Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Recognize the clinical criteria that determine when to obturate.
- 2.
List the criteria for the ideal obturating material.
- 3.
Describe the purpose of obturation and the reasons inadequate obturation may result in treatment failure.
- 4.
Identify the core obturating materials most commonly used and list their constituents and physical properties.
- 5.
Describe the advantages and disadvantages of each core material.
- 6.
Discuss the indications and contraindications for obturation with each core material.
- 7.
Differentiate between standardized, nonstandardized, and tapered sizes of gutta-percha (GP) cones and discuss when each is indicated.
- 8.
Define and differentiate between lateral and vertical compaction and suggest where each is indicated.
- 9.
Describe the lateral compaction technique.
- 10.
Discuss the significance of depth of spreader penetration during lateral compaction.
- 11.
Describe the vertical compaction technique.
- 12.
Describe briefly other techniques used for obturation, including thermoplasticization, thermocompaction, paste injection, core carrier systems, and sectional obturation.
- 13.
Describe the custom cone (chloroform-softened) technique and discuss when it is indicated.
- 14.
Describe the preparation of the canal for obturation.
- 15.
Review the techniques for final drying and apical clearing.
- 16.
Discuss the technique for fitting the master cones.
- 17.
List criteria for the ideal sealer.
- 18.
Describe a technique for mixing and placing a sealer.
- 19.
Discuss the technique for removing excess sealer and obturating material from the chamber and explain why this process is necessary.
- 20.
Discuss the clinical and radiographic criteria for evaluating the quality of obturation.
Learning Objectives
After reading this chapter, the student should be able to:
- 1.
Recognize the clinical criteria that determine when to obturate.
- 2.
List the criteria for the ideal obturating material.
- 3.
Describe the purpose of obturation and the reasons inadequate obturation may result in treatment failure.
- 4.
Identify the core obturating materials most commonly used and list their constituents and physical properties.
- 5.
Describe the advantages and disadvantages of each core material.
- 6.
Discuss the indications and contraindications for obturation with each core material.
- 7.
Differentiate between standardized, nonstandardized, and tapered sizes of gutta-percha (GP) cones and discuss when each is indicated.
- 8.
Define and differentiate between lateral and vertical compaction and suggest where each is indicated.
- 9.
Describe the lateral compaction technique.
- 10.
Discuss the significance of depth of spreader penetration during lateral compaction.
- 11.
Describe the vertical compaction technique.
- 12.
Describe briefly other techniques used for obturation, including thermoplasticization, thermocompaction, paste injection, core carrier systems, and sectional obturation.
- 13.
Describe the custom cone (chloroform-softened) technique and discuss when it is indicated.
- 14.
Describe the preparation of the canal for obturation.
- 15.
Review the techniques for final drying and apical clearing.
- 16.
Discuss the technique for fitting the master cones.
- 17.
List criteria for the ideal sealer.
- 18.
Describe a technique for mixing and placing a sealer.
- 19.
Discuss the technique for removing excess sealer and obturating material from the chamber and explain why this process is necessary.
- 20.
Discuss the clinical and radiographic criteria for evaluating the quality of obturation.
Objectives of “Obturation”
Historically, obturation has been considered one of the critical steps of root canal treatment and, when not properly performed, a potential cause of treatment failure. An early and often quoted report stated that most treatment failures could be attributed to inadequate obturation. Healing was evaluated radiographically at various times after root canal treatment. Such retrospective surveys, however, have major limitations; the outcome may demonstrate clearly a correlation between the observed failures and poorly obturated root canal systems (RCSs), but just because two events are associated does not prove cause and effect. In other words, although RCSs in these failed treatments may not have demonstrated radiographically dense obturations, other factors may have caused irritation of the periapical tissues and failure, such as (1) loss of or an inadequate coronal seal, (2) inadequate debridement and disinfection, (3) missed and untreated RCSs, (4) vertical root fractures, (5) significant periodontal disease, (6) coronal fractures, (7) poor aseptic technique, and (8) procedural errors (e.g., incorrect length, ledging, zipping, and perforations).
Significantly, a periapical lesion may heal temporarily after debridement without obturation. Although this is not an acceptable treatment option, it does demonstrate an important concept: what is removed from the RCS is more important than what is inserted into it. The goal is to create a watertight seal to maintain a clean and disinfected RCS environment and to provide an optimum state for the health of the periapical tissues.
The objective of obturation is to create a watertight seal along the length of the RCS from the coronal opening to the apical termination. Traditionally the importance of establishing and maintaining a coronal seal has been overlooked; the quality of the coronal seal wasn’t deemed important. However, it is now known to be as important as the apical seal to a long-term favorable outcome. A watertight coronal seal can prevent residual microbes in the RCS from gaining access to the periodontal ligament, causing disease. It also minimizes the entry of new microbes into the RCS from the apical foramen, lateral or accessory canals, coronal opening, or odontoblastic tubule dead tracts.
Potential Causes of Failure
Most treatment failures related to deficiencies in obturation are long-term failures. A low volume of irritant or the slow release of irritant into periapical tissues causes damage that is not apparent in the short term. The persistence or development of periapical pathosis may not be evident for months or even years after treatment. Therefore, recall evaluation to assess healing is important. Obturation-related failures may occur in different ways as described in the following sections.
Apical Seal
Leaving Debris in the RCS
Bacteria, tissue debris, and other irritants are usually not totally removed during cleaning and shaping (see Chapter 16 ). These constitute a potential source of irritation to periapical tissues that may not allow healing. Sealing these irritants in the RCS during obturation may prevent (or limit) their escape into the surrounding tissues. This seal must remain intact indefinitely because this reservoir of irritants may persist and cause disease years later. Interestingly, some bacteria sealed in the canal may lose viability, probably because of lack of substrate. Other bacteria may remain dormant, waiting for the introduction of substrate to proliferate and cause disease. Even dead bacteria or their remnants can be irritating or antigenic and cause inflammation and negative immunologic consequences.
Traditionally the apical foramen has been viewed as the main point of entry of microbes into the RCS. Later investigations have reported that, in fact, coronal microleakage often is the primary means of microbial entry.
Coronal Seal
Irritants from the Oral Cavity
A coronal seal is extremely important because if the myriad of irritants present in the oral cavity gain access to the RCS and subsequently to the periapical tissues, they may cause inflammation and prevent healing. Irritants include microorganisms, food, chemicals, or other agents that pass through the mouth.
If a properly obturated RCS is exposed to saliva, a dissolution of sealer (with subsequent leakage over a relatively short period) may occur. This results in leakage of bacteria, toxins, and chemicals into, and around, the gutta-percha (GP). The consequences of sealer loss are obvious; communication between the oral cavity and the periodontal ligament (PDL) eventually becomes complete via accessory canals, dead tracts, or the apical foramen.
It is not possible to determine clinically whether the passage of irritants from the oral cavity to the periapex has occurred. Therefore, it is unwise to restore a tooth in which an RCS has been exposed to saliva, bacteria, food debris, or other irritants from the oral cavity. Coronal exposure of the obturating material for longer than a short period, through loss of restoration, recurrent caries, or defective margins, requires retreatment. The duration of exposure that indicates retreatment depends on various factors, such as the quality of the obturation, the length of the RCS, and/or the surface area of exposure.
Restoration
Proper material selection and a superlative placement technique are critical. This aspect of the overall treatment is an integral part of obturation. The restoration acts as a protector of tooth structure and is the primary coronal seal, whether temporary or definitive. These factors are discussed in detail in Chapter 17 .
Lateral Seal
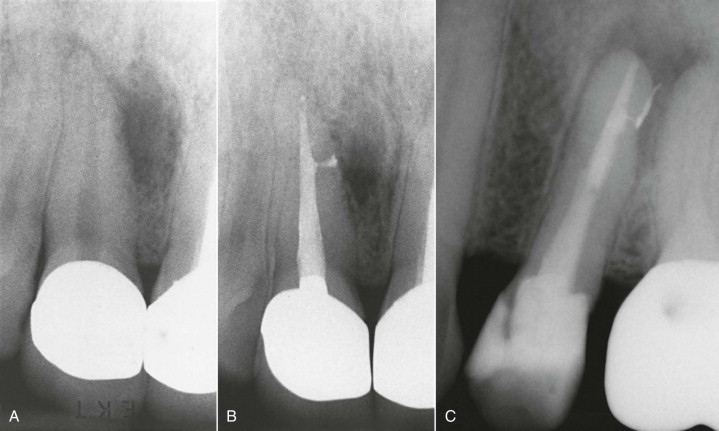
The lateral seal is not as critical as the apical and coronal seals. Lateral/accessory canals are normally subcrestal and do not communicate with the oral cavity. However, establishment of a seal in the middle third of the RCS is also important. Lateral canals are often found in these regions; they constitute a potential channel for irritants from the RCS to the PDL ( Fig. 18.1 ).
Length of Obturation
The extent of the obturation mass relative to the apical foramen is also important. Ideally, obturating materials should remain within the RCS.
Overextension (Overfill)
Overextensions are undesirable. Prognostic studies report that failures increase with time when the primary obturating material has been extruded beyond the apical foramen. Histological examination of periapical tissues after overextension (overfill) typically demonstrates increased inflammation and delayed or impaired healing. Patients also experience more postobturation discomfort. Two other problems with overextension are irritation from the material itself and an inadequate apical seal.
Obturating Materials
Whether the obturation material is core or sealer, both are irritants, to a greater or lesser degree, when in contact with host tissues. The GP core can cause mild tissue irritation initially. Sealers are toxic and invoke a foreign body response and inflammation when they are in contact with tissues. The irritation from the sealer continues until the sealer sets. A small amount of sealer passing out of the foramen into PDL may not be a significant problem. However, when there is gross overextension of the primary obturating material and the sealer, persistent inflammation and failure can result ( Fig. 18.2 ).

Lack of Apical Seal Secondary to Overextension
Lack of an adequate apical seal may be even more important than irritation from the materials. GP, like amalgam, requires a matrix to compact against. An analogy is trying to compact and form amalgam into a Class II preparation without a metal matrix. The same is true of GP and sealer. Absence of an apical matrix or barrier may prevent sufficient lateral and vertical compaction, resulting in an inadequate seal. A tapered apical preparation helps form an adequate matrix for GP compaction and facilitates an adequate apical seal, with or without a small amount of sealer passing through the foramen into the PDL.
Obturation Short of the Apical Construction (Underfill)
An underfill results when both the preparation and the obturation mass are short of the desired working length (WL) or when the obturation does not extend to the WL. Either of these circumstances, or failure to treat a canal, may contribute to lack of healing, particularly long term ( Fig. 18.3 ).

The “optimal” preparation/obturation length for a properly prepared RCS is slightly short of the apical foramen. Preparation or obturation excessively short of these lengths (more than 3 mm) may leave existing or potential irritants in the RCS. Periapical inflammation may then develop over an extended period, depending on the volume of irritants or the balance established between irritants and the immune system.
Compared with overfill, underfill is less of a problem, as indicated by outcome assessment and histologic studies. Therefore, it is preferable to err on the short side to confine everything to the interior of the RCS.
Lateral Canals
The role of lateral and/or accessory canals in root canal treatment has been a subject of debate. These canals connect the RCS to the PDL. Irritants in the RCS, such as bacteria and necrotic debris, may gain access to the lateral PDL and initiate inflammation (see Fig. 18.1 ). Histological examination of roots after debridement has demonstrated that lateral canals are rarely, if ever, debrided. However, certain techniques tend to move core material and/or sealer (primarily) into a lateral or accessory canal. When the main RCS has been adequately cleaned, shaped, and obturated, radiolucencies adjacent to lateral canals heal as readily as periapical lesions. This typically occurs whether the obturating material has or has not been expressed into a lateral or accessory canal. In general, the obturation of lateral canals is inconsequential to the outcome of most root canal treatments, despite the claims that certain techniques fill lateral canals.
Vertical Root Fractures
A vertical root fracture (VRF) is a devastating occurrence that usually requires removal of the tooth or the fractured root through a root amputation or hemisection. Signs and symptoms, in addition to radiographic findings, demonstrate that bone loss and soft tissue lesions are common. Lateral forces exerted during obturation or post placement are major etiologic factors in VRFs, owing to their wedging action. However, many crown/root fractures are idiopathic. The pathogenesis, findings, and prevention of vertical fractures are discussed further in Chapter 8 .
Timing of Obturation
When questions arise, such as, “When is treatment to be completed?” or “Is it time to obturate?” the following factors must be considered: signs and symptoms, pulp and periapical status, and difficulty of the procedure. Combinations of these factors affect the decisions made about the number of appointments and the timing of obturation.
Patient’s Symptoms
In general, if the patient presents with severe symptoms and the diagnosis is symptomatic (acute) apical periodontitis or abscess, obturation is contraindicated. These are emergency situations; therefore, it is preferable to manage the immediate problem and delay definitive treatment. Acute apical abscesses have been treated in a single appointment, although this is generally not recommended.
Painful irreversible pulpitis is a different situation. Because the inflamed pulp (the source of the pain) is removed, obturation may be completed at the same appointment, time permitting.
Pulp and Periapical Status
Vital Pulp
If time and the situation permit, the procedure may be completed in a single visit, regardless of the inflammatory status of the pulp.
Necrotic Pulp
Without significant periapical discomfort, obturation may be completed during the same appointment as RCS preparation. Pulp necrosis with asymptomatic apical periodontitis or chronic apical abscess, or condensing osteitis alone, is not necessarily a contraindication to single-appointment treatment.
There may be advantages to multiple appointments. Placement of an intracanal antimicrobial dressing (e.g., calcium hydroxide) reduces bacteria. Calcium hydroxide in the RCS for 7 days reduces the bacterial load. A comparison of single-visit to multiple-visit intracanal calcium hydroxide treatment did not demonstrate differences in the long-term prognosis. However, the presence of bacteria in the RCS at the time of obturation may have a significant impact on the long-term prognosis. At present, there are no definitive conclusions about when single- or multiple-visit procedures are indicated in which situations. The decision for obturation should be based on thorough canal disinfection procedures.
One situation that contraindicates single-visit care is the persistence of exudation into the RCS during preparation. The potential for post-treatment exacerbation is increased if the periapical lesion is productive and generates continual drainage. If the canal is sealed, pressure and corresponding tissue destruction may proceed rapidly. In these cases, cleaning and shaping are completed, followed by calcium hydroxide placement. In general, exudation is diminished and controllable at a subsequent appointment, and obturation may then be completed.
Degree of Difficulty
Complex cases are time-consuming and may be better managed in multiple appointments. If the treatment period would exceed 2 hours and/or the clinician believes that he or she may be better prepared to treat the case at subsequent appointments, obturation should be delayed.
Culture Results
Obtaining cultures is a procedure in use many years ago. The principle was to obtain negative cultures prior to obturation. However, there was no substantive documentation that the technique or the outcomes were valid. Thus, this technique is no longer used universally.
Number of Appointments
The decision on the number of appointments needed usually is made during initial treatment planning. The decision to schedule another appointment, when made during an appointment, reflects a change of circumstances. For example, the patient or dentist becomes tired or has lost patience, or the RCS continues to drain.
Core Obturating Materials
Primary obturating materials are usually solid or semisolid (paste or softened form). These comprise the bulk of material that will fill the RCS and may or may not be used with a sealer. A sealer is essential with all solid obturating materials, although sealers behave differently with different obturating materials and techniques.
Obturating materials may be introduced into the canals in different forms and may be manipulated by different means once inside. These materials and methodologies are discussed in some detail; alternatives also are discussed, but in less detail. Whatever the material, there are desirable properties that must be considered ( Box 18.1 ).
Grossman suggested that the ideal obturant would do the following :
- ▪
Be easily introduced into the canal
- ▪
Seal the canal laterally and apically
- ▪
Not shrink after insertion.
- ▪
Be impervious to moisture
- ▪
Be bactericidal or at least discourage bacterial growth
- ▪
Be radiopaque
- ▪
Not stain the tooth structure
- ▪
Not irritate periapical tissues or affect the tooth structure
- ▪
Be sterile or easily sterilized
- ▪
Be easily removed from the root canal
Currently, no material or combination of materials satisfies all these criteria.
Solid Materials
Solids have major advantages over semisolids (pastes). Although various materials have been used, the only one universally accepted as the primary material is gutta-percha. It has withstood the test of time and research and is by far the most commonly used. Synthetic resin–based core materials are also available (these are discussed later in the chapter).
Major advantages of solid cores over semisolid paste types is the clinician’s ability to better control length and also a reasonable ability of the solid material to adapt itself to irregularities and create an adequate seal throughout the root canal system (RCS).
Gutta-Percha
Composition
The primary bulk ingredient of a GP cone is zinc oxide (±75%). GP, which is a congener of rubber, accounts for approximately 20% and gives the cone its unique properties (e.g., plasticity). The remaining ingredients are binders, opaquers, and coloring agents.
Shapes
GP cones are available in two basic shapes, standard and nonstandard (or conventional). In general, standardized sizes conform to the requirements of either the International Organization of Standardization (ISO) or the American Dental Association/American National Standards Institute (ADA/ANSI). Nonstandard materials and equipment do not conform to those requirements. Standardized cones are designed to have the same size and taper as the corresponding endodontic instruments used to prepare the RCS; that is, a No. 40 cone with an 0.04 taper should correspond to a No. 40 nickel-titanium (NiTi) rotary instrument with an 0.04 taper.
Clinical observations and studies indicate that commercially available so-called standardized cones show wide variations in size and taper. This lack of uniformity is not critical; however; canal shape after preparation is also variable.
GP master cones (MCs) with varying tapers tend to be selected according to the method of canal preparation or to match the master apical file tip size and corresponding taper.
Advantages
GP was introduced as an obturating material more than 160 years ago. Due to its usefulness and popularity, it has become the standard to which other obturating materials are compared.
GP has a number of advantages. First, because of its plasticity, it adapts with compaction to irregularities in prepared canals, especially when thermoplasticized. Second, it is relatively easy to manage and manipulate, even with complex obturation techniques. Third , GP is relatively easy to remove from the RCS, either partially to allow post placement or totally for retreatment. Fourth, GP is relatively biocompatible, being nearly inert over time when in contact with connective tissue. If a cone becomes contaminated, it can be effectively sterilized by immersion in sodium hypochlorite (1% concentration or greater) for 1 minute.
Sealability
Studies show that, regardless of the technique, the use of GP without a sealer does not result in an adequate seal. Disadvantages of GP include lack of chemical adhesion to each other and, more important, to dentin. When heat is applied or GP is mixed with solvents (e.g., chloroform or eucalyptol), it shrinks markedly during cooling or with evaporation of the solvent, leaving space between the core and dentinal walls. A sealer is used because it fills the spaces between the GP cones and between the GP and the RCS wall. However, it has been reported that the sealer does not predictably fill all of these spaces and coat the walls.
Methods of Obturation
As stated earlier, obturation methods are varied and imaginative. Enterprising dentists and manufacturers have devised (and sell) a variety of devices (with special techniques) in an attempt to enable the clinician to obturate more quickly and effectively.
The most popular obturation method is lateral compaction, followed by warm vertical compaction. Other techniques involve either chemical or physical alteration of the GP in an attempt to render the material more plastic, which assists in adaption to either additional GP or the RCS walls.
Another variation is a system that includes a solid core (carrier) surrounded by a coating of GP. The carrier may be stainless steel or titanium but is more typically plastic. After RCS preparation, the carrier and GP are warmed in a heater specifically designed for this purpose and placed in the canal as a unit.
Other technologies have been introduced that involve warming, plasticizing, and injecting GP. All are discussed in more detail later in this chapter.
Resin
Synthetic polyester resin–based polymers have been advocated as an obturation material ( Fig. 18.4 ). The core material, composed of polycaprolactone with fillers of bioactive glass and other components, is used with a dual-cured Bis-GMA resin sealer and self-etching primer. This combination is an attempt to form a single entity, or so-called monoblock, in the RCS; it involves a chemical bond between the sealer and dentin and the sealer and core material. The material has been reported to be noncytotoxic, biocompatible, and nonmutagenic and has been approved for use by the U.S. Food and Drug Administration (FDA). Early research reported that this material was more resistant to leakage than GP. More recent evidence indicates no difference in leakage compared to more standard techniques. The resin cores, available in nonstandard and standard sizes, have handling properties similar to those of GP and can be removed by solvents and heat if retreatment is indicated. Pellets are also available for use in thermoplastic injection techniques. As yet there are no controlled clinical trials with long-term evaluation to demonstrate how this system compares to GP as an obturating material.

Silver Points
Silver points were designed to correspond to the last file size used in preparation and presumably to fill the RCS precisely in all dimensions. This would be ideal if the preparation were round, a shape that is rarely achieved. It is impossible to predictably prepare an RCS to a uniformly round shape. It was thought that silver points had oligodynamic properties, but later evidence indicated that they did not.
Although the short-term sealability success of silver points seemed comparable to that of GP, silver points are a poor long-term choice as a routine obturating material. Their major disadvantages are lack of adaptability ( Fig. 18.5 ) and possible toxicity to periapical tissues from corrosion. Also, because of their tight frictional fit, silver cones are difficult to remove, either totally during retreatment or partially during post space preparation.
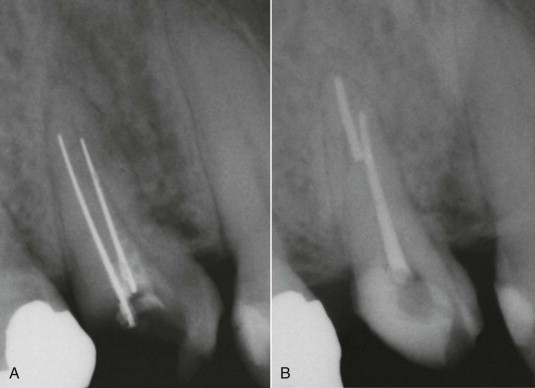
Silver cones are not recommended.
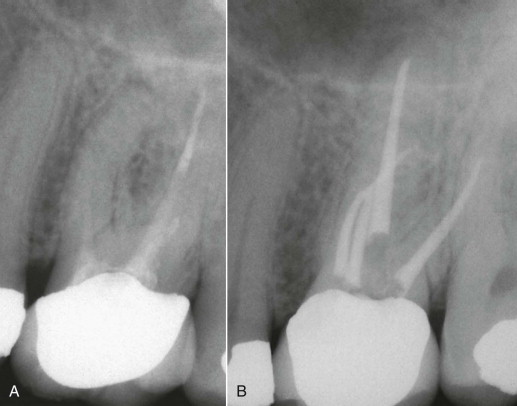
Pastes (Semisolids)
It seemed like a great idea: why not develop a paste or cement with bioactive ingredients? This material could be mixed in a liquid or putty form and injected to the WL, obturating the entire RCS, and then allowed to set. The process would be faster, the paste would fill the entire canal space, and obturation would be much simpler.
Although the concept is appealing, there are significant practical difficulties. The major disadvantages with the use of paste materials are lack of predictable length control, shrinkage, toxicity of ingredients, preclinical difficulties in introduction of the material without voids, and resorbability of the materials.
Paste filling is not recommended.
Types
Zinc Oxide–Eugenol (ZnOE)
ZnOE may be used in its pure state in primary teeth because it is resorbable as the tooth is exfoliated. However, it is generally not advocated in permanent teeth. Other formulations combine ZnOE with various additives. The types known as N2 and RC2B are most common. These are derivations of Sargenti’s formula and contain opaquers, metallic oxides (lead) or chlorides (mercuric), steroids (at times), plasticizers, paraformaldehyde, and various other ingredients. Claims of antimicrobial properties, biologic therapeutic activity, and superiority are made for these paste formulations. However, no scientific evidence exists verifying that they contribute any beneficial aspects to healing. In fact, most of these additives are very toxic. In 1998 the American Association of Endodontists issued a position statement on the use of paraformaldehyde-containing endodontic filling materials.
Use of these materials is below the standard of care and therefore not recommended.
Plastics
It has been suggested that a resin-based sealer, such as AH26 or Diaket, be used as the sole obturating material. These sealers have the same disadvantages as other pastes and are therefore not recommended.
Techniques of Placement
Various methodologies have been advocated for insertion of pastes and/or sealers. Two popular methods are injection and placement with a Lentulo spiral.
Injection is accomplished using a syringe-type device with a barrel and special needles. The paste is mixed and placed in the barrel, a screw handle is inserted and twisted, and the paste is extruded through the needle. The needles are placed deep in the canal, and the paste is expressed as the needles are slowly backed out of the canal. Advocates claim that this method completely fills the canal from the apical portion to the canal orifice. However, it is not unusual for voids to develop, resulting in a short or overextended obturation.
Paste placement is assisted using Lentulo spiral drills. The paste is mixed and placed into the chamber, and the Lentulo drill is spun into the RCS. The RCS is filled with paste, and the drill is slowly withdrawn, as with the syringe device. The reverse spiral on the Lentulo is what carries the paste into the RCS.
Both techniques are more attractive in theory than in fact. Neither technique has demonstrated an ability to seal effectively over time or to completely obturate the RCS.
Moreover, because of a lack of predictable length control, both injection and placement by Lentulo spiral drill have major deficiencies and are not recommended.
Advantages and Disadvantages of Pastes
The advantages of pastes are speed, relative ease of use, and use of a single material. The equipment needed, at least with the Lentulo spiral technique, is relatively simple, comprising only a limited assortment of special drills.
The disadvantages are lack of predictability and lack of consistent length control. Also, it is difficult to avoid overextension or underfill ( Fig. 18.6 ). Another major disadvantage is inconsistent sealability. This may be related to three factors: (1) large voids or discrepancies within the material or adjacent to the walls; (2) shrinkage of ZnOE on setting, which leaves space for microleakage; and (3) solubility of pastes in tissue or oral fluids.
Sealers
Sealer, as an adjunct, accomplishes the objective of creating a watertight seal. Sealer must be used in conjunction with the primary obturating material, regardless of the technique or material used. This makes the physical properties and placement of the sealer important.
Desirable Properties
Grossman outlined the criteria for an ideal sealer, which are presented in the following list. None of the sealers currently available has all these ideal properties, but some have more than others.
- ▪
Tissue tolerance. The sealer and its components should cause neither tissue destruction nor cell death. All commonly used sealers show some degree of toxicity. This toxicity is greatest when the sealer is unset but tends to diminish after setting and with time.
- ▪
No shrinkage with setting. The sealer should remain dimensionally stable or even expand slightly on setting.
- ▪
Slow setting time. The sealer should provide adequate working time for placement and manipulation of obturating material, then set reasonably soon after obturation is complete. It is desirable to have sealer unset if post space is made immediately.
- ▪
Adhesiveness. A truly adhesive material forms a tight bond between the core material and dentin.
- ▪
Radiopacity. Sealer should be readily visible on radiographs so the operator knows where it is located both within the RCS and in the periapex when overextended. However, sealer should not be more radiopaque then core material because it would mask voids and obturation imperfections.
- ▪
Absence of staining. Remnants should not stain dentin or enamel. Currently, all tested sealers, particularly ZnOE-based sealers or those containing heavy metals, stain dentin to a greater or lesser degree.
- ▪
Solubility in solvent. Occasionally, creation of post space or retreatment may be necessary days, months, or years after obturation. The sealer should be soluble in a solvent. Different sealers have different degrees of solubility in different solvents and with varying mechanical techniques.
- ▪
Insolubility to oral and tissue fluids. Sealer should not resorb when in contact with tissue fluids. However, all sealers are soluble to a greater or lesser extent when in contact with oral fluids.
- ▪
Bacteriostatic properties. Although a bactericidal sealer would seem to be desirable, a substance that kills bacteria could also be toxic to host tissues. At minimum, the sealer should not encourage bacterial growth.
- ▪
Ability to create a seal. This is obviously an important physical property. The material must create and maintain a watertight seal apically, laterally, and coronally.
Types
In general, the four major types of sealers are ZnOE-based, plastics, glass ionomer, and those containing calcium hydroxide. Other variations and compounds have been proposed or are marketed as sealers; these should be considered experimental.
Certainly, the standard sealer with which all others are compared is the Grossman formulation, which has withstood the test of time and use, although some plastics (resins) are now widely used and have many desirable properties. Calcium hydroxide and glass ionomer types are newer and have interesting properties but also significant drawbacks.
ZnOE-Based Sealers
The major advantage of ZnOE-based sealers is their long history of successful use. Obviously, their positive qualities outweigh their negative aspects (staining, a very slow setting time, nonadhesion, and solubility).
Grossman’s Formulation
Grossman’s formula is as follows:
-
Powder: Zinc oxide (body), 42 parts; staybelite resin (setting time and consistency), 27 parts; bismuth subcarbonate, 15 parts; barium sulfate (radiopacity), 15 parts; sodium borate, 1 part.
-
Liquid: Eugenol
Most ZnOE sealers in use today are variations of this original formula. Three problems with this formulation are its very slow setting time, toxic effects on host tissue, and lack of adhesiveness.
Epoxy Resin
Epoxy has traditionally been available in a powder-liquid formula (AH26, AH Plus, and ThermaSeal Plus). Its advantages include antimicrobial action, adhesion, a long working time, ease of mixing, and very good sealability. Its disadvantages are staining, relative insolubility in solvents, some toxicity when unset, and some solubility to oral fluids. There are newer formulations without hexamine tetramine, which has been implicated in postobturation sensitivity. This formulation is also easier to mix because it is composed of two pastes mixed equally.
Other Plastics
Other plastics are primarily of the methylmethacrylate type and are not commonly used.
Calcium Hydroxide
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


