This case report describes the treatment and long-term follow-up care of a patient diagnosed with cleidocranial dysplasia who had multiple impacted permanent and supernumerary teeth. The aim of the treatment was to provide an adequate esthetic and functional reconstruction of the occlusion with good periodontal care. The patient was treated with a multidisciplinary therapeutic protocol including orthodontic and surgical procedures, and traction of 11 permanent teeth. The proposed objectives of good occlusion, normal function, healthy periodontium, and balanced profile were achieved, and the 3-year follow-up records showed stable results.
Cleidocranial dysplasia (CCD) is a rare congenital bone disorder with an autosomal dominant pattern of inheritance, but approximately 40% of patients appear to have spontaneous mutations that affect both sexes to an equal extent. The prevalence is 1 in a million, with complete penetrance and widely variable expressivity. Clavicle hypoplasia results in placement of the shoulders close to the front of the body, and these patients often seem to have a long neck. The sagittal fontanelle suture is characteristically sunken, giving the skull a flattened appearance. The frontal, parietal, and occipital bones are also prominent, and the sinuses are underdeveloped and narrow.
The face is brachycephalic with an increased transverse diameter of the skull. The eyes are widely spaced, and the base of the nose is depressed and wide. In addition, midfacial hypoplasia, which is most likely related to the shortened anterior cranial base, and a relatively prognathic mandible are craniofacial anomalies frequently associated with the condition. Patients also have reduced height of the lower third of the face and a skeletal Class III tendency because of the underdeveloped maxilla and the upward and forward mandibular rotation.
The oral findings usually identified in patients with CCD are retained deciduous teeth without root resorption and supernumerary teeth that displace the developing permanent teeth and obstruct their eruption, resulting in multiple impacted permanent teeth and a serious malocclusion. The vertical development of the alveolar bone is reduced; there is a late but spontaneous eruption of the permanent first and, usually, the second molars in both jaws, and there is a delay of approximately 3 years in the root development of the permanent teeth.
The teeth often have hypoplastic enamel and dilacerated roots without cellular cementum. Some tooth germs are deformed and rudimentary, and microdontia and twinning are also present.
The treatment of patients with CCD requiring traction of many teeth is a challenge because there is no extensive literature about the subject, making it difficult to follow a protocol of how to perform the traction, especially when the patient is an adult. In this case report, special emphasis has been given to potential dental complications and their management.
Diagnosis and etiology
A woman, 22 years 8 months of age, sought dental treatment at the Department of Dentistry of the Federal University of Santa Catarina in Brazil and was diagnosed with CCD. The facial analysis showed midfacial hypoplasia with poor maxillary growth in the anteroposterior direction. The intrabuccal assessment showed the permanent dentition, with the mandibular midline deviated 3 mm to the left and the maxillary midline deviated 1 mm to the right ( Fig 1 ). The patient had 8 erupted permanent teeth in the maxillary arch and only 5 in the mandibular arch ( Fig 2 ).
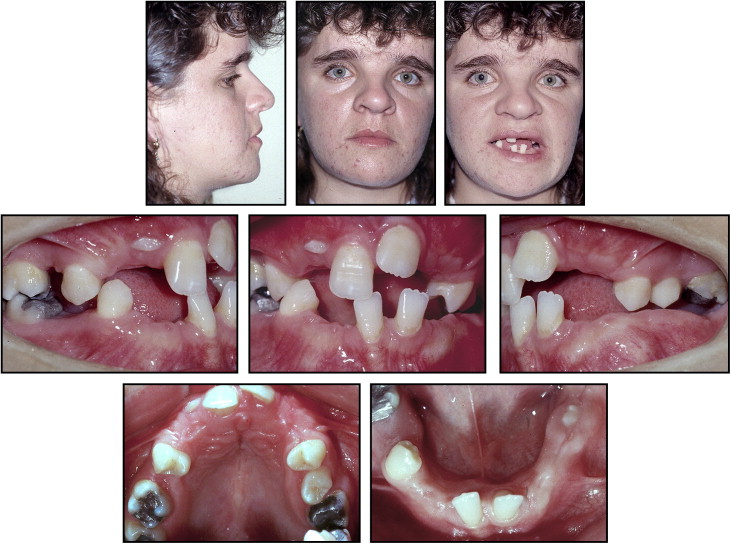
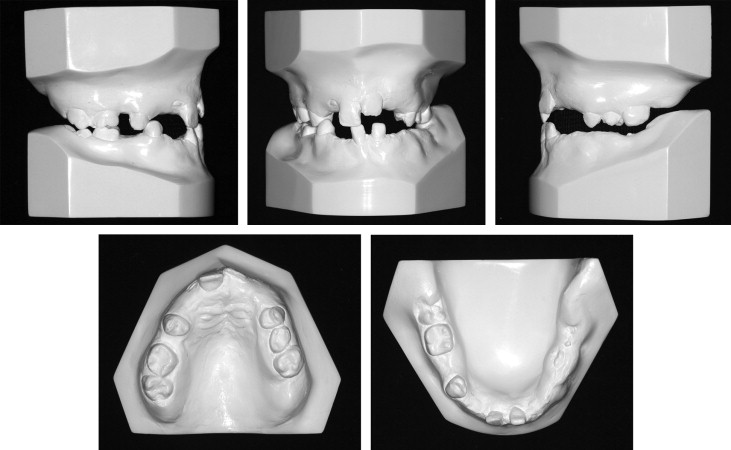
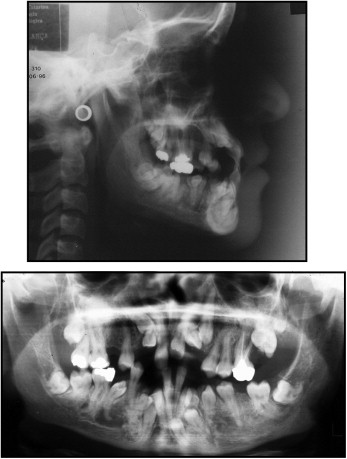
The panoramic radiograph ( Fig 3 ) showed the retained permanent teeth, 3 supernumerary teeth in the mandible, agenesis of the maxillary right second premolar, as well as some dilacerated roots. A radiolucency was observed in the periapical region of the mandibular right premolar tooth, but because there was no pain and the teeth were vital, it was determined to be insignificant. This was also visible in the posttreatment panoramic image, where only a variation in bone pattern was diagnosed, since the adjacent teeth were healthy, and the lamina dura was integrated. The cephalometric radiograph ( Fig 3 ) showed a skeletal Class III pattern caused by forward mandibular rotation with a predominantly horizontal facial growth vector (ANB, 0°; GoGn-SN, 24°; FMA, 20°). The Wits appraisal markedly showed the Class III pattern between the maxilla and the mandible. The incisors were retroclined, especially the mandibular ones (1.NA, 21°; 1-NA, 3 mm; 1.NB, 18°; 1-NB, 2 mm; IMPA, 85°; Table ).
| Measurement | Pretreatment | Posttreatment | Follow-up |
|---|---|---|---|
| Skeletal pattern | |||
| SNA (°) | 89 | 89 | 88 |
| SNB (°) | 89 | 89 | 88 |
| ANB (°) | 0 | 0 | 0 |
| Facial convexity (°) | 0 | −1 | −2 |
| Y-axis (°) | 57 | 57 | 58 |
| Facial angle (°) | 94 | 92 | 92 |
| SN.GoGn (°) | 24 | 23 | 23 |
| FMA (°) | 20 | 19 | 19 |
| AO-BO (mm) | −4 | −3 | −2 |
| Dental pattern | |||
| IMPA (°) | 85 | 92 | 92 |
| 1-NA (mm) | 3 | 6 | 5 |
| 1.NA (°) | 21 | 30 | 29 |
| 1-NB (mm) | 2 | 3 | 3 |
| 1.NB (°) | 18 | 23 | 23 |
| 1.1 (°) | 140 | 125 | 127 |
| Profile | |||
| Upper lip-S line (mm) | −2 | −3 | −3 |
| Lower lip-S-line (mm) | 0 | −2 | −2 |
Treatment objectives
The following treatment objectives were established: (1) clear the path of eruption of the submerged permanent teeth by extraction of the supernumerary teeth; (2) proceed with forced eruption of the permanent teeth with orthodontic traction; and (3) correct the anterior and posterior crossbite and perform dental alignment and leveling to achieve adequate intercuspation. Thus, the main objectives of the treatment for this patient were to create a stable functional occlusion. A balanced profile was also desired.
Treatment objectives
The following treatment objectives were established: (1) clear the path of eruption of the submerged permanent teeth by extraction of the supernumerary teeth; (2) proceed with forced eruption of the permanent teeth with orthodontic traction; and (3) correct the anterior and posterior crossbite and perform dental alignment and leveling to achieve adequate intercuspation. Thus, the main objectives of the treatment for this patient were to create a stable functional occlusion. A balanced profile was also desired.
Treatment alternatives
The aim of dental management of patients with CCD is to achieve an optimal functional and cosmetic result by early adulthood. Unfortunately, this patient received assistance only after she had already reached adulthood, so we had the following alternatives with a multidisciplinary approach.
- 1.
Extraction of all unerupted teeth, followed by orthodontic alignment and leveling of the erupted teeth in preparation for a partial dental prostheses.
- 2.
Surgical exposure of the unerupted teeth to provide support for an overdenture. The overdenture could also be supported by implants. This option also included orthodontic alignment and leveling of the erupted teeth.
- 3.
Removal of the supernumerary teeth, surgical exposure of the impacted teeth, and then their orthodontic traction. First, traction of the unerupted mandibular teeth would occur, supported by a removable appliance in the maxillary arch. When possible, the fixed orthodontic appliance would be applied in the mandibular arch for tooth alignment and, subsequently, traction of the unerupted maxillary teeth.
- 4.
Removal of the supernumerary teeth, surgical exposure of the impacted teeth, and orthodontic traction of the unerupted mandibular and maxillary teeth, supported by skeletal anchorage. Then, when all teeth were erupted in sequence, conventional orthodontic treatment would begin.
Treatment progress
Initially, the supernumerary teeth were extracted. The next step was surgical exposure of the unerupted mandibular teeth. The orthodontic attachments were bonded for traction supported by a maxillary removable appliance. In all forced eruptions, intraoral elastics were applied with a force varying from 50 to 150 g; these were used throughout the day as frequently as possible. Next, edgewise brackets were bonded in the mandibular arch, and we proceeded with alignment and leveling. Once the mandibular teeth were aligned, the patient was referred again to the oral surgeon for exposure of the unerupted maxillary teeth and the bond attachments in the maxillary teeth to support the intraoral elastics and provide traction.
Some teeth were erupted with force. When the patient reached the age of 28 years, the complete fixed appliances were installed.
Expanded arches were used to create space in the arch and slightly project the maxillary anterior teeth. During this phase, the goals were alignment and leveling, anterior and posterior crossbite correction, and improvement of the incisor relationships. The mechanics of the segmented arch with cantilevers were used to assist in tooth traction, and continuous arches with loops were used for leveling and space closure. The mechanics of Class II elastics on the left and Class III elastics on the right were used to correct the midline with a force of 150 g as frequently as possible throughout the day.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


