Introduction
Mandibular lateral displacement (MLD) is clinically characterized by deviation of the chin, facial asymmetry, dental midline discrepancy, crossbite in the posterior region, and high prevalence of internal derangement of the temporomandibular joint. Morphologic and functional characteristics of MLD should be clarified to correct and prevent this malocclusion.
Methods
We examined the morphologic features, occlusal scheme, and functional behavior of MLD in 116 patients. Facial morphology was examined with posteroanterior cephalograms, occlusion guidance on the articulator after face-bow transfer, and condylar movement with the condylograph.
Results
The superiorly inclined occlusal plane was associated with mandibular deviation in the same direction. The posterior occlusal plane on the shifted side was significantly steeper than that on the nonshifted side. Functional analysis of condylar movement showed a close relationship between the direction of MLD and the direction of condylar lateral shift during opening and closing, and protrusion and retrusion. The occlusal guidance inclination in the buccal segment of the nonshifted side was steeper than that in the shifted side.
Conclusions
The results suggested that reduced vertical height of the dentition on 1 side induced mandibular lateral adaptation with contralateral condylar shift (asymmetry); this leads to condylar lateral shift during functional movement.
Mandibular lateral displacement (MLD) is relatively common in patients with malocclusion. The occurrence of MLD is of particular interest, since most types of malocclusion involve some facial asymmetry. MLD is characterized by mandibular deviation to 1 side evidenced by deviation of the chin from the facial midline, crossbite in the posterior region, and dental and skeletal midline discrepancies. It was also reported that MLD patients with facial asymmetry have internal derangement of the temporomandibular joint (TMJ). For the clinicians, MLD is a challenging anomaly and can sometimes be compromised in its results, because it is difficult to treat orthodontically, even with orthognathic surgery because of the asymmetry of the skeletal frame. This might be attributed to a lack of understanding of the morphologic and functional characteristics of this malocclusion.
In recent craniofacial biology research, the general consensus seems to be that the adaptation of skeletal and dentoalveolar elements of the face after functional displacement of the mandible leads to reestablishment of the structural and functional balance of the orofacial region. It was been suggested that the dentofacial complex is obviously adaptable to the functional demand in occlusal configuration and the change of occlusal function in growing facial bones. It was also pointed out by Petrovic and Stutzman that the cant of the maxillary occlusal plane is an important factor contributing to mandibular positioning.
As we reported earlier, the cant of the occlusal plane is closely associated with various dentoskeletal frames during craniofacial growth and development. It was speculated that horizontalization or flattening of the maxillary occlusal plane induces functional forward adaptation of the mandible followed by active transformation of the TMJs. Our previous investigation indicated that the cant of the frontal occlusal plane (OP) in MLD malocclusion tilted superiorly to the side to which the mandible was shifted, often with TMJ symptoms on the side with the shifted condyle. In this context, it must be considered that the vertical and transverse positions of the mandible associated with the vertical height of the posterior teeth (posterior vertical dimension) are important to understand MLD malocclusion, although the interrelationship among occlusal plane deviation, MLD, and functional disturbances still remains to be elucidated.
These previous findings led us to reevaluate MLD patients to consider a therapeutic functional approach based on occlusal plane control by reestablishing the appropriate occlusal vertical dimension on the affected side; this is an effective treatment for the correction of the facial asymmetry due to MLD, with consequent improvement of occlusal and articular functions.
In this study, the morphologic, occlusal, and functional characteristics and orthodontic approach to MLD malocclusion are discussed.
Material and methods
The Human Research Ethics Board at Kanagawa Dental College approved this study, and informed consent was read and signed by each participant.
Initial records of patients with nonhereditary craniomandibular asymmetry before, during, and after orthodontic treatment at the orthodontic department of Kanagawa Dental College were selected. A total of 116 patients (average age, 20.8 ± 7.8 years; 35 males: age, 20.7 ± 6.8; 81 females: age, 20.9 ± 8.3 years) diagnosed as having MLD without pathologic conditions that affect the TMJs, including congenital disorders such as hemifacial microsomia, condylar hyperplasia, rheumatoid arthritis, and osteoarthritis, participated in this study. These patients’ facial morphology was examined by using posteroanterior cephalograms, occlusion guidance on the articulator after face-bow transfer, and condylar movement with a condylograph. All patients were treated or intended to be treated for their MLD malocclusion according to the treatment protocol at Kanagawa Dental College based on vertical dimension and occlusal plane control.
The morphologic characteristics of MLD were studied on the cephalograms as shown in Figure 1 . The midfacial reference plane to assess facial asymmetry was a line running through crista galli and anterior nasal spine. The angle between the midfacial plane and the line running through anterior nasal spine and menton was defined as the degree of MLD. A positive value indicated MLD to the left side and a negative value to the right side. The angle between the perpendicular line of the midfacial plane and the line running through the occlusal surface of the bilateral maxillary first molars was defined as the OP. The angle between the perpendicular line of the midfacial plane and the line connecting the right and left antegonial notches was defined as the frontal mandibular plane (AG). The angle between the perpendicular line of the midfacial plane and the line connecting the right and left mastoid processes of the temporal bone was defined as the frontal mastoid plane. Positive values of OP and AG indicated that these planes inclined superiorly toward the left side.
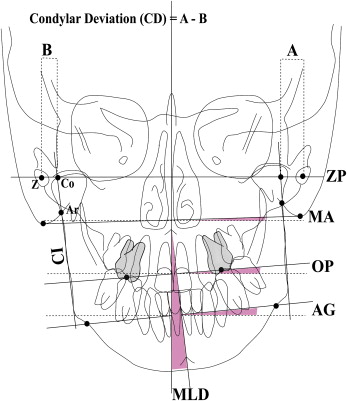
Since the condyle follows the growth of the whole ramus, to evaluate condylar deviation, the lateral ramus line, which was the tangent line from the cross point of the condylar process tracing and the tracing of the mastoid process to the lateral shape of gonial tracing, was drawn as an indicator of condylar inclination. Then, the central points of the oval shape of right and left zygomatic arches were connected as the zygomatic plane. The distance between the zygomatic arches and the cross point of the zygomatic plane and the condylar inclination was measured. The distance between right and left was subtracted to indicate condylar deviation, with a positive value indicating deviation to the right side and vise versa. It is easily recognized by correlation figures showing negative values for MLD right and positive values for MLD left.
The mounted maxillary casts were transferred to a 3-dimensional (3D) digitizer (Gamma GmbH, Klosterneuburg, Austria). The tooth guidance surfaces were designed for protrusion and laterotrusion. The start and end points of the occlusal guidance were called functional points Fl and F2 ( Fig 2 ). F1 and F2 were located on the mesial and distal marginal ridges of the maxillary central incisors and the mesial marginal ridges of the maxillary lateral incisors, canines, premolars, and first molars. The F1 points were created in maximum intercuspation with mandibular incisal edges, cusps of the canines, and buccal cusps of the premolars and the first molars in contact and are the starting points for eccentric movements.
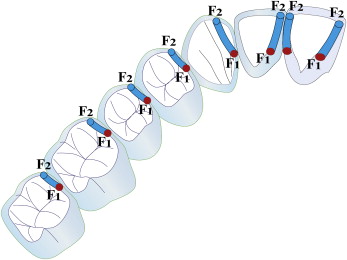
The most eccentric contact right before disocclusion is F2. It is located next to the incisal edge on the lingual surface of the maxillary front teeth. The F2 points in the premolars and molars was close to the cusp tip, usually not coinciding with it. A line connecting Fl and F2 showed an angulation to the axis-orbital plane referenced by anatomic face-bow transfer by using the anatomic hinge axis points and the left incisura infraorbitalis for mounting the maxillary casts in an articulator (SAM Präzisionstechnik, Munich, Germany). A 3D digitizer recorded the coordinates of both functional points after a mobile pin was placed on the respective spot. Calibration of the digitizer preceded every recording. The digitizer had a measuring accuracy of 0.01 mm, and each point was recorded 3 times. The corresponding inclinations of the maxillary second molars were measured for study purposes. A mobile measuring pin was manually moved to Fl and F2, and the digitizer recorded the coordinates of these points with reference to the axis-orbital plane. The inclinations of the guidance were then calculated from the coordinates, providing the average of the 3 measurements with reference to the axis-orbital plane.
Occlusal planes were also calculated by connecting the inclinations of the F1 points with reference to the axis-orbital plane. Three occlusal planes were measured. The conventional occlusal plane was the line connecting F1 of the central incisor and first molar, the anterior occlusal plane was that of the central incisor and first premolar, and the posterior occlusal plane was that of the second premolar and second molar.
The 3D condylar paths of the patients were recorded during opening and closing movements of the mandible and analyzed with a computerized condylography (Cadiax, Gamma Dental, Klosterneuburg, Austria) system. The condylography system consisted of a cranial attachment and a mandibular face-bow. A functional clutch was fixed to the labial surface of the mandibular dentition, and mandibular movements were confirmed to have no interference. The mandibular face-bow was then connected to the clutch. Two-dimensional condylar movement in the sagittal plane was recorded on digitizers, which were attached to the cranial face-bow and placed over the TMJ region bilaterally.
Lateral deviation of the condyle during mandibular functional movement was detected by the stylus attached to the mandibular face-bow. After positioning the stylus on the hinge axis, condylar movements in both TMJs were recorded 3-dimensionally from a reference position established by using unforced chin-point guidance.
To investigate the lateral shift of the condyle during opening movement (ΔY shift), the condylar paths in the transverse plane were observed on the condylographic tracing. As shown in Figure 3 , there were several types of ΔY shift that indicated medial (inward) and lateral (outward) deviation.
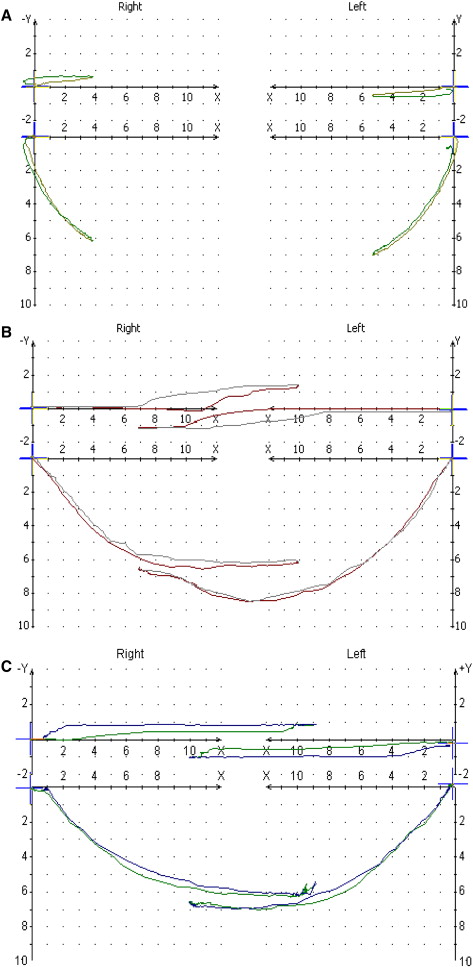
The ΔY shift was seen in different conditions of mandibular functional movement, which was evaluated by condylographic axis movement. They were classified into 3 groups according to mandibular lateral translation (MLT): (1) MLT with closed lock (closed lock ΔY), which showed lateral translation with severely limited condylar movement during opening and closing movements; (2) MLT with overrotation (overrotation ΔY), which showed lateral translation with excess condylar rotation in maximum opening position; and (3) MLT without closed lock and overrotation, which showed lateral translation (ΔY MLT) relatively close to the reference.
Statistical analysis
Statistical analyses were performed with the SPSS program for Windows (version 15, SPSS, Chicago, Ill). The mean values and standard deviations for all measured variables of occlusal plane inclination, occlusal guidance inclination, and condylar movements (open/close, protrusion/retrusion, and mediotrusion/medioretrusion) were calculated for each subject. In addition to standard descriptive statistical calculations, the Student and Welch t tests were used to detect differences of outcome measurements between the 2 groups: shifted and nonshifted sides in MLD ( Tables I-V ), and the statistical significance levels were established at P <0.05 and P <0.01. Percent distribution of the 4 patterns of lateral translation including the relationship between MLD and ▵Y-shift directions was also calculated ( Tables VI , VII ).
| Shifted side (mm) | Nonshifted side (mm) | |||||
|---|---|---|---|---|---|---|
| Occlusal planes | Mean | SD | Mean | SD | Difference (mm) | P |
| 1-6 | 11.35 | 4.12 | 10.49 | 3.66 | 0.86 | |
| 1-4 | 10.35 | 4.36 | 9.63 | 4.17 | 0.72 | |
| 5-7 | 18.05 | 12.29 | 13.81 | 5.85 | 4.24 | ∗ |
| 6-7 | 20.39 | 12.13 | 15.22 | 5.28 | 5.17 | ∗ |
| Shifted side (mm) | Nonshifted side (mm) | |||||
|---|---|---|---|---|---|---|
| Tooth | Mean | SD | Mean | SD | Difference (mm) | P |
| Central incisor | 55.48 | 10.09 | 55.07 | 9.32 | 0.41 | |
| Lateral incisor | 51.10 | 10.48 | 53.62 | 12.01 | 2.52 | |
| Canine | 45.22 | 8.47 | 49.13 | 9.63 | 3.91 | ∗ |
| First premolar | 27.78 | 11.77 | 33.25 | 11.63 | 5.47 | ∗ |
| Second premolar | 18.18 | 10.40 | 24.97 | 11.21 | 6.79 | ∗ |
| First molar | 8.36 | 6.88 | 13.23 | 8.83 | 4.87 | ∗ |
| Second molar | 7.83 | 9.64 | 10.14 | 6.63 | 2.31 | |
| Shifted side (mm) | Nonshifted side (mm) | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Difference (mm) | P | |
| Quantity (mm) | 16.68 | 2.83 | 15.21 | 2.67 | 1.47 | † |
| SCI (at S = 3 mm) | 53.75 | 10.30 | 53.49 | 10.43 | 0.26 | |
| SCI (at S = 5 mm) | 54.09 | 9.24 | 52.65 | 9.53 | 1.44 | |
| SCI (at S = 10 mm) | 46.68 | 9.31 | 44.94 | 9.42 | 1.74 | |
| TCI (at S = 3 mm) | 0.00 | 10.08 | 3.25 | 13.78 | 3.25 | |
| TCI (at S = 5 mm) | –1.11 | 4.18 | 1.63 | 6.97 | 2.74 | ∗ |
| TCI (at S = 10 mm) | –1.50 | 3.74 | 1.19 | 3.68 | 2.69 | † |
| S-E difference | 0.82 | 0.79 | 0.43 | 0.49 | 0.39 | ‡ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


