort I distraction
When there is adequate alveolar width for implants but the edentulous maxilla is in a retrognathic position, the maxilla can be distracted forward and downward to optimize prosthetics for implants, which must be placed secondarily. The great advantage of the distraction procedure is prosthodontist-directed repositioning of the maxilla into optimal position for emergence profile implant restoration. The surgeon unfamiliar with this procedure must understand that the edentulous jaw can be placed within 1 mm of the desired anterior maxillary alveolar position. For a retrodisplaced maxilla, Le Fort I distraction is the most accurate of all grafting or distraction approaches for gaining an esthetic emergence of an implant restoration.
The technique has limited use because it is a special situation approach for treating young female edentulous patients who present with a modest retropositioned maxilla that needs to be brought down and forward to bring the alveolus into orthoalveolar form to optimize perioral and gingival esthetics.
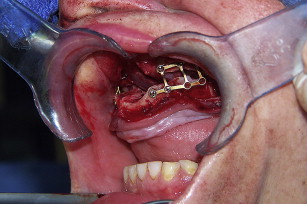
The technique ( Figs. 22–27 ) can be done in the office setting under intravenous anesthesia but is best done in the operating room. Medical models can be made from computerized axial tomography scan images and used to do mock Le Fort I surgery and distraction plate placement. The distraction plates are prebent and placed on the models to gain the appropriate vector for advancement, so they are ready for use during surgery.
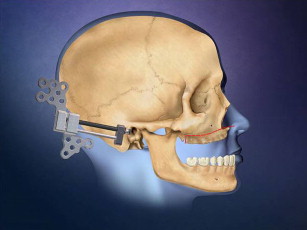
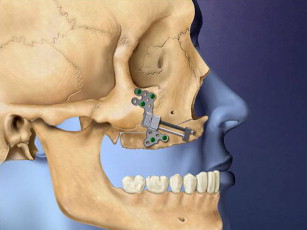
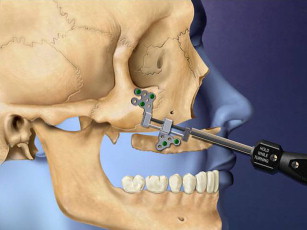

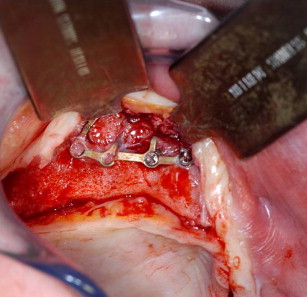
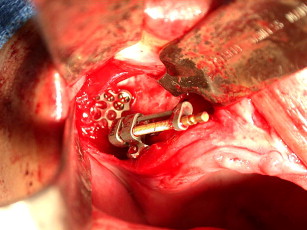
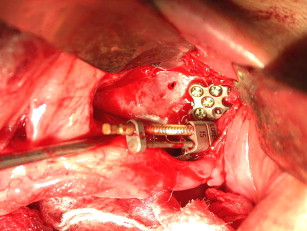
Figs. 28–38 show the Le Fort I distraction technique. A vestibular incision is made in a 35-year-old female patient (see Figs. 28 and 29 ), and sinus membranes are elevated bilaterally followed by horizontal osteotomy cuts (see Fig. 30 ). The pterygoid sutures and nasal septum were freed using osteotomes, and then the maxilla is minimally downfractured to allow for freedom of movement. In the operating room, the maxilla can be fully mobilized, although this is not always necessary for unimpeded distraction to proceed. The distraction plates were then fixed into place with downward and medial vectors (see Figs. 30 and 31 ), with the osteotomy site open about 2 mm (see Fig. 32 ). The sinus floor was grafted but not the osteotomy sites. The distraction proceeded over a 2-week period following a 1-week latency (see Figs. 33 and 34 ). The use of BMP-2 as graft material not only facilitates sinus floor augmentation but also augments distraction osteogenesis, which to a great extent is based biologically on mechanoreceptor-induced BMP-2 signaling.


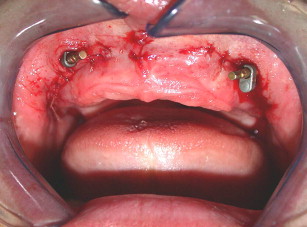






The maxilla had healed well 6 months later. The bone plates were removed and implants placed transgingivally (see Figs. 35 and 36 ). And then, the final restoration was done (see Figs. 37 and 38 ), which showed a natural gingival emergence that was stable at 3 years.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


