Surgery for obstructive sleep apnea (OSA) is indicated when applicable conservative therapies are unsuccessful or intolerable and for patients with an underlying specific surgically correctable abnormality that is causing the OSA. It can provide definitive treatment and, thus, eliminate issues of patient compliance with other therapies, but only if performed competently, both in terms of technical skill and on the correctly identified area(s) of upper airway (UA) obstruction.
Maxillomandibular advancement (MMA) with adjunctive extrapharyngeal procedures is the most effective acceptable (excludes tracheostomy) surgical treatment of OSA, with a therapeutic efficacy equal to nasal continuous positive airway pressure (nCPAP). Like nCPAP that pneumatically splints open the UA, MMA “pulls forward” the anterior pharyngeal tissues (e.g., soft palate and tongue) attached to the maxilla, mandible, and hyoid to structurally enlarge the entire velo-orohypopharyngeal airway; and enhance the neuromuscular tone of the pharyngeal dilator musculature (e.g., tensor veli palatini and genioglossus), via an extrapharyngeal operation with minimal risks of postoperative edema-induced UA embarrassment or pharyngeal dysfunction.
Etiopathogenesis
OSA is part of a continuum of sleep-related breathing disorders (SBD) that also includes snoring and upper airway resistance syndrome, which results from repetitive collapse or obstruction of the UA during sleep that is caused by a complex array of physiologic and anatomic abnormalities. Snoring is the “warning bell” of partial or impending airway collapse, whereas OSA occurs with a complete airway obstruction lasting longer than 10 seconds. Resultant reduced oxyhemoglobin levels to the brain, heart, and other vital organs can lead to a myriad of signs and symptoms, including daytime hypersomnolence, memory loss, morning headaches, irritability, depression, decreased libido, and impaired concentration. Left untreated, OSA can cause hypertension, stroke, cardiovascular dysrhythmias, myocardial infarction, and sudden death while asleep.
OSA is a very common but potentially life-threatening medical disorder. An estimated prevalence of SBD is 24% and 9% of adult males and females, respectively, and an estimated 50 to 70 million Americans suffer from chronic sleep disorders. Daytime sleepiness alone costs $150 billion annually in lost productivity and mishaps, and another $48 billion in medical costs related to motor vehicle accidents that involve drowsy drivers; 20% of all serious car crashes are associated with daytime hypersomnolence, independent of alcohol. Factors that can precipitate or exacerbate OSA include advancing age, weight gain, sedative-hypnotic medications and alcoholic beverages within 2 hours of sleep, and supine sleep.
Pathologic Anatomy
Disproportionate UA anatomy in OSA may include specific structures or multiple sites or areas that can be diffusely complex, which varies between different patients. OSA surgical procedures can be classified anatomically as intrapharyngeal or extrapharyngeal. Intrapharyngeal procedures are performed on soft tissues that compose or lie within the velo-orohypopharyngeal airway wall or lumen, whereas extrapharyngeal surgery involves skeletal structures that lie outside the UA. Common intrapharyngeal sites include an elongated or retropositioned soft palate in the velopharynx, and hypertrophied tonsils and macroglossia or a retropositioned tongue base in the orohypopharynx. Hypoplastic or retropositioned extrapharyngeal lower facial skeletal structures, including the maxilla, mandible, and hyoid, may also be causative of OSA because they support or stabilize these velo-orohypopharyngeal soft tissues. In contrast to extrapharyngeal surgery, intrapharyngeal procedures can produce life-threatening UA edema in the immediate postoperative period and are often subtherapeutic because they address isolated sites or limited areas of an often diffusely complex, narrowed velo-orohypopharyngeal airway.
Pathologic Anatomy
Disproportionate UA anatomy in OSA may include specific structures or multiple sites or areas that can be diffusely complex, which varies between different patients. OSA surgical procedures can be classified anatomically as intrapharyngeal or extrapharyngeal. Intrapharyngeal procedures are performed on soft tissues that compose or lie within the velo-orohypopharyngeal airway wall or lumen, whereas extrapharyngeal surgery involves skeletal structures that lie outside the UA. Common intrapharyngeal sites include an elongated or retropositioned soft palate in the velopharynx, and hypertrophied tonsils and macroglossia or a retropositioned tongue base in the orohypopharynx. Hypoplastic or retropositioned extrapharyngeal lower facial skeletal structures, including the maxilla, mandible, and hyoid, may also be causative of OSA because they support or stabilize these velo-orohypopharyngeal soft tissues. In contrast to extrapharyngeal surgery, intrapharyngeal procedures can produce life-threatening UA edema in the immediate postoperative period and are often subtherapeutic because they address isolated sites or limited areas of an often diffusely complex, narrowed velo-orohypopharyngeal airway.
Diagnostic Studies
Polysomnography
OSA, as well as other SBD, is diagnosed by overnight polysomnography (PSG), which is a sleep study usually performed in a sleep laboratory. Multiple physiologic parameters are recorded to establish the diagnosis and quantitate severity. An apnea-hypopnea index (AHI) greater than 10 (events per hour of sleep), an apnea index (AI) greater than 5, and a lowest arterial oxyhemoglobin saturation (LSAT) less than 90% are pathologic. PSG is also performed to assess the therapeutic efficacy of OSA treatments, which include nCPAP, oral appliances, weight loss, positional therapy, and surgery.
Cephalometric Analysis
Clinical examination alone is inadequate to evaluate the UA. In comparison with other reputable diagnostic modalities (e.g., nasopharyngolaryngoscopy, intraluminal pressure transducers, somnofluoroscopy, computed tomography scans, and magnetic resonance imaging), lateral cephalometry (though limited to a static, lateral, two-dimensional view of the head and neck in awake erect patients), is comfortably noninvasive, safe with minimal radiation exposure, easy to perform in an outpatient setting, and inexpensive. It produces results that are objective, standardized, and reproducible, and therefore has been utilized extensively in the OSA literature.
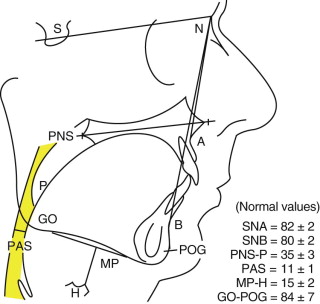
If cephalometry ( Fig. 114-1 ) is to be employed for diagnostic imaging of the UA in OSA patients, two modifications are recommended. First, because pharyngeal volume fluctuates with phases of respiration, cephalometry should be standardized by obtaining films at both end-tidal volume (ETV) and during a modified Mueller maneuver (forced inspiration against a closed mouth and nose, to simulate UA collapse associated with negative inspiratory forces generated during OSA events). Second, because the most critical site of orohypopharyngeal closure may vary, the cephalometric posterior airway space (PAS) should be measured at the narrowest level of hypopharyngeal collapse, rather than a level determined by skeletal landmarks.
Oral Appliances as Predictors of Mandibular Advancement
It is difficult to predict therapeutic efficacy of any surgical treatment for OSA. However, unlike the maxilla, the mandible can be reversibly protruded and the UA imaged (e.g., with lateral cephalometry) to view and measure velo-orohypopharyngeal enlargement. Custom-fabricated oral appliances worn during sleep can be tested with overnight PSG to document therapeutic efficacy of mandibular advancement for OSA. If mandibular advancement appliances are subtherapeutic (e.g., because there are multiple sites of UA narrowing or severe orohypopharyngeal narrowing not fully relieved by sole mandibular advancement due to limitations of temporomandibular joint condylar translation), or therapeutic but intolerable with required nightly use, then MMA might be a reasonable alternative. Although oral appliances are generally therapeutic for mild to moderate OSA, MMA may be necessary for more severe OSA and for those who cannot tolerate wearing devices while asleep.
Treatment Goals
All OSA surgery should (strive to) accomplish the following general goals : be safe, with minimal morbidity; cause minimal pain, disfigurement, and dysfunction; be therapeutic; be cost-effective; and be comprehensive, ideally addressing all sites of UA obstruction in one operation ( Box 114-1 ).
- •
Safe with minimal morbidity (“first do no harm”)
- •
Minimal pain, disfigurement, and dysfunction
- •
Therapeutic, immediate, and long-term
- •
Cost-effective
- •
Comprehensive, ideally addressing all sites of obstruction in one operation
Patients may be evaluated for OSA surgery when four prerequisites are satisfied. First, they exhibit OSA diagnosed by PSG (inclusion criteria of an AHI greater than 15 or an AI greater than 5 and an LSAT less than 90%) that is clinically significant (inclusion criterion of excessive daytime sleepiness). Second, all applicable conservative therapies (e.g., nCPAP, weight loss, positional therapy, reduction of late evening sedative-hypnotic medications or alcoholic beverages, oral appliances or other devices) have been unsuccessful or intolerable. Third, they are medically and psychologically stable, and, fourth, are willing to proceed with surgery ( Box 114-2 ).
Surgical Prerequisites
- 1
Clinically significant OSA (AHI >15 or AI >5, LSAT <90%, and EDS)
- 2
Conservative treatments (e.g., CPAP) nonapplicable/unsuccessful/ intolerable
- 3
Medically/psychologically stable
- 4
Willing to proceed with surgery (i.e., informed consent)
For Specific Site(s)/Segmental Area(s) that are Distinctly Identifiable
- 1
Treat with appropriate procedures that address these specific sites
- 2
If a staged approach is recommended/desired, treat the most severe/critical site/area first
For Diffusely Complex or Multiple Sites that are not Readily Distinguishable
- 1
Extrapharyngeal skeletal advancement procedures first to enlarge/stabilize pharyngeal airway
- a
Primary single-stage definitive treatment; or
- b
Minimize risk of postoperative edema-induced airway embarrassment associated with subsequent intrapharyngeal surgery
- a
- 2
Intrapharyngeal soft-tissue procedures second, if still necessary, for clinically significant residual OSA
The selection of surgical procedures should not be market driven or specialty- or stage-specific; rather, selection should be “site-specific,” based on each patient’s specific sites of UA obstruction. For specific sites or segmental areas that are distinctly identifiable, treat with appropriate procedures that address these specific sites or areas. If a staged approach is recommended and desired, treat the most severe or critical site or area first. For those patients with diffusely complex or multiple sites or areas that are not easily identified, extrapharyngeal skeletal advancement procedures (e.g., MMA) may be performed initially (see Box 114-2 ).
(NOTE: Parameters used by different authors to measure OSA surgical “success” vary in the literature. The primary inclusion criterion for the case series in Tables 114-1 to 114-3 and Figure 114-6 is reported preoperative and postoperative AHI or occasionally the respiratory disturbance index (RDI), which are used synonymously though slight differences currently exist. The reader is referred to the source documents, because these definitions have varied over time. Unless otherwise stated, “success” is generally defined as a postoperative AHI less than 20 and/or greater than 50% reduction in AHI. To standardize results of the AHI data, the primary outcome measure for comparison of surgical procedures is the mean percentage (%) reduction in AHI [from preoperative to postoperative].)
Surgical Treatment and MMA Techniques
Telegnathic Surgery
Although the surgical techniques are similar, the treatment goals and criteria for success differ for MMA as telegnathic (derived from the Greek words tele, which means “over a distance,” and gnathis, which relates to the jaws) surgery versus orthognathic (derived from the Greek words ortho, which means “to straighten,” and gnathis ) surgery. Whereas orthognathic surgery includes maxillary and mandibular osteotomies to treat malocclusion to improve mastication, speech, and esthetics, telegnathic surgery includes skeletal (i.e., maxillary, mandibular, and hyoid) advancement to anatomically enlarge and physiologically stabilize the pharyngeal airway to treat OSA. Ideally, MMA may harmoniously satisfy the goals and be successful as both orthognathic and telegnathic surgery. However, this may not always be feasible. Accordingly it should not be viewed as failure, but rather, accepted as known limitations of this type of surgery.
For example, telegnathic MMA may be therapeutic for OSA, but yet maintain an existing, albeit “untreated,” malocclusion in a patient who elects not to pursue concomitant orthodontic therapy. On the other hand, orthognathic mandibular setback surgery to successfully treat a Class III malocclusion might create hypopharyngeal narrowing and frank OSA. Another case scenario is sole mandibular advancement to correct a Class II malocclusion, but yet is subtherapeutic for existing OSA in that maxillary advancement was also required to enlarge and stabilize the entire velo-orohypopharyngeal airway.
In addition to malocclusion, other dental problems such as severe periodontal disease or compromised fixed bridgework may be relative contraindications for elective orthognathic surgery, but yet not (contraindications) for telegnathic surgery to treat the potentially life-threatening medical disorder of OSA. In cases of hypopharyngeal narrowing in the absence of skeletal hypoplasia (i.e., a normal profile), MMA might create an unesthetic facial appearance in terms of bimaxillary protrusion with alar base flaring and nasal tip rotation.
Unlike the relatively healthy and younger orthognathic patient, the typical OSA patient (who finally presents for telegnathic MMA after years of failed prior therapies) has a health status that is often compromised by morbid obesity, hypertension, and other medical problems, as well as depression and cognitive dysfunction. Hence, the perioperative management is often more intensive, and the associated risks higher, for telegnathic (versus orthognathic) surgery.
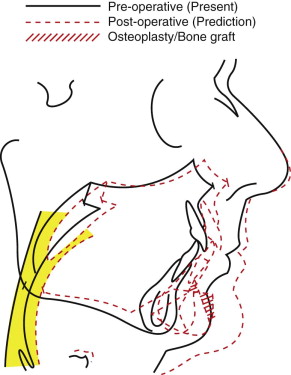
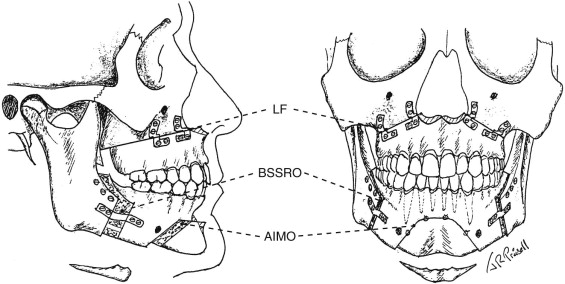
Surgical Principles and Management
Telegnathic MMA ( Figs. 114-2 and 114-3 ) is a technically tedious and difficult operation that is best performed under hypotensive anesthesia (to control blood loss) in a hospital operating room with both a surgeon and assistant surgeon. Bilateral sagittal split ramus osteotomies (BSSRO) with rigid internal and/or maxillomandibular fixation (MMF) are performed for mandibular advancement. A Le Fort I osteotomy (LF) with bone graft and rigid internal fixation (RIF) is performed for maxillary advancement to anterosuperiorly reposition and stabilize the attached soft palate for velopharyngeal enlargement (thereby perhaps eliminating invasive soft palatal surgery), and to maintain a functional occlusal relationship with the synchronously advanced mandibular dentition (thereby preserving the functions of mastication and speech articulation).
The soft palate is a tissue organ whose known primary function is to prevent reflux of air and liquids into the nasopharynx during speech and swallowing, respectively. Also, its role in snoring may be a self-protection warning sign, or “bell” (to the bed partner), of partial or impending UA obstruction, which may progress to OSA. A dysmorphic or abnormal-looking soft palate may be an anatomic variant of normal that ensures compensatory functioning and, therefore, may not always be a cause of OSA. Retropalatal narrowing and collapse, often induced by swallowing (e.g., during nasopharyngolaryngoscopy), should be understood as normal velopharyngeal closure, rather than perhaps misinterpreted as a site of obstruction dictating surgery. Surgical ablation or distortion may produce dysfunction, such as velopharyngeal insufficiency (VPI); velopharyngeal stenosis; voice changes; dysphagia; and, in cases of “social” snoring amelioration, may produce “silent” apnea—either of immediate or delayed (with advancing age and/or weight gain) onset. In addition, pain, hemorrhage, and UA obstruction in the immediate postoperative period may occur because of velopharyngeal edema which, particularly if compounded with coexisting untreated hypopharyngeal narrowing, can result in death.
MMA preserves the functional integrity of the pharyngeal tissues. Edema from the intraoral labial vestibular MMA incisions is anatomically shielded from the UA by the underlying bony structures and, thus, is confined to the facial soft tissues. Although this extraosseous edema may produce a frightfully swollen face, it does not typically extend to the UA. The entire velo-orohypopharyngeal airway is more patent at the moment of skeletal advancement, (i.e., like the immediate UA opening produced by a CPR “jaw-thrust” maneuver). Hence, early endotracheal tube (ETT) extubation is encouraged (serving to minimize ETT-induced glottic edema) and usually accomplished in the operating room at the conclusion of the operation. Centrally acting opiate and opioid narcotics (which can cause respiratory depression and therefore are to be used judiciously) may not be necessary because, first of all, rigidly fixated MMA bony segments (unlike operated pharyngeal soft tissues) do not move and accordingly are not painful during swallowing, coughing, and vocalization; and second, trigeminal (sensory) nerve branches encased within bony canals are usually surgically traumatized, resulting in numbness rather than severe pain.
Counterclockwise Rotational Advancement
The amount of mandibular advancement is usually the main determinant of the therapeutic efficacy of MMA for OSA, because the most critical site of UA obstruction is usually hypopharyngeal. (The hypopharynx is the common “bottleneck” from the nasal and oral inspiratory pathways.) However, the limiting factor for the amount of MMA advancement is the degree of maxillary protrusion, which thins the upper lip and results in excessive maxillary incisor show, alar base flaring (even with compensatory nasal base cinch sutures and V – Y advancement closure of the vestibular tissues), and upward nasal tip rotation. Hence, the LF is usually performed before the BSSROs. Osteoplasty of the anterior nasal spine minimizes excessive nasal tip rotation. The piriform rims are enlarged, the caudal edge of the nasal septum relieved, and the inferior turbinates outfractured to minimize iatrogenic nasal obstruction. The amount of anterior maxillary impaction is determined by the degree of maxillary incisor show with lips in repose. Resultant telescoping of the inferior over the superior edges of the osteotomized anterior maxillary walls provides a trough for placement of corticocancellous bone, which prevents soft tissue ingress and promotes a uniform and stable bony union.
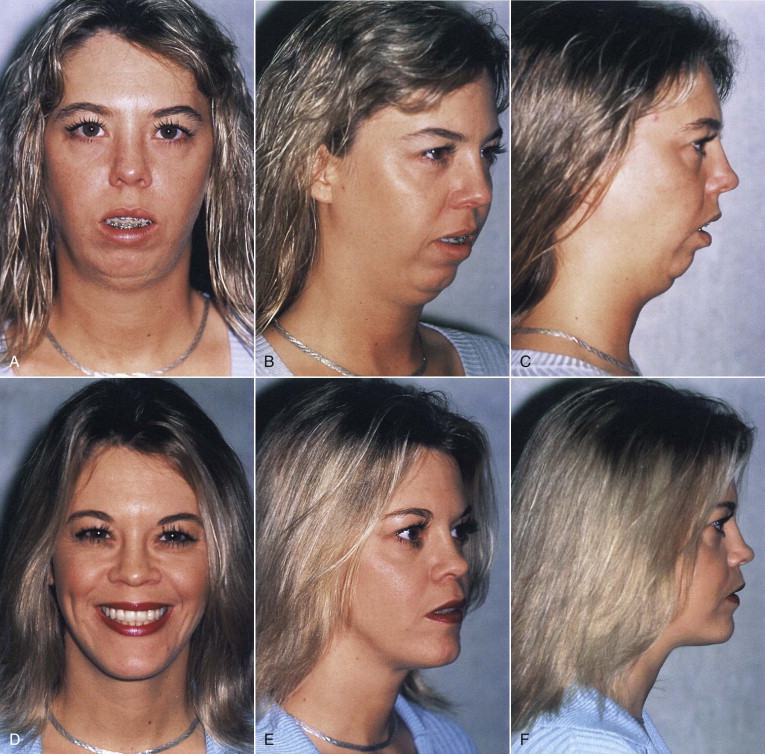
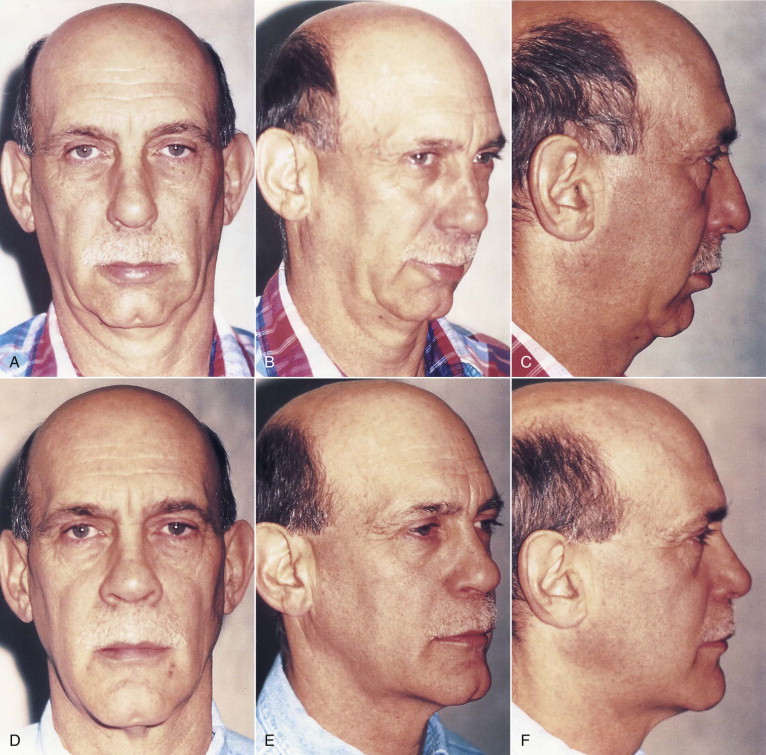
Counterclockwise rotation of the maxillomandibular complex allows for maximum mandibular advancement to enlarge the hypopharynx for therapeutic efficacy while minimizing the unesthetic affects of excessive maxillary advancement. Other esthetic enhancements of counterclockwise rotational advancement include elimination of excessive maxillary incisal show at rest or gummy smile and lip incompetence in dolichocephalic facies, increased horizontal and vertical dimension of the lower face with accentuation of the lower jawline and hyoid elevation that raises the chin–neck angle in mandibular retrognathism cases ( Fig. 114-4 ), and tightening or rejuvenation of neck skin laxity in relatively older patients ( Fig. 114-5 ).
Prevention of Skeletal and Airway Relapse
Counterclockwise rotation with anterior maxillary impaction allows for greater mandibular advancement. For example, the resultant mandibular advancement following 6 mm maxillary advancement and 3 mm anterior impaction might be 15 mm. Posteroinferiorly directed forces from the intact tongue-related (e.g., genioglossus) and suprahyoid (e.g., geniohyoid and anterior digastric) musculature on the distal mandibular osteotomy segments may cause skeletal instability and relapse. In contrast to conventional orthognathic surgery, it is critical that anteroinferior mandibular myotomies not be performed in telegnathic MMA, because intact tongue-related and suprahyoid musculature is necessary for orohypopharyngeal enlargement to treat OSA. However, release of the deep tendons of the temporalis and masseteric sling at the inferior border and vertical scoring of the inelastic periosteum lateral to the BSSROs facilitates this counterclockwise rotational advancement.
To minimize skeletal and attached anterior pharyngeal tissue relapse, RIF must be reinforced, for example, with bicortical screws and unicortical bone plates at the superior and inferior borders, respectively, of BSSROs (see Fig. 114-3 ). Corticocancellous block bone grafts wedged between all osteotomy advancement “gaps” will minimize soft tissue ingress and, thus, promote more uniform and esthetic bony unions. Temporary MMF with anteriorly directed elastic ligatures around orthodontic appliances or arch bars facilitates advancement and stability of the distal mandibular segment for RIF placement. Dental implants may facilitate MMF in cases of periodontally unstable dentitions and partial or complete edentulism. Once healed to a bony union, the advanced maxillomandibular complex is stable, with an expanded velo-orohypopharyngeal airway in all three dimensions.
Anterior Inferior Mandibular Osteotomy
An extrapharyngeal anterior inferior mandibular osteotomy (AIMO) produces additional advancement of the tongue-related and suprahyoid musculature (an indirect hyoid suspension) for additional enlargement and stabilization of the orohypopharyngeal airway. It is critical that the height, width, and thickness of the distal segment be large enough to include all muscle insertions that may extend beyond the genial tubercles superiorly, laterally, and inferiorly. In contrast to AIMO, a sliding genioplasty made with a single horizontal cut may be too low, and a rectangular pull-through “window” segment that does not include the inferior border may be too small, respectively, to capture all of the muscle insertions, and a 90-degree torsion of this distal segment (for structural stabilization) may precipitate tendon rupture or necrosis and detachment of this soft tissue pedicle.
A wide inferiorly based trapezoid-shaped AIMO should extend to within 5 mm of the teeth apices, at least 10 mm anterior to the mental foramina, and include the inferior mandibular border. The distal segment is advanced the full bicortical thickness and stabilized by overlapping the superior edge of the lingual cortex anterior to the buccal cortex of the proximal (tooth-bearing) segment before placement of RIF. Aggressive osteoplasty of the distal segment’s buccal cortex will allow a tension-free vestibular closure, as well as reshape an otherwise unesthetic prognathic chin. Corticocancellous bone grafting will minimize soft tissue ingress, promote a more uniform bony union, and lessen an otherwise unesthetic deep mentolabial fold (see Figs. 114-2, 114-3, 114-4, and 114-5 ).
Distraction Osteogenesis
Although used extensively for transverse maxillary expansion in children and adults, and reported in the pediatric literature for single-jaw (e.g., mandibular and midfacial) and, less commonly, staged two-jaw lengthening, the potential application of distraction osteogenesis (DO) for simultaneous maxillary and mandibular advancement for OSA is challenging and promising.
Telegnathic surgery utilizing DO offers three advantages over conventional osteotomies. First, DO may be performed before skeletal maturation to treat OSA in younger patients (e.g., children and infants). Second, DO allows greater advancement of hard and accompanying soft tissues to treat more severe cases of skeletal hypoplasia, including craniofacial syndromes and/or soft tissue inelasticity. The surgical technique involves less tissue dissection, and bone grafting is not needed. The gradual soft tissue accommodation associated with incremental skeletal advancement may improve skeletal stability in terms of minimizing skeletal relapse due to muscle tension or soft tissue inelasticity. Third, the amount of jaw advancement may be titrated to optimal therapeutic positioning, as confirmed by serial PSG, analogous to the titration of nCPAP and oral appliance therapy.
On the other hand, telegnathic surgery utilizing DO has three disadvantages, in comparison with conventional osteotomies. First, patients may be intolerant of the extraosseous fixation devices and noncompliant with the required multiple office visits for serial adjustments of these devices. Second, inherent difficulties with parallel alignment of distraction devices and subsequent coordination of vectors of skeletal advancement, particularly in bimaxillary cases, may result in higher incidences of malocclusion and facial asymmetry. Third, financial costs of the hardware, additional surgery (e.g., for hardware removal), and labor intensive postoperative care are higher than conventional osteotomies. These limitations should lessen with technical improvements (e.g., miniaturized and bioresorble distraction devices) and refined clinical expertise. The indications for telegnathic DO will become more clearly defined with additional scientific studies.
Surgical Staging with Unilevel and Multilevel Operations
Although MMA is known to be highly therapeutic for OSA, its indications and staging protocols remain unsettled. This is partly because of existing diagnostic dilemmas such as: identifying and ranking (in terms of severity) the often diffusely complex or multiple sites of obstruction; and knowing when and how to prioritize and combine the numerous available surgical procedures in one or more stages, which may be influenced (and perhaps biased) by the surgeon’s education, training, and experience. One approach is to perform certain procedures stepwise according to a methodical sequential (staging) protocol, such as uvulopalatopharyngoplasty (UPPP) and other procedures first; then, if unsuccessful, an MMA. However, this may result in unnecessary additional intrapharyngeal surgery with potentially life-threatening UA edema that may be painful, dysfunctional, expensive, subtherapeutic, and ultimately a deterrent for patients to seek definitive surgical treatment. (Note: “Phase” and “stage” are synonymous and thus are used interchangeably.)
In general, multilevel (surgical procedures performed concomitantly to address multiple levels of UA narrowing) and unilevel (surgery to address single levels of UA narrowing) operations are less therapeutic than MMA. Riley et al reported a success rate of 60% (145 of 239 cases) and only 42% (44 of 104 cases with severe OSA) for phase I surgery, which consisted of UPPP and/or genioglossus advancement with hyoid myotomy (GAHM) suspension in the largest multilevel series. Sher et al reported 41% success (137 of 337 cases from 37 series) of UPPP, which is the most commonly performed OSA surgery. Elshaug et al reported success rates of 52% (92 of 178 cases from 7 subsequent series) for UPPP, 49% (35 of 72 cases from 3 series) for laser-assisted uvuloplasty (LAUP), and 61% (22 of 36 cases from 2 series) for radiofrequency (RF) tissue reduction. Kezirian et al reported that many hypopharyngeal procedures are also relatively subtherapeutic, including 62% success (56 of 91 cases from 4 series) of GA, 55% success (180 of 328 cases from 5 series) of GAHM, 35% success (95 of 269 cases from 11 series) of RF tongue base (RFTB), 35% success (27 of 77 cases from 6 series) of tongue base suspension (TBS) via a bone screw–anchored sling stitch; 50% success (37 of 74 cases from 5 series) of midline glossectomy (MLG); and 50% success (51 of 101 cases from 4 series) of hyothyroidopexy (HSThy).
In general, most patients do not pursue additional (i.e., staged) OSA surgery, despite the knowledge that MMA is highly therapeutic. Riley et al reported that only 26% (24 of 94) of their stage I (UPPP and/or GAHM) failures, Bettega et al reported that only 38% (13 of 34) of their stage I (UPPP, tonsillectomy [Tons], HSThy, and GA or inferior sagittal osteotomy [ISO]) failures, and Lee et al reported that only 27% (3 of 11) of their stage I (UPPP and ISO or AIMO) failures, proceeded to stage II (MMA). None of the 9 and 18 multilevel surgical failures from Dattilo et al (UPPP, LAUP, or uvulopalatal flap; hyoid suspension [HS], GA, and Tons) and Hendler et al (UPPP and anterior mandibular osteotomy [AMO]) participated in their respective MMA series.
Primary and Secondary Mma
Fifteen MMA case series (inclusion criterion of more than 5 cases) performed in adult OSA patients (pediatric and DO cases were excluded) are listed in Table 114-1 . Eleven “primary” MMA series were performed initially as a definitive (single-staged) operation ; and four “secondary” (e.g., phase II) MMA series followed unilevel or multilevel (e.g., phase I) surgery as part of two-phase protocols. MMA was highly therapeutic with summary mean percent reductions in AHI of 86.5% (88.4% for case series with no concomitant intrapharyngeal, and 92.1% with extrapharyngeal procedures) for primary, and 86.6% for secondary MMA. Significantly, no additional stages of surgery were reported following any MMA series.
| REF # | PRIMARY AUTHOR YR | # CASES % SUCCESS (AHI <20) | ADJUNCTIVE PROCEDURES (IN ADDITION TO LF & BSSRO) | BMI (KG/M 2 ) | AGE (YR) | % MALE | AHI | % REDUCTIONS IN AHI | LSAT | # DAYS HOSPITAL | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PRE-OP | POST-OP | CPAP | SURG | CPAP | PRE-OP | POST-OP | CPAP | ||||||||
| Primary MMA | |||||||||||||||
| Hochban, 1997 | 37/38 = 97.4% (AHI <10) |
42.8 | 36 = 94.7 | 45.2 | 2.5 | 94.5 | |||||||||
| Dekiester, 2006 | 25 | ||||||||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


