Endosseous implants have revolutionized dental prosthetic rehabilitation, providing a reliable, a stable, and an aesthetic option for dental reconstruction. Dental implants have similarly improved the functionality of reconstructions following cancer surgery. The use of dental implants in oral cancer reconstruction can be divided into 2 categories: (1), for retention of a prosthetic device, for example, palatal obturator, used as the primary means of maxillary reconstruction, and (2), for dental rehabilitation after bony reconstruction of the jaws. This article discusses these different uses of endosseous implants in patients with head and neck cancer.
Endosseous implants have revolutionized dental prosthetic rehabilitation, providing a reliable, stable, and aesthetic option for dental reconstruction. Dental implants have similarly improved the functionality of reconstructions following cancer surgery. The use of dental implants in oral cancer reconstruction can be divided into 2 categories. First, for retention of a prosthetic device, for example, palatal obturator, used as the primary means of maxillary reconstruction. Second, for dental rehabilitation after bony reconstruction of the jaws. This article discusses these different uses of endosseous implants in patients with head and neck cancer.
Implants for maxillary obturators
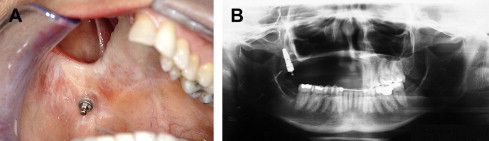
For more than a hundred years, use of the palatal obturator has been the principal mode of reconstruction of the maxilla after extirpative surgery and is still considered by many to be the gold standard in maxillary reconstruction. Depending on the nature of the defect (size, vertical extent of maxillary resection, degree of soft tissue loss, involvement of soft palate) and the status of the patient’s dentition, the conventional obturator can function quite well as a means of restoring the dentition and separating the oral and nasal cavities ( Fig. 1 ). However, many disadvantages of tissue- and tooth-borne devices are apparent.

In the partially dentate patient, the obturator is designed to function much like a removable partial denture, with support provided by the remaining palatal bone, the obturated cavity, and the remaining dentition. This situation may lead to unfavorable forces on the remaining dentition, compromising these teeth over time. In the edentulous patient, only the remaining hard palate, the maxillary alveolus, and the obturated cavity are available for support. In more extensive resections, there may be no maxillary bone present to provide obturator support, and therefore, very few options are available for conventional obturator use.
Similarly, retention of these prostheses can also be problematic. In the absence of the dentition, soft tissue retention at the interface of the buccal mucosa and the obturated cavity has been considered a primary retention principle in the fabrication of these devices. These devices have marginal levels of retention and are commonly a source of annoyance from constant irritation caused by the mobility of the prostheses. These factors also lead to a large bulk of material that can make the appliance difficult to handle and relatively heavy.
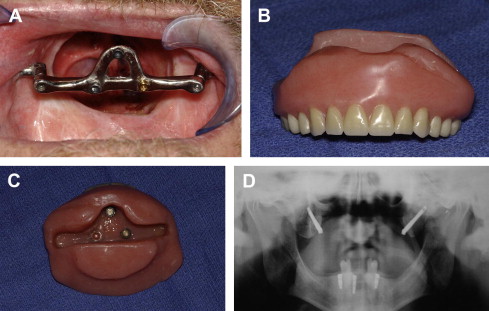
Endosseous and zygomatic implants can improve a patient’s ability to wear these obturators by improving prosthetic stability and retention. In the edentulous patient, use of multiple endosseous implants in the residual alveolar bone can provide a platform for the fabrication of a retention bar that supports the overlying obturator prosthesis. Depending on the size and location of the defect, the forces placed on these implants can be unfavorable and can lead to eventual implant loss in a fashion similar to obturators supported by natural teeth in the partially edentulous patient. Placement of endosseous implants into the remaining bone surrounding the maxillary defect (pterygoid plates, zygoma, residual maxilla) ( Fig. 2 ) has been advocated to avoid these unfavorable forces. However, these implants have poor osteointegration potential and are difficult to restore and maintain.
Although the zygomatic implant was initially intended for aiding in the prosthetic rehabilitation of the atrophic maxillary alveolus, it has been adapted often in combination with traditional endosseous implants for maxillary obturator support and retention. Some of the limitations of implant placement in the bone surrounding the maxillectomy defect are mitigated by the use of these specialized implants, in that they are able to engage more distant bone. Very little literature exists on the use of zygomatic implants for this indication, and little is known about the long-term implications of these devices in maxillary reconstruction, but their use seems to be a reliable and effective adjunct to traditional implants for prosthesis support ( Fig. 3 ). In a series by Schmidt and colleagues, 21% of zygomatic implants failed at the time of stage II implant surgery. This relatively high implant failure rate was attributed to the use of radiation either before or after implant placement. Another case series reporting on a mixed group of patients receiving zygomatic implants for maxillectomies as well as traumatic injuries, severely atrophic maxillas, cleft lip, and cleft palate reported an overall failure rate of 5.9%.
Implants in reconstructed jaws
The reconstructive surgeon has several options for bony reconstruction of the maxilla or mandible. The specifics of different bone graft harvest sites or free flap donor sites are beyond the scope of this article, but the characteristics of some of these options as they pertain to implant reconstructions are worthy of mention. Regardless of the technique used for jaw reconstruction, the surgeon should consider the goal of full dental rehabilitation as the ultimate end point of the reconstruction.
Advancements in reconstructive surgery have taken cancer reconstruction from a high-risk afterthought of cancer treatment to a reliable and expected component of cancer surgery. The use of regional flaps and free tissue transfer has allowed for more complex reconstructions and improved functional outcomes. Similarly, the necessity for dental reconstruction has followed with these advancements, and in many cases, it is no longer satisfactory to have a successful cancer ablation and an edentulous reconstructed jaw.
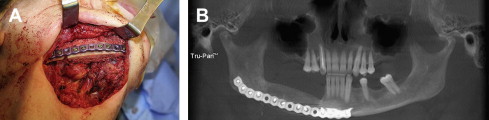
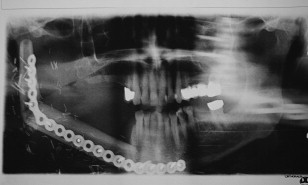
The time-honored gold standard in jaw reconstruction is the free iliac crest bone graft. Bone harvested from the anterior or posterior iliac crest is placed in a mandibular defect as a block or a corticocancellous graft, or a combination of the 2 ( Fig. 4 ). Because of the nonvascular nature of these grafts, this procedure is generally performed as a secondary operation many months after the initial cancer ablation to avoid the high incidence of graft loss and infection when performed primarily. This type of mandible reconstruction is most suited for relatively short defects of the lateral mandible that do not cross the midline and is a highly effective technique for reconstruction in benign tumor resections such as ameloblastomas. The usefulness of this type of reconstruction is somewhat decreased in cancer reconstruction because many patients require postoperative radiation treatment that can inhibit bone graft healing and consolidation. Preoperative and postoperative hyperbaric oxygen (HBO) therapy and the use of regional flaps to provide vascularized tissue to the area have been advocated by some investigators to improve the vascular quality of the wound bed and graft healing. Although useful in selected cases, the emergence of microvascular free tissue transfer has largely supplanted these techniques.
Composite microvascular tissue transfer has revolutionized cancer reconstruction, in that bone and soft tissue can be transferred from a distant site in the same operative encounter as the ablative surgery and, in most instances, from a single donor site. The literature is replete with various donor sites advocated for use in maxillary and mandibular reconstruction, including the ilium, fibula, scapula, radius, rib, and metatarsal. Each donor site has its own advantages and disadvantages, and an ideal replacement for maxillary or mandibular bone and intraoral soft tissue does not exist yet. However, of the donor sites currently available for jaw reconstruction, the ilium and fibula have emerged as the most desirable. Of these 2 sites, the fibula has numerous advantages over the ilium, with few drawbacks.
The iliac crest bone can be harvested as a bone-only, an osteocutaneous, or a myo-osteocutaneous (internal oblique) flap, based on the deep circumflex iliac artery (DCIA) and the accompanying deep circumflex iliac vein (DCIV). This flap’s greatest advantage is the bone volume available for transfer, which is more than suitable for implant placement. Although the volume of the bone is good, the length of the bone available is somewhat limited, and the volume of soft tissue that must be included with this flap can be bulky ( Fig. 5 ). The DCIA and DCIV provide a fair length of pedicle for mandible reconstruction, but their use in the maxilla usually requires vein grafts. Finally, harvesting of the DCIA flap requires disruption of the anterior abdominal wall and upper leg muscle attachments, leading to hernias and gait disturbances, respectively. Collectively, these drawbacks have somewhat overshadowed this flap’s significant bone volume advantage over the fibula and has affected its acceptance as a suitable donor site for jaw reconstruction. Accordingly, implantation into iliac crest grafts has not been reported much, and very little literature is available for review.

The fibula can also be harvested as a bone-only, an osteoseptocutaneous, or a myo-osteocutaneous flap (soleus or flexor hallucis longus). The fibula flap was introduced for use in mandible reconstruction in 1989 by Hidalgo and has been the first choice for jaw reconstruction for many reconstructive surgeons. The fibula flap is popular for several reasons, including the ease of harvest, ability to work in 2 teams, availability of a long bony segment for harvest, low morbidity, and good pedicle length and caliber of vessels. Its disadvantages are few, but critics have argued that the bone is of insufficient height, has an inflexible skin paddle, and has the possibility of potential vascular compromise to the foot.
Much of the criticism regarding the effectiveness of the fibula in mandible reconstruction is aimed at its lack of vertical height. On average, the fibula’s height is between 13 and 15 mm and is very close to that of an edentulous mandible ( Fig. 6 ), but the fibula certainly lacks the height of a dentate mandible ( Fig. 7 ). Various techniques to increase the fibula’s height have been proposed, such as distraction osteogenesis of the segments or “double barreling” of the fibula ( Fig. 8 ), but a relatively simple technique is to simply adapt the fibula to abut the native mandible in a slightly more superior position than the inferior border ( Fig. 9 ). Of course, a slight cosmetic deformity with a lack of bone at the inferior border may occur, but this deformity is generally minor and of little concern to most patients.


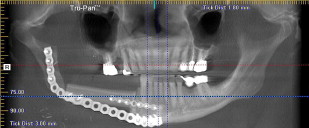
Presurgical planning with the restoring prosthodontist is mandatory before implant surgery. A surgical guide can be fabricated based on the prosthodontist’s estimation of the location of the reconstructed bone and his/her ideal locations for implant fixtures. In some cases, this guide may not be helpful because of inaccurate estimation of the bone location but can serve as a blueprint for the next-best implant location. Cone beam computed tomographic scans and implant planning software help mitigate these limitations in the planning phase.
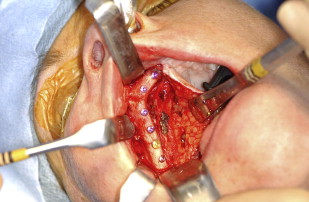
The actual implant placement procedure is no different from that in traditional implant surgery; however, a few principles should be followed. When accessing the implantation sites, if a skin paddle exists over the flap or graft, care should be exercised to preserve the perforator to the skin when designing the incision. Skin paddle revascularization from the surrounding mucosa is unpredictable at best, and at present, there is no way to determine if the skin paddle will survive without its native blood supply. In most mandibular reconstructions, these perforators emerge from the ligual aspect of the reconstructed mandible as is the case with the fibula osteoseptocutaneous flap, iliac crest osteocutaneous flap, and pectoralis major myocutaneous flaps placed before free bone grafting of the mandible. Therefore, the incision should be made at the skin-mucosa interface on the lateral or buccal aspect of the skin paddle. This incision allows lingual retraction of the skin paddle and provides access to the bone and fixation hardware. Some circumstances may require the perforators to emerge laterally to the mandible, so careful review of the operative report should be done before implant surgery.
Similar to mandibular reconstruction, if a fibula osteoseptocutaneous flap is used for maxillary reconstruction, often, the perforator to the skin emerges from the palatal aspect of the skin paddle. Again, the incision is made on the lateral aspect of the skin to preserve this blood supply and minimize the risk of devitalizing the skin ( Fig. 10 ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


