Fig. 17.1
Example of Class I, II, and III profiles
The clinical exam consists of an extraoral and intraoral evaluation. The extraoral evaluation includes an assessment of the patient’s temporomandibular joint (TMJ), including presence of popping, clicking, pain, or locking. In patients with TMJ pain, orthodontics should not be started until the pain is controlled. The effects of orthodontics on the TMJ are varied and not widely understood. Orthodontics is not a proper treatment for TMJ joint pain, generally. The muscles of mastication, opening, and closing should be palpated for the presence of myofascial pain. Range of motion should be evaluated for normalcy of maximum opening, protrusion, and excursive movements.
The intraoral evaluation begins with evaluating the health of the teeth and periodontium, as well as the level of oral hygiene. These can be categorized as poor, good, or excellent. Full periodontal probing should be done in all patients over the age of 18. Some orthodontists may also advocate periodontal probing of younger patients to screen for subgingival calculus, deep pockets, and aggressive periodontitis.
Molar classification is determined based on the relationship of the first molars, as originally described by Edward H. Angle (Angle 1899). Normal, Class I, relationship is defined as the mesiobuccal cusp tip of the maxillary first molar lining up with the buccal groove of the mandibular first molar. (Fig. 17.2) Class I relationship of the canine is defined as the cusp tip of the maxillary canine positioned directly interproximal between the mandibular canine and first premolar. (Fig. 17.3) Any deviation of the maxillary teeth anterior to the mandibular teeth is classified as Class II molar and/or canine. (Fig. 17.4 and 17.5) Posterior deviations are classified as Class III. (Fig. 17.6) The extent to which a patient is Class II or III is defined by the amount of cusps from the Class I position (¼, ½, full cusp, or more than a full cusp). Class II malocclusions are further classified into Division 1 (Fig. 17.4) or Division 2. Class II Division 2 malocclusions typically demonstrate retroclination of the upper central incisors, a deep overbite, and proclination of the upper lateral incisors. (Fig. 17.5) If Class II or III occlusion appears unilaterally with the opposing side being Class I, the occlusion would be defined as being a subdivision on that side. For example, a patient that is Class I on the right, but Class II, Division 1 on the left would be classified as Class II, Division 2, subdivision left.




Fig. 17.2
Examples of molar classification with arrows illustrating position of mesiobuccal cusp of maxillary first molar and buccal groove of the mandibular first molar. The relationship of these is used to determine the molar classification

Fig. 17.3
Class I occlusion – arrows delineating the mesiobuccal cusp tip of the maxillary first molar lining up with the buccal groove of the mandibular first molar

Fig. 17.4
Class II, Division 1 occlusion – arrows delineating the mesiobuccal cusp tip of the maxillary first molar ¾ of a cusp mesial to the buccal groove of the mandibular first molar

Fig. 17.5
Class II, Division 2 occlusion – arrows delineating the mesiobuccal cusp tip of the maxillary first molar ¾ of a cusp mesial to the buccal groove of the mandibular first molar. Note the lateral incisor overlapping the retroclined central incisor and deep bite, typical of this malocclusion

Fig. 17.6
Class III occlusion – arrows delineating the mesiobuccal cusp tip of the maxillary first molar a full cusp distal to the buccal groove of the mandibular first molar
Fig. 17.7
Example of a comprehensive records form
Overjet is measured, in millimeters, from the incisal edge of the maxillary incisor to the most labial point of the opposing mandibular incisor. A relationship where the maxillary incisors lie anterior to the mandibular teeth results in positive overjet. When the maxillary teeth are posterior to the mandibular incisors, the overjet is recorded as negative. Overbite is recorded as the measurement from the incisal edge of the maxillary incisor to the incisal edge of the opposing mandibular incisor. Teeth with overlap are recorded as having positive overbite, while those without are edge to edge or cases with space between the incisors there is negative overbite (i.e., open bite). The overall overjet and overbite should both be recorded based on the teeth with the worst relationship (Cangialosi et al. 2004). If the patient’s lower incisors are touching the palatal tissues, this is termed an impinging overbite and can sometimes result in loss of gingival tissue or palatal inflammation. The midlines of both the upper and the lower jaw should also be recorded in relationship to the face and to each other. Crossbites in the anterior and posterior should be noted. Posterior crossbites presenting with maxillary tooth completely buccal to the mandibular tooth is termed a Brodie crossbite.
Every patient should be evaluated for a slide or shift from centric relation (CR) into maximum intercuspation (MI). Slides are caused by interferences which prevent the patient from biting where the proper mandibular position is. Classification, overjet, crossbites, midlines, and several other relationships may be different in CR and should be recorded in both relationships. When orthodontic treatment begins, oftentimes the shift is eliminated, and the mandible settles in the CR position. For this reason, malocclusions should be treated to the assessment in CR.
17.1.2.2 Study Models
Stone or digital models are used to study the occlusal relationships from several angles and to generate a space analysis. In order to perform a space analysis, the widths of all of the teeth are measured and recorded. The arch length is recorded from mesial of one permanent first molar to the mesial of the contralateral molar. If the arch length is greater than the sum of the tooth widths of the second premolar to the contralateral second premolar, there is spacing. If it is smaller, there is crowding. In the mixed dentition, the lower permanent incisors can be used to predict the width of the canine and premolars. The Moyers and Tanaka-Johnston analyses are the most commonly used methods for this. The Moyers analysis provides a table with prediction values based on the cumulative width of the lower incisors. The Tanaka-Johnston analysis determines the width of the canine and premolars by calculating one-half of the sum of the mandibular incisors and adding 10.5 mm to determine the width of the mandibular teeth on one side and 11 mm for the maxillary teeth. Adding the predicted values to the incisors and comparing that to the arch length provides the amount of spacing or crowding that is expected.
The width of the teeth can also be used to determine if a tooth-size discrepancy exists. Based on Bolton’s tooth-size analysis (Bolton 1962), the ratio of the tooth widths, first molar to first molar, of the mandible to the maxilla, should ideally be 0.91. The mandible to maxilla ratio of canine to canine widths should be 0.77. Ratios greater than the norm indicate mandibular excess or maxillary deficiency. Less than the norm indicates maxillary excess or mandibular deficiency. If a tooth-size discrepancy goes undetected, there may be difficulty in finishing with a Class I molar and canine relationship.
In addition to the information obtained in the intraoral examination, models can provide a way to help treatment plan. The models can be moved in all planes of space to determine what treatment options may serve to correct the malocclusion. They can also be used to create tooth setups for treatment planning and presenting to the patient.
17.1.2.3 Photographs
The American Board of Orthodontics advocates the use of three extraoral photos consisting of:
-
Anterior view with relaxed lips
-
Anterior view with full smile
-
Profile view with the patient facing to the left with the ear exposed for proper orientation
In all of these photos glasses and distractors (such as large earrings) should be removed, and a solid colored background is used. Anterior photos allow one to evaluate the facial shape, harmony, and symmetry, as well as incisal show and buccal corridors.
Five intraoral photos constitute the standard for diagnosis. These include:
-
Occlusal photos of the maxillary and mandibular arches
-
Frontal and lateral views in maximum intercuspation
The use of cheek retractors, suction, or air should be used to eliminate surrounding soft tissue and saliva. If a slide from CR to MI is discovered in the intraoral examination, frontal and lateral photographs should be taken in CR as well. (Fig. 17.8)
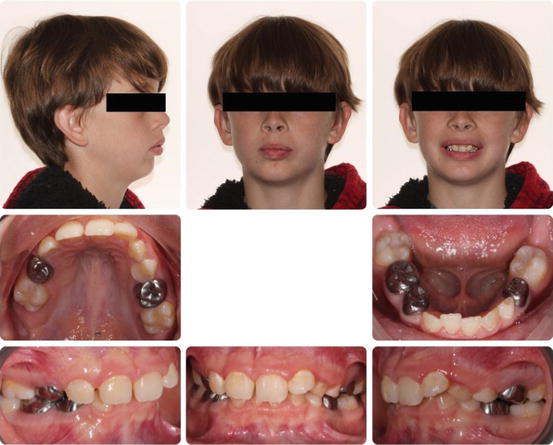
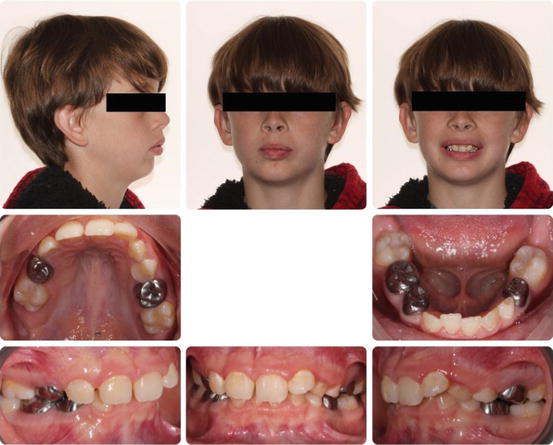
Fig. 17.8
Example of photo composite
17.1.2.4 Radiographs
Radiographs serve an important role in treatment planning. Most general dentists readily have access to panoramic radiographs. These serve to assess tooth eruption, development, root parallelism, and pathology. In patients that are 18 years old or older, vertical bitewings should be taken to assess bone levels around the teeth and to detect the presence of bone loss.
Lateral cephalometric radiographs help in the skeletal assessment (Steiner 1960). These radiographs are typically traced. (Fig. 17.9) A number of skeletal points are marked and serve as the basis for several linear and angular measurements. Some basic points for skeletal evaluation are:
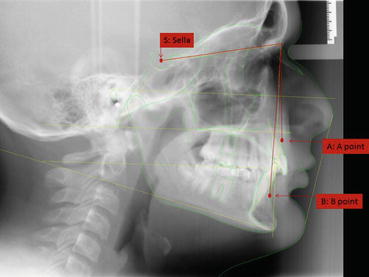
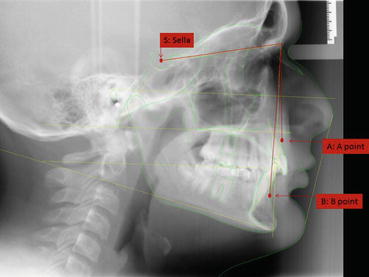
Fig. 17.9
Lateral cephalometric radiograph with key landmarks labeled
-
Sella (S): the middle of the sella turcica
-
Nasion (N): the most anterior point of the nasofrontal suture
-
A point (A): the deepest part of the concavity on the anterior of the maxilla
-
B point (B): the deepest part of the concavity of the anterior of the mandible
These points together form a number of lines and angle:
-
Sella-Nasion-A point (SNA): Indicates the anteroposterior position of the maxilla. The normal value for this angle in Caucasians is 82°.
-
Sella-Nasion-B point (SNB): Indicates the anteroposterior position of the mandible. The normal value for this angle in Caucasians is 80°.
-
A point-Nasion-B point (ANB): Indicates the anteroposterior relationship of the maxilla and mandible. The normal value for this angle in Caucasians is 2–4°. Values greater than this indicated a Class II skeletal relationship. Smaller values indicate a Class III relationship.
More advanced analysis of a lateral cephalometric radiograph can provide information about the anteroposterior position and angulation of the upper and lower incisors, vertical dimensions of the face, and growth tendencies.
More recently, the use of cone-beam computed tomography (CBCT) has become more popular in the field of orthodontics. (Fig. 17.10) Full or limited view CBCTs can be used when skeletal asymmetries, impacted teeth, or cleft lip and palate is suspected. CBCTs can also be used to extract digital models, panoramic, and lateral cephalometric radiographs. In cases where a CBCT is indicated, the radiation exposure to the patient should be considered to determine which combination of radiographs would keep it as low as possible in accordance with the as low as reasonably achievable (ALARA) principle for dentistry (ADA 2012).
Fig. 17.10
Use of cone beam computed tomography to locate upper right permanent canine and assess potential root resorption of the upper right lateral incisor
17.1.3 Creating the Orthodontic Problem List and Objectives
17.1.3.1 Ideal Soft Tissue, Skeletal, and Occlusal Features
Before determining a problem list or objectives, it is important for dental practitioners to recognize what ideal soft tissue, skeletal, and occlusal features are. Soft tissue profiles are ideally Class I with a 90° or slightly obtuse nasolabial angle. The upper and lower lip should have adequate support and lip curl. From the frontal perspective the face should be symmetric. When smiling, the upper and lower midlines should be on with the facial midline. Ideal tooth show is full maxillary incisor plus 1–2 mm of gingival show as previously discussed. Esthetically gingival margin heights should be at the proper heights in relationship to one another and symmetrical. The shape of the smile from canine to canine based on the incisal edges should follow the shape lower lip. In the vertical dimension, the facial thirds should be about equal. Skeletal ideals are based off of the lateral cephalometric radiograph. The ideal skeletal evaluation would reveal a Class I relationship of the maxilla and mandible in good anteroposterior relationship to the rest of the face. SNA, SNB, and ANB are used to determine this and are described above.
“Ideal” occlusion has been described by a number of authors. Angle was responsible for developing the first classification system for molar relationships as Class I, II, or III as described above. Andrews developed six occlusal features consistent in a series of “ideal” occlusions which has since been used to develop what is considered the norm for objectives (Andrews 1972). The first is molar relationship, similar to the Angle’s classification; Class I molar relationship is ideal. Other features of the ideal occlusion are proper mesiodistal and buccolingual tip of the crowns of the teeth, no rotations, no spacing, and a flat curve of Spee. The mesiodistal tip of teeth can be evaluated on a panoramic radiograph. The buccolingual tip, also known as torque, of the incisors is evaluated on a lateral cephalometric radiograph, while the torque of molars is evaluated on study models. Other ideal aspects of occlusion are 1–2 mm of overjet, 20 % overbite, lack of crossbites, no crowding, and Class I canine. Ideal functional aspects of occlusion are incisor guidance in protrusion and canine guidance in excursive movements. Some patients may require group function for guidance when the canines are worn down significantly. Contacts on all of the teeth should be even in maximum intercuspation, and no slide from CR to MI should exist.
17.1.3.2 Developing the Problem List
Based on the known ideal features and the information collected during the exam, a problem list is developed. This list can then be used in determining objectives, assessing the difficulty of a case, or in communicating information in a referral to an orthodontic specialist. The most important problem that should be included in the list is the patient’s chief complaint. Inability to address this in orthodontic treatment would result in an overall failure of treatment.
Ackerman and Proffit developed a system of categorizing problems into five main groups (Ackerman et al. 2007). The first is the dentofacial appearance, which includes symmetry, facial proportions, incisor display, lip support, and soft tissue profile. The second category includes the teeth and arch form including alignment, symmetry of the jaws, and spacing or crowding. The next three categories include the skeletal and dental problems in the transverse, anteroposterior (sagittal), and vertical planes of space. In the transverse problems include posterior crossbites, torque of the posterior dentition, and asymmetries of the maxilla and/ or mandible. In the sagittal plane, classification of the molar, canine, and skeleton are noted, as well as anterior crossbites and overjet. A slide or shift forward from CR to MI would also constitute a problem in the sagittal plane. Lastly, the dental deviations in the vertical category would include overbite which would result in a deep or open bite. Skeletally, vertical problems would include vertical maxillary excess or a steep or flat mandibular plane. Some traits in malocclusions may not be easily categorized. For example, open bites can have both skeletal and dental etiologies. Cases such as this and other skeletal issues are more complex and should be referred to the orthodontist for comprehensive orthodontic treatment. Some problems do not meet the qualifications for any of these categories. Such examples are periodontal health and maxillary frenum attachments.
When treating orthodontic cases, the Ackerman-Proffit analysis can be used to develop soft tissue, skeletal, and dental objectives. Objectives are then used to determine optimal treatment options for the patient. Every patient presents with a unique set of problems and diagnoses and therefore a unique treatment plan should be developed for every patient to properly treat them.
The five categories of the Ackerman-Proffit analysis are also useful in referring a patient to orthodontics. A list of concerns that the general dentist has in regard to the patient can be listed simply as:
- 1.
Soft tissue frontal and profile
- 2.
Arch form, space analysis, and symmetry
- 3.
Transverse dimension
- 4.
Anteroposterior dimension
- 5.
Vertical dimension
Use of this concise method helps streamline the referral process and alerts the orthodontist to the potential complexity of a case.
17.2 Orthodontic Treatment in the Primary and Mixed Dentition
17.2.1 Timing and Goals of Treatment
Malocclusions in younger patients can lead to functional issues, psychological problems, or dental disease, including increased susceptibility to caries, periodontal disease, and traumatic injury (Proffit et al. 2013). While many of these patients may benefit from orthodontic treatment, it is not an immediate need for all. Orthodontic treatment typically begins between the ages of 9 and 14, but some malocclusions can benefit from earlier treatment. The American Dental Association recommends that children visit the dentist by age one. In addition to maintaining regular dental care and oral hygiene, it is the responsibility of the general or pediatric dentist to monitor the child’s dental and craniofacial development during these critical years. If any abnormalities in the development of the dentition or craniofacial complex are noted, parents should be informed and a referral to an orthodontist should be made.
Distinguishing the complexity of orthodontic problems is a crucial skill for the dentist to attain (Proffit et al. 2013). Intervention at the appropriate time allows the practitioner the opportunity to guide jaw growth, lower the risk of trauma to protruded teeth, correct harmful oral habits, improve appearance and self-esteem, guide permanent teeth into a more favorable position, improve the way lips meet, and maintain or develop space for erupting teeth. The decision to treat a patient or refer to a specialist depends on the experience of the general dentist and the severity of the malocclusion. Unless earlier treatment is indicated, the American Association of Orthodontists recommends that a child has a complete orthodontic evaluation and/or referral no later than age 7 to determine treatment needs and timing (Suresh et al. 2015). Prior to this time, close monitoring of radiographs, eruption sequence, space analysis, and jaw relation should be integrated by the general or pediatric dentist from much earlier in life.
It is known that skeletal patterns and malocclusions are established in early childhood. Early treatment may consist of intraoral and extraoral appliances to exert the greatest control over dentoskeletal form and function. Proper orthodontic evaluations and treatment of children can prevent the development of more serious problems and may result in shorter or less complicated treatment at a later age. While the literature provides some conflicting evidence, there are some indications that some correctable dental discrepancies left untreated can turn into permanent skeletal discrepancies and even worsen. The rationale for early orthodontic treatment is to eliminate skeletal or dental disharmonies and enhance occlusal development to promote normal growth and development, improve function, and avoid psychosocial distress during the formative years (Bahreman 2013).
17.2.2 Indications for Early Orthodontic Referral and Treatment
It is of utmost importance for primary care dentists to be able to distinguish problems that need to be treated soon and those that can wait for later comprehensive orthodontic care. Indications for early orthodontic referral and treatment can be broadly categorized into the following ten signs seen in a child’s or young adolescent’s dentition:
- 1.
Severe overjet
- 2.
Deep impinging bite
- 3.
Posterior crossbites
- 4.
Anterior crossbites
- 5.
Parafunctional habits
- 6.
Severe crowding
- 7.
Ectopic eruption
- 8.
Delayed eruption and impacted teeth
- 9.
Psychological factors
- 10.
Growth discrepancies
These characteristics should be kept in mind while evaluating children at each regular visit. If identified involving permanent teeth, appropriate measures to prevent, maintain, or correct should be attempted without delay.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


