Since the introduction of nonreusable, stainless steel dental local anesthetic needles, needle breakage has become an extremely rare complication of dental local anesthetic injections. But although rare, dental needle breakage can, and does, occur. Review of the literature and personal experience brings into focus several commonalities which, when avoided, can minimize the risk of needle breakage with the fragment being retained from occurring.
Local anesthesia forms the backbone of pain control techniques in dentistry. The injection of cocaine with epinephrine in 1885 by William Halsted enabled, for the first time, surgical procedures to be performed painlessly in a conscious human being. Before this the only option for pain-free surgery was general anesthesia, the controlled loss of consciousness, which does not prevent pain but simply prevents the patient from responding outwardly to it.
The basic local anesthetic armamentarium has, with very minor improvements, remained unchanged since Halsted’s time: a syringe, needle, and a vehicle for carrying the drug, today the glass (or in some countries, plastic) dental cartridge.
Syringes have undergone change from the original Pravez glass syringe (a traditional hypodermic syringe) in 1853 to the more modern breech-loading, metallic, and cartridge-type aspirating syringe devices presently used in dentistry. New computer-controlled local anesthetic delivery systems (C-CLAD) are becoming increasingly popular.
Cook-Waite Laboratories introduced the prefilled dental cartridge into dentistry in 1920, and trademarked the now commonly used name Carpule. Before its introduction, the dentist prepared his (the use of his is correct as the profession at that time was essentially entirely male) local anesthetics daily, using a mortar and pestle to pulverize a procaine tablet. Prefilled cartridges provided the doctor with a standardized formulation of a higher quality and greater sterility. The breech-loading cartridge-type aspirating syringe was developed to accommodate the cartridge.
Needles have also undergone change since their introduction. In the early to mid-1900s needles were reusable, being cleaned, sharpened and, hopefully, sterilized between patients. Stainless steel disposable needles were introduced into dentistry in the 1960s and remain the standard today.
The importance of local anesthesia to dentistry cannot be overstated. Local anesthetics represent the safest and the most effective drugs in all of medicine for the prevention and management of pain. Clinically adequate local anesthesia allows dental care to proceed safely in a pain-free environment and may represent the most important thing done for our patients to enable them to receive quality care. However it is the administration, actually the injection, of local anesthetics that represents the single most fear-inducing thing that dentists do to the patient during a typical dental visit.
Approximately 75% of medical emergencies reported in dentistry may be related to fear (stress). Of 30,608 emergencies reported by Malamed, 50.3% were syncope (fainting). Seeking to determine when during a dental appointment medical emergencies were most apt to occur Matsuura found that 54.9% of the reported emergencies occurred during or immediately after the local anesthetic injection. Quite simply, fainting during injections is the most common medical emergency seen in dentistry.
Trypanophobia (an irrational fear of procedures involving injections) is not uncommon amongst dental patients. Dentists have all had patients state: “Doctor, do you have to give me a shot to do this?” Or “Doctor, I hate getting shots but once I am numb I’m okay.” Or “Doctor, I just don’t want to see the needle.”
In 2004, De St Georges listed the factors considered by patients when evaluating their dentist. The top 2 factors were a dentist who does not hurt, (no. 2) and one who gives a painless injection. (no. 1).
Fearful dental patients, evaluating specific dental procedures, listed seeing the needle as more fear-inducing that feeling the needle. Asked specifically about which item(s) of the local anesthetic armamentarium (syringe, cartridge, needle) is most threatening, almost unanimously the response is the needle.
The local anesthetic needle
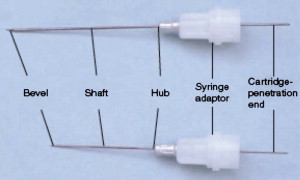
The dental local anesthetic needle should permit the deposition of a local anesthetic solution in close proximity to the targeted nerve and allow for successful aspiration to prevent intravascular injection of the drug. The needle itself is composed of 1 continuous length of stainless steel metal that starts at the needle tip ( Fig. 1 ) around which is placed a metal or plastic syringe adaptor and needle hub, exiting the opposite side as the portion of the needle that penetrates the diaphragm of the local anesthetic cartridge. The needle is firmly secured within its hub either by crimping of the metal hub against the needle or with glue (plastic hubbed needles). Needles have the following components in common: the bevel, the shaft (or shank), the hub, and the syringe-penetrating end ( Fig. 2 ).

The bevel defines the point or tip of the needle. Manufacturers describe bevels as long, medium, and short. The greater the angle of the bevel with the long axis of the needle, the greater is the degree of deflection as the needle passes through the soft tissues of the mouth ( Fig. 3 ). As the needle bevel is eccentric, the shaft of the needle is deflected as the needle advances through soft tissue toward the target zone for anesthetic deposition. This is most obvious in injection techniques such as inferior alveolar nerve block in which more soft tissue must be penetrated (between 20 and 25 mm in the average adult patient).
The shaft or shank of the needle is 1 long piece of tubular metal running from the tip of the needle through the hub and continuing as the piece that penetrates the cartridge. Two factors to consider regarding this component of the needle are the diameter of its lumen (eg, the needle gauge) and the length of the shaft from point to hub.
The hub is a plastic or metal piece through which the needle is attached to the syringe. The interior surface of the plastic and metal syringe adaptor of the needle is usually prethreaded allowing for its easy attachment to the syringe.
The syringe-penetrating end of the dental needle extends through the needle adaptor and perforates the diaphragm of the local anesthetic cartridge. Its tip lies within the cartridge.
Two factors must be considered when selecting needles for use in various injection techniques: length and gauge.
Needle Length
Needle length refers to the length of the needle shaft from the hub to the tip. Three needle lengths are used in dentistry: long, short, and extra short. Although there is some minor variation in length amongst needle manufacturers, in the United States a typical long dental needle is 32 mm, a short needle is 20 mm, and an extra short needle is 10 mm ( Table 1 ).
| Manufacturer | 25 g Long | 25 g Short | 27 g Long | 27 g Short | 30 g Long | 30 g Short | 30 g Extra Short |
|---|---|---|---|---|---|---|---|
| Industry Standard | 32 | 20 | 32 | 20 | |||
| 1 | 30 | 30 | 21 | 25 | 21 | ||
| 2 | 32 | 22 | 32 | 22 | 21 | 12 | |
| 3 | 32 | 21 | 25 | 21 | |||
| 4 | 35 | 35 | 25 | 25 | 10 | ||
| 5 | 32 | 21 | 19 |
A time-honored tenet of needle usage is: “Do not insert a needle into the soft tissues to its hub, unless absolutely necessary for the success of the injection.” The significance of this statement becomes evident later.
A short needle may be used for any injection in which the penetration depth of soft tissue to the deposition site of the local anesthetic solution is less than 20 mm. Long needles are recommended for deeper penetration.
Needle Gauge
Gauge refers to the diameter of the lumen of the needle; the smaller the number, the greater the diameter of the lumen. A 30-gauge needle has a smaller internal diameter than a 25-gauge needle. Industry standards for needle gauge are presented in Table 2 .
| Specifications for Needle Gauges | ||
|---|---|---|
| Gauge | Outer Diameter (mm) | Inner Diameter (mm) |
| 7 | 4.57 | 3.81 |
| 8 | 4.19 | 3.43 |
| 10 | 3.40 | 2.69 |
| 11 | 3.05 | 2.39 |
| 12 | 2.77 | 2.16 |
| 13 | 2.41 | 1.80 |
| 14 | 2.11 | 1.60 |
| 15 | 1.83 | 1.32 |
| 16 | 1.65 | 1.19 |
| 17 | 1.50 | 1.04 |
| 18 | 1.27 | 0.84 |
| 19 | 1.07 | 0.69 |
| 20 | 0.91 | 0.58 |
| 21 | 0.81 | 0.51 |
| 22 | 0.71 | 0.41 |
| 23 | 0.64 | 0.33 |
| 25 | 0.51 | 0.25 |
| 26 | 0.46 | 0.25 |
| 27 | 0.41 | 0.20 |
| 30 | 0.31 | 0.15 |
There is movement amongst dentists toward the use of smaller diameter needles on the assumption that they are less traumatic to the patient than larger diameter needles ( Table 3 ). Studies dating back to 1972 show this assumption to be unwarranted. Hamburg reported that patients are unable to differentiate among 23-, 25-, 27-, and 30-gauge needles. Fuller and colleagues reported no significant differences in perception of pain produced by 25-, 27- and 30-gauge needles during inferior alveolar nerve blocks in adults. Lehtinen compared 27- and 30-gauge needles and found that although insertion of the 30-gauge needle required significantly less force, the difference in pain perception was less remarkable.
| Gauge | Length | Data Provided by | |||
|---|---|---|---|---|---|
| Sullivan-Schein Inc. (2006) | Septodont Inc. (2006) | ||||
| 25 | Short | <1% | 1% | 0.6% | 3% |
| Long | 1% | 2.3% | |||
| 27 | Short | 10% | 42% | 13% | 38% |
| Long | 32% | 25% | |||
| 30 | Short | 50% | 56% | 51% | 59% |
| Extra short | 6% | 8% | |||
To avoid accidental intravascular injection, aspiration must be performed (preferably twice) before the deposition of any significant volume of local anesthetic. Trapp and Davies and Delgado-Molina and colleagues reported that no significant differences existed in ability to aspirate blood through 25-, 27- and 30-gauge dental needles. However, there is increased resistance to aspiration of blood through a thinner needle (eg, 30-gauge) compared with larger diameter needles (eg, 27- or 25-gauge).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


