Respiratory compromise in patients with congenital craniofacial anomalies is usually secondary to retrognathia and the resultant glossoptosis of the tongue base. Severe airway obstruction, termed obstructive sleep apnea (OSA) or sleep disorder breathing (SDB), is associated with significant morbidity and mortality in infants and children. They exhibit frequent episodes of oxygen desaturation, hypoxemia, acidosis, inspiratory stridor, sternal retraction, and poor feeding. Infants and children with long-term airway obstruction exhibit failure to thrive, daytime somnolence, hemodynamic changes (including cor pulmonale and pulmonary hypertension), developmental disabilities, insufficient weight gain, malnutrition, increased pulmonary morbidity, and death.
Numerous modalities have been used to treat obstructive sleep apnea, including prone positioning, nasopharyngeal airways, tongue-lip adhesion, mandibular distraction, and tracheostomy. Mandibular distraction has proven to be an effective method for airway management in children. Its application relieves the source of obstruction and eliminates the risks of delayed speech, feeding difficulties, mucus plugging, and tracheomalacia associated with tracheostomy. In a relatively short time, the family is able to care for an affected child at home without the aid of monitors, nasal tubes, or frequent repositioning.
Etiopathogenesis
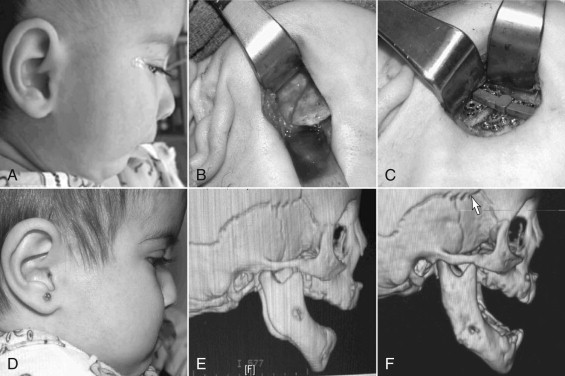
Patients with congenital retrognathia and glossoptosis, with or without cleft palate, are diagnosed with Pierre Robin sequence ( Fig. 115-1 ). This group represents the majority of children who may benefit from mandibular distraction. Additional findings of ocular abnormalities and one of several defined mutations in collagen production lead to the diagnosis of Stickler syndrome. Children with mandibulofacial dysostosis disorders such as Treacher Collins syndrome, Nager syndrome, and bilateral hemifacial microsomia often suffer from obstructive apnea and may also benefit from mandibular distraction.
Pathologic Anatomy
Common to the syndromes just discussed is the presence of hypoplasia of the mandible. Mandibular retrognathia, with or without the presence of micrognathia, positions the base of the tongue posteriorly, resulting in glossoptosis. On physical examination, significant mandibular-maxillary discrepancy is noted, as measured from the apex of the mandibular alveolar ridge and the apex of the maxillary alveolar ridge in the midline, and is especially pronounced when the patient is supine, with the force of gravity acting on it, or while feeding. The tongue base abuts the posterior pharyngeal wall. The result is an infant with labored, noisy breathing, rapid development of fatigue, and costal retractions. Surgical techniques such as glossopexy or tongue-lip adhesion, that position the tongue forward, are often criticized in that only the soft tissue is addressed and not the underlying skeletal problem.
Pathologic Anatomy
Common to the syndromes just discussed is the presence of hypoplasia of the mandible. Mandibular retrognathia, with or without the presence of micrognathia, positions the base of the tongue posteriorly, resulting in glossoptosis. On physical examination, significant mandibular-maxillary discrepancy is noted, as measured from the apex of the mandibular alveolar ridge and the apex of the maxillary alveolar ridge in the midline, and is especially pronounced when the patient is supine, with the force of gravity acting on it, or while feeding. The tongue base abuts the posterior pharyngeal wall. The result is an infant with labored, noisy breathing, rapid development of fatigue, and costal retractions. Surgical techniques such as glossopexy or tongue-lip adhesion, that position the tongue forward, are often criticized in that only the soft tissue is addressed and not the underlying skeletal problem.
Diagnostic Studies
Evaluation of mandibular retrognathia includes a polysomnogram, pH probe study or modified barium swallow, laryngoscopy, and maxillofacial CT scan.
The polysomnogram, performed in the supine position, records central apneas, obstructive apneas, and hypopneas. Central apneas are characterized by an absence or decrease in respiratory effort. In contrast, obstructive episodes are associated with an increased respiratory effort while airflow decreases. Hypopnea refers to a decrease in airflow by 30% to 50% from baseline. It is important to exclude central apnea as a cause of respiratory distress, as this neurologic condition will not benefit from skeletal advancement. Normal values of the calculated apnea-hypopnea index (AHI) in children are different from those of adults. Studies of normal children have suggested that an AHI greater than 1 is abnormal, with AHI 1 to 4 classified as mild OSA; AHI 5 to 10, moderate OSA; and AHI greater than 10, severe OSA. Cohen and colleagues demonstrated an improvement of mean AHI from 25.24 to 1.72 following mandibular distraction.
The polysomnogram also provides data on sleep architecture. Obstructive events may worsen during rapid eye movement (REM) sleep as muscle tone decreases. The result is frequent awakenings and less time spent in REM sleep. In growing children, the result may be decreased secretion of growth hormone and other chemical signals released during REM sleep, which can contribute to developmental delays.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


