Introduction
To increase stability and mandibular setback movement, surgical maxillary impaction is normally performed with mandibular setback surgery in treating adult skeletal Class III patients. This article demonstrates the use of microimplants for anchorage to intrude molars and the resultant rotation of the maxillary occlusal plane clockwise to increase the surgical mandibular setback and reduce the posterior vertical dimension instead of maxillary surgical impaction.
Methods and Results
A 21-year-old man with mandibular prognathism was treated with mandibular setback surgery that included orthodontic treatment for decompensation. Microimplants placed into the palatal alveolar bone between the maxillary first and second molars were used to intrude the maxillary posterior teeth and change the occlusal plane clockwise. This produced 4 mm more of distal movement of the chin during mandibular setback surgery compared with the surgical prediction with no change in the occlusal plane. These results were similar to those of 2-jaw surgery with maxillary posterior impaction.
Conclusions
The intrusion of the maxillary posterior teeth with microimplants might prevent the need for maxillary surgery in adult skeletal Class III patients.
Skeletal anchorage has made it possible to correct malocclusions that were impossible to correct with conventional orthodontic mechanics. The use of microimplants has increased over other skeletal anchorage systems, dental implants, and miniplates, thanks to their low-cost, easy surgical placement and removal, and few anatomic limitations. Because of their small size, they can be placed between the roots of the teeth.
Microimplants can provide anchorage for en-masse retraction of the anterior tooth segments and the whole arch, intrusion of 1 tooth or more, and protraction of the molars. Furthermore, microimplants might bring about skeletal changes after surface bone resorption after bodily retraction of anterior teeth and mandibular skeletal changes by auto-rotation of the mandible after intrusion of the molars in open-bite treatment. With the aid of microimplants, clinicians can move teeth exactly to the goal.
The first treatment option for an adult with a skeletal Class III malocclusion is orthognathic surgery, which consists of 2-jaw or 1-jaw mandibular surgery. The presurgical orthodontic treatment is basically a decompensation process to align and level the teeth properly in relation to the jaw bones. The position of teeth in the conventional technique can be controlled mainly by extraction of teeth and partly by the patient’s compliance in using extraoral anchorage devices. However, with microimplants, we clinicians can control tooth movement precisely and 3 dimensionally. The anteroposterior or vertical position of the anterior or posterior teeth can be controlled by microimplants. Control of the maxillary occlusal plane in patients with facial asymmetry could eliminate the need for maxillary jaw surgery. Control of the occlusal plane in an anteroposterior direction could change the distal movement of the proximal segment in mandibular setback surgery, and this could enhance the profile improvement. Here, we describe a patient whose teeth were positioned in a proper position relative to the jaw base with microimplant anchorage and discuss the effect of maxillary molar intrusion on the amount of mandibular setback surgery.
Diagnosis and etiology
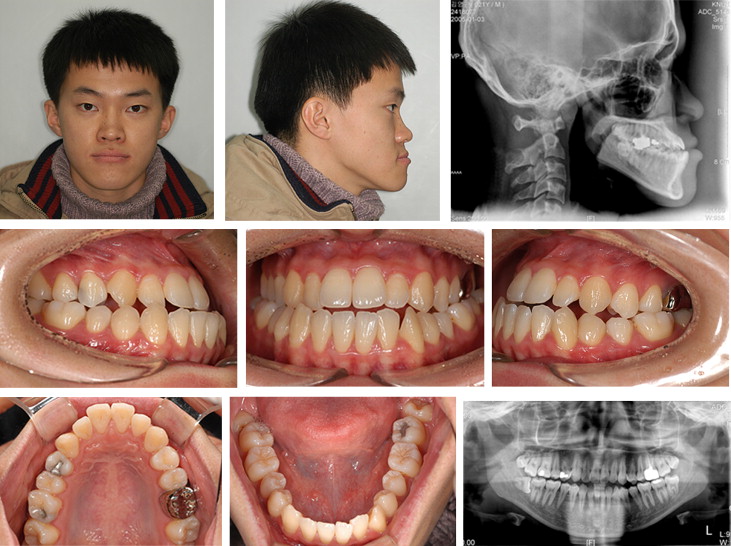
A 21-year-old man with mandibular prognathism came for treatment ( Fig 1 ). He had a Class III sagittal skeletal relationship with a concave profile. The etiology of mandibular prognathism was assumed to be overgrowth of the mandible; the SNB angle was 88°, the position of pogonion relative to the nasion-perpendicular was 16.8 mm (normal range, –2 to +4 mm), and the distance from condylion to anatomic gnathion was 130.4 mm (normal value, 119.4 ± 5.3 mm) ( Table ). The FMA was 23°, and the lower facial height was 64.3 mm. The nasolabial angle was 80°. The patient’s vertical skeletal proportions were normal, and there was no facial asymmetry.
| Pretreatment | Before surgery | Posttreatment | |
|---|---|---|---|
| SNA (°) | 83 | 83 | 83 |
| SNB (°) | 88 | 88.5 | 81 |
| ANB (°) | –5 | –5.5 | 2 |
| NaP-A (mm) | 3.4 | 2.7 | 1.5 |
| NaP-Pog (mm) | 16.8 | 17.8 | 2.6 |
| Co-A (mm) | 91.7 | 90.5 | 89.3 |
| Co-Gn (mm) | 130.4 | 140 | 120 |
| ANS-Me (mm) | 72 | 71.2 | 71 |
| FMA (°) | 19 | 18.5 | 25.5 |
| PFH/AFH | 53/71.5 (0.74) | 51/71.5 (0.71) | 44/70.5 (0.62) |
| FH to OP (°) | –2.8 | 0.8 | 3.5 |
| FH to UI (°) | 140.5 | 127.5 | 128.5 |
| IMPA (°) | 84 | 83 | 78.5 |
| Z-angle (°) | 87 | 82.5 | 82.5 |
| Nasolabial angle (°) | 80 | 87 | 100 |
| Upper lip to E (mm) | –3 | –4.8 | –2 |
| Lower lip to E (mm) | 2.8 | 5.5 | –1 |
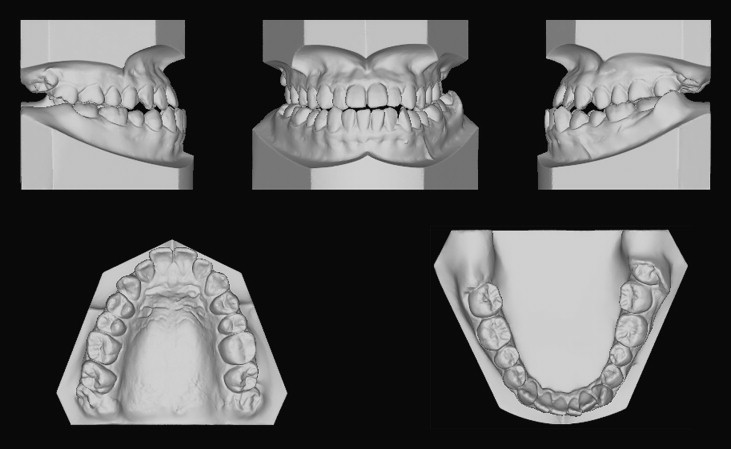
Intraorally, the patient had Class III canine and molar relationships ( Figs 1 and 2 ). He had –4 mm of overjet and 0 mm of overbite. Both maxillary and mandibular midlines were coincident with the patient’s facial midline. The maxillary anterior teeth were proclined (angle of the maxillary incisors to Frankfort horizontal [FH] plane, 140.5°), and the mandibular anterior teeth were retroclined (angle of the mandibular incisors to the mandibular plane, 84°). This showed dentoalveolar compensation for the sagittal skeletal discrepancy. The cant of occlusal plane to the FH plane was –2.8°. Arch-length discrepancies in the maxillary and mandibular arches were –2 and –4.5 mm, respectively. There was no apparent transverse discrepancy.
Treatment objectives
Five treatment objectives were identified: (1) correct the mandibular prognathism, (2) balance the position of the upper lips after positioning the maxillary anterior teeth properly relative to the maxilla, (3) change the occlusal plane in a clockwise direction by intruding the maxillary posterior teeth about 2 mm to increase the surgical mandibular setback movement, (4) establish functional occlusion with normal overbite and overjet, and (5) resolve crowding.
Treatment objectives
Five treatment objectives were identified: (1) correct the mandibular prognathism, (2) balance the position of the upper lips after positioning the maxillary anterior teeth properly relative to the maxilla, (3) change the occlusal plane in a clockwise direction by intruding the maxillary posterior teeth about 2 mm to increase the surgical mandibular setback movement, (4) establish functional occlusion with normal overbite and overjet, and (5) resolve crowding.
Treatment alternatives
The first treatment option was mandibular setback surgery. Surgical setback movement of the mandible was necessary to obtain facial esthetics and normal occlusion. Presurgical orthodontic treatment would include extraction of the maxillary first premolars, alignment of the crowded anterior teeth, linguoversion of the maxillary anterior teeth, and labioversion of the mandibular anterior teeth.
The second alternative was 2-jaw surgery with clockwise rotation of the maxillary occlusal plane (jaw rotation). Surgical impaction of the maxillary posterior segment reduces the posterior vertical dimension or maintains the vertical length of the masseteric ring; these movements enhance posttreatment stability. Impaction of the maxillary posterior segment also increases the surgical mandibular setback movement.
The third treatment option was mandibular 1-jaw surgery after control of the tooth positions 3 dimensionally with microimplants. Clockwise rotation of the maxillary occlusal plane after intrusion of the maxillary posterior teeth can cause clockwise rotation of the distal segment of the mandible during mandibular setback surgery. Intrusion of the maxillary posterior teeth can be performed easily and efficiently with microimplants. This orthodontic procedure can eliminate maxillary surgery. The ease of the surgical procedure and the expected good treatment effects led the patient to choose this option.
Treatment planning
Both cephalometric prediction and paper surgery has been done. For presurgical orthodontic treatment, extraction of the maxillary first premolars and the maximum retraction of the maxillary anterior segment were planned, because the patient had an acute nasolabial angle and proclined maxillary inciors. Because the incisal tip of the maxillary incisors was positioned high in relation to the reposed upper lip, extrusion of the maxillary incisors was planned during distal retraction and lingual tipping of the maxillary incisors. Labioversion of the mandibular incisors provides a better chin-lower lip line.
To change the maxillary occlusal plane in the clockwise direction, intrusion of the maxillary posterior teeth was planned. Intrusion of the posterior teeth seemed more rational than extrusion of the anterior teeth, because the vertical position of the maxillary incisors could allow only 2 mm of extrusion, and extrusion of the anterior teeth is reportedly more prone to relapse. Microimplants can be used for anchorage to intrude the maxillary posterior teeth. The decision on the amount of intrusion was made on the basis of the paper surgery. Bilateral sagittal split ramus osteotomy was planned.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


