This article highlights the commonly used medications used in dentistry and oral surgery. General dentists and specialists must be knowledgeable about the pharmacology of the drugs currently available along with their risks and benefits. Enteral sedation is a useful adjunct for the treatment of anxious adult and pediatric patients. When enteral sedation is used within the standards of care, the interests of the public and the dental profession are served through a cost-effective, effective service that can be widely available. Oral sedation enables dentists to provide dental care to millions of individuals who otherwise would have unmet dental needs.
Key points
- •
There is a strong need and demand for adult and pediatric enteral sedation services in dentistry.
- •
Knowledge of the potential risks and benefits of oral sedatives is absolutely necessary to allow the clinician to use an effective anesthesia technique safely in the office setting.
- •
This article highlights the pharmacology of the medications commonly used for oral conscious sedation in dentistry as well as clinical guidelines for administration.
- •
Patient safety is the paramount consideration. Oral administration to achieve conscious sedation requires state regulation to ensure safety.
Dental anxiety has been shown to be one of the biggest barriers for patients in seeking needed care. An estimated 100 million people in the United States (approximately 30%) are in need of dental care but neglect the dental visit. A survey conducted in the United States found that 18% of adults would visit the dentist more frequently if they were given a drug to make them less nervous. With the strong need to treat fearful and anxious adult patients, effective sedation and pain control have become integral components of dental care.
General dental practitioners have used in-office oral sedation for more than 160 years during routine dental practice. The oral route has remained the safest, most established, and most commonly used route of drug administration. Advantages of the oral route of drug administration in adults versus other routes of drug administration include:
- 1.
Lower incidence of adverse reactions
- 2.
Decreased severity of adverse reactions
- 3.
High degree of patient acceptance and compliance
- 4.
Convenience of administration
- 5.
Low cost
- 6.
Additional equipment or personnel not needed
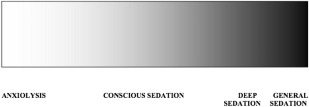
Oral medications are well suited for anxiolysis (minimal sedation) and conscious sedation (moderate sedation) in dentistry. Anxiolysis is a drug-induced state in which patients respond appropriately to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected. Anxiolysis is the lightest level of sedation ( Fig. 1 ).
Oral medication to achieve anxiolysis in adult patients seems to have a wide margin of safety. When the intent is minimal sedation for adults, the appropriate initial dosing of a single enteral drug is no more than the maximum recommended dose (MRD) of a drug that can be prescribed for unmonitored home use. The MRD is the maximum US Food and Drug Administration (FDA)–recommended dose of a drug as printed in FDA-approved labeling for unmonitored home use. Incremental and supplemental dosing both apply to the administration of minimal sedation. Incremental dosing is the administration of multiple doses of a drug until a desired effect is reached, but not to exceed the MRD. During minimal sedation, supplemental dosing is a single additional dose of the initial dose of the initial drug that may be necessary for prolonged procedures. The supplemental dose should not exceed one-half of the initial total dose and should not be administered until the dentist has determined that the clinical half-life of the initial dosing has passed. The total aggregate dose must not exceed 1.5 times the MRD on the day of treatment for minimal sedation. Regulatory agencies in all 50 United States and Canada allow anxiolysis without an additional permit beyond completion of an accredited predoctoral dental training program.
The American Dental Association (ADA) first developed clinical guidelines, including educational requirements, for the use of sedation in dentistry in 1996 and most recently released an update in 2012. In the 2012 ADA clinical guidelines, it is stated that, “For all levels of sedation and anesthesia, dentists, who are currently providing sedation and anesthesia in compliance with their state rules and/or regulations prior to adoption of this document, are not subject to these educational requirements. However, all dentists providing sedation and general anesthesia in their offices or the offices of other dentists should comply with the Clinical Guidelines in this document.” The 2012 ADA Clinical Guidelines for the Use of Sedation and General Anesthesia by Dentists state that to administer minimal sedation (anxiolysis) the dentist must have successfully completed:
- 1.
Training to the level of competency in minimal sedation consistent with that prescribed in the ADA Guidelines for Teaching Pain Control and Sedation to Dentists and Dental Students, or a comprehensive training program in moderate sedation that satisfies the requirements described in the Moderate Sedation section of the ADA Guidelines for Teaching Pain Control and Sedation to Dentists and Dental Students at the time training was commenced; or
- 2.
An advanced education program accredited by the ADA Commission on Dental Accreditation that affords comprehensive and appropriate training necessary to administer and manage minimal sedation commensurate with these guidelines; and
- 3.
A current certification in Basic Life Support (BLS) for Healthcare Providers
Administration of minimal sedation by another qualified dentist or independently practicing qualified anesthesia health care provider requires operating dentists and their clinical staff to maintain current certification in Basic Life Support for Healthcare Providers.
Conscious sedation is defined as, “a minimally depressed level of consciousness that retains the patient’s ability to independently and continuously maintain an airway and respond appropriately to physical stimulation or verbal command and that is produced by a pharmacological or non-pharmacological method or a combination thereof.” All patients pass through anxiolysis before entering conscious sedation. The same drugs that are prescribed for anxiolysis produce oral conscious sedation usually at a dosage greater than 1.5 times the FDA-approved maximum recommended dosage or in combination with other central nervous system (CNS)–altering medications.
According to the 2012 ADA Clinical Guidelines for the Use of Sedation and General Anesthesia by Dentists to administer moderate (conscious) sedation dentists must have successfully completed:
- 1.
A comprehensive training program in moderate sedation that satisfies the requirements described in the Moderate Sedation section of the ADA Guidelines for Teaching Pain Control and Sedation to Dentists and Dental Students at the time training was commenced; or
- 2.
An advanced education program accredited by the ADA Commission on Dental Accreditation that affords comprehensive and appropriate training necessary to administer and manage moderate sedation commensurate with these guidelines; and
- 3.
(i) A current certification in Basic Life Support for Healthcare Providers and (ii) either current certification in advanced cardiac life support (ACLS) or completion of an appropriate dental sedation/anesthesia emergency management course on the same recertification cycle that is required for ACLS
Administration of moderate sedation by another qualified dentist or independently practicing qualified anesthesia health care provider requires the operating dentist and his/her clinical staff to maintain current certification in Basic Life Support for Healthcare Providers.
Per state regulation, oral conscious sedation (moderate sedation) may be safely and effectively administered in the dental office. New York state requirements for a Dental Enteral Conscious Sedation Certificate include 20 clinically oriented experiences in the use of enteral conscious sedation techniques; 18 hours of training, including but not limited to instruction in nitrous oxide and emergency medicine; BLS; and 6 hours of continuing education. In addition, a minimum of 2 individuals must be present in the operatory; such individuals must include the dentist and 1 additional qualified individual. In New York and specified other states, the dentist shall not administer conscious sedation (enteral or parenteral) to more than 1 patient at a time. Six hours of training every 3 years is required for the dentist to renew an oral sedation permit in New York. American dentists can find state-specific regulations at the following link to the chart of state statutory requirements for conscious sedation permits provided by the ADA: http://www.ada.org/∼/media/ADA/Advocacy/Files/anesthesia_sedation_permit.ashx .
Benzodiazepines are the preferred drugs for the management of dental fear and preoperative anxiety. Benzodiazepines are anxiolytic, have sedative properties, and produce anterograde amnesia. These drugs are indicated for the management of mild to moderate anxiety. Benzodiazepines act by facilitating the physiologic inhibitory effects of gamma-aminobutyric acid (GABA), the major inhibitory neurotransmitter in the brain. Benzodiazepines have a high therapeutic index (ratio of the toxic dose of a drug to its therapeutic dose), and therefore possess a high margin of safety, which is the primary advantage compared with other classes of sedative-hypnotics, especially the barbiturates, which have a much lower therapeutic index. Benzodiazepines have proved to be fairly innocuous in intentional or accidental overdose when taken without additional drugs.
Benzodiazepines are effective as single agents, thus drug cocktails are not necessary. Benzodiazepines vary by onset time, duration, metabolism, and in degree of sedation. Triazolam, diazepam, lorazepam, and alprazolam are the most effective and commonly administered benzodiazepines for anxiolysis and conscious sedation in dentistry.
Triazolam (Halcion) was first introduced in the 1980s. It is the most prescribed psychoactive drug and the most popular drug prescribed by dentists to alleviate pretreatment patient anxiety in the United States. Triazolam has been described as a nearly ideal anxiolytic for oral sedation in dentistry because of its short half-life of 1.5 to 5.5 hours and absence of active metabolites. A high level of sleep and amnesic effect is produced by triazolam, with little residual drowsiness or hangover effect. Triazolam has about a 45% bioavailability and an onset of action of approximately 1 hour. If administered sublingually, the rate of onset is improved to about 30 minutes and bioavailability is increased. The reported duration of triazolam is an average 1 to 2 hours.
Triazolam is available in 0.125-mg and 0.25-mg tablets. The average dose is 0.25 mg and the FDA MRD is 0.5 mg. As pregnancy category X, triazolam is contraindicated in pregnant patients. Caution should be taken when using it in the elderly or debilitated because excessive sedation is possible. The initial recommended dose in elderly patients is 0.125 mg. Overdose may occur at 4 times the MRD of 0.5 mg, which is 2 mg or 8 tablets (0.25 mg) ( Table 1 ).
| Dose (mg) | 0.25–0.5 Average: 0.25 MRD: 0.5 |
| Onset | 1 h 30 min; sublingual |
| Duration (h) | 1–2 |
| Contraindications | Pregnancy |
| Precautions | Excessive sedation possible in elderly |
| Availability | Tablets: 0.125, 0.25 mg |
| Active Metabolites | None |
| Pregnancy Category | X |
| Classification | Sedative/hypnotic |
Diazepam (Valium) was synthesized in 1959 and marketed in 1963. Diazepam was the leader among prescription drugs by the 1970s, and remained so until recently. After oral administration, diazepam has an onset of about 1 hour, achieving 90% of maximal clinical effect. Peak onset of plasma levels occurs within 2 hours. From the presence of active metabolites and prolonged plasma half-life of 20 to 70 hours, a long-lasting effect may occur with prolonged oral administration. Because of the presence of active metabolites, patients may experience a hangover effect. Diazepam is well tolerated in elderly patients. The recommended dose of diazepam for anxiolytic premedication is 5 to 10 mg 1 hour before treatment. It is available in 2-mg, 5-mg, and 10-mg tablets and 10 mg/5 mL syrup ( Table 2 ).
| Dose (mg) | 2–20 |
| Onset (h) | 1 |
| Duration (h) | 1–3 |
| Contraindications | Allergy, acute narrow-angle glaucoma |
| Precautions | Sedation intensified with CYP3A4 and CYP2C19 inhibitors |
| Availability | Tablets: 2, 5, 10 mg Syrup: 10 mg/5 mL |
| Active Metabolites | Yes |
| Pregnancy Category | D |
| Classification | Antianxiety |
Lorazepam was marketed in 1977 under the trade name Ativan. The drawback to the use of lorazepam is the longer onset time of 1 to 2 hours. Thus, administration may be best suited for patients at home before the dental visit. Lorazepam has a profound amnestic and effective antianxiety affect. Its usage is well tolerated in elderly individuals. Lorazepam is contraindicated in patients with narrow-angle glaucoma and with a known allergy to benzodiazepines. Caution must be taken to not oversedate the patient and in patients with a depressive disorder or psychosis. Reported side effects include sedation (15.9%), dizziness (6.9%), weakness (4.2%), and ataxia (3.4%). For preoperative anxiety control, a dose of 2 to 4 mg may be given or prescribed 1 to 2 hours before the dental appointment ( Table 3 ).
| Dose (mg) | 2–4 |
| Onset (h) | 1–2 |
| Duration (h) | 2–4 |
| Contraindications | Allergy, acute narrow-angle glaucoma |
| Precautions | Oversedation, depressive disorders, psychosis |
| Availability | Tablets: 0.5, 1, 2 mg |
| Active Metabolites | None |
| Pregnancy Category | D |
| Classification | Antianxiety Sedative/hypnotic |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


