Normal-sleeping individuals experience a lower metabolic rate and relative cardiovascular quiescent state with lower heart rate and blood pressure that naturally occurs during sleep compared with the waking state. In patients with obstructive sleep apnea (OSA), this quiescent state becomes disrupted. Research has shown a higher risk for several medical disorders, most ominous being a myocardial infarction or stroke. This article serves as an overview to the cardiovascular, cerebrovascular, metabolic, and gastroesophageal effects of OSA.
Normal sleeping individuals experience a lower metabolic rate and relative cardiovascular quiescent state with lower heart rate and blood pressure that naturally occurs during sleep compared with the waking state. In patients with obstructive sleep apnea (OSA), this quiescent state becomes disrupted. Research has shown a higher risk for several medical disorders, most ominous being a myocardial infarction or stroke. This article serves as an overview to the cardiovascular, cerebrovascular, metabolic, and gastroesophageal effects of OSA.
Overview of pathophysiology
Complete pathophysiology and background of disease mechanisms is beyond the scope of this article; however, a brief introduction may be helpful before introducing each medical complication of sleep apnea. Please see Fig. 1 for a graphical representation of the following succinct explanation.
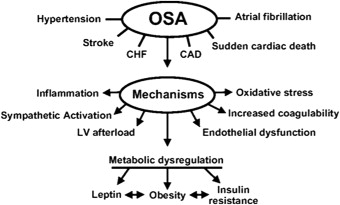
Most patients with sleep apnea trigger hypoxemic events during the apnea with reoxygenation on recovery from the apnea event, causing oxidative stress. Intermittent hypoxia can potentially lead to reactive oxygen species that can damage biomolecules and alter cellular functions that can contribute to inflammation and endothelial dysfunction. The longer the period of apnea, the more likely transient hypercapnia can also result. It has also been well described that sleep apnea increases sympathetic activation leading to vasoconstriction, a strong factor in cardiovascular consequences of sleep apnea. Inflammation including elevations of C-reactive protein (CRP), adhesion molecules, and other cytokines and inflammatory mediators has been shown to be overly active in patients with sleep apnea. Although platelet dysfunction and factors of coagulation, such as fibrinogen, are increased in patients with sleep apnea, the clear connection to sleep apnea as a direct cause is not certain and may be linked to other comorbid conditions.
Each obstructive apnea is accompanied by waves of effort against a closed airway that, in turn, causes negative intrathoracic pressure changes. Transmural pressure increases across the heart and great vessels with a ripple effect of increased afterload, atrial size, diastolic dysfunction, and increased cardiac wall stress.
Leptin, a protein involved in appetite suppression, has been shown to be elevated in patients with OSA at levels higher than in subjects with a comparable body mass index (BMI). Other important metabolic dysregulation has a connection between relative insulin resistance and patients with sleep apnea. This glucose intolerance associated with OSA appears to be independent of BMI.
Cardiovascular
Systemic Hypertension
Important information to understand the link between systemic hypertension and patients with sleep apnea has been evident in several studies. The Wisconsin Sleep Cohort Study showed a dose-response relationship between OSA and blood pressure elevations independent of age, sex, BMI, and other factors. It is interesting to note that the Sleep Heart Health Study did not show a statistical difference once BMI was factored out, with the implication that the development of hypertension was more related to obesity itself rather than purely OSA. There were enough differences in study design, for example, using a different score for apnea-hypopnea index (AHI), so as not to discount a link with systemic hypertension; however, there are likely other associated factors. Nonetheless, the seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure stated the importance of OSA as a risk factor for systemic hypertension.
Intermittent nocturnal hypoxia not only sets off oxidative stress and other factors introduced earlier, but also activates the renin-angiotensin system. This then increases endothelin-l, an amino acid peptide produced by vascular endothelial cells and an important vasoconstrictor in the pathway leading to systemic hypertension. Angiotensin II, a bioactive product of the renin-angiotensin system, is a potent arteriole vasoconstrictor and triggers release of aldosterone that can lead to fluid accumulation and further airway resistance.
Continuous positive airway pressure (CPAP) has been shown to improve blood pressure control in hypertensive patients. A recent small study revealed that CPAP therapy in a small group of hypertensive subjects reduced sympathetic activity during the daytime and reduced vascular resistance. Another larger prospective controlled study showed data to suggest that OSA is associated with increased arterial stiffness that was independent of age, gender, BMI, antihypertensive medications, and hypertension and that CPAP therapy significantly reduced arterial stiffness. If a patient with elevated blood pressure cannot tolerate CPAP, oral appliances have also recently been shown to improve hypertension in small studies.
Myocardial Ischemia and Infarction
There is evidence of a greater prevalence of OSA in patients with coronary artery disease than those who do not have coronary artery disease. As mentioned earlier, intermittent hypoxia as a result of sleep apnea in the face of a reduction of stroke volume in combination with cardiac transmural pressure elevation in susceptible patients with coronary artery disease can lead to increased risk of myocardial infarction and sudden death. Other factors include blood pressure surges with the sympathetic activation and intrathoracic pressure swings, systemic inflammation, and endothelial dysfunction. Table 1 lists the process from pathophysiology to subsequent disease.
| Underlying Pathophysiology | Signs and Symptoms | Disease Progression |
|---|---|---|
| Profound intermittent hypoxia Sympathetic vasoconstriction Cellular level acidosis Blood pressure elevation Endothelial dysfunction Systemic inflammation ↑Cardiac transmural pressure |
Nocturnal angina (symptoms of chest discomfort) Nocturnal ST depression on electrocardiogram |
Coronary artery disease Ventricular arrhythmias Myocardial ischemia Myocardial infarction Sudden cardiac death a |
a Sudden cardiac death timing is traditionally between the hours of 6 and 11 am ; however, in those with OSA, this shifts over to traditional sleeping periods, most pronounced between 12 midnight and 6 am .
When patients with OSA were compared with control subjects, there were more episodes of cardiac arrhythmias and nocturnal ST-segment depression. Peker and colleagues reported, on a study of 182 men with and without OSA over 7 years, an increased risk of developing cardiovascular disease that was independent of age, BMI, blood pressure, and smoking. A larger study of participants followed over a 10-year period showed a significant increase in both fatal and nonfatal cardiovascular events in patients with severe OSA who were on no therapy compared with healthy controls. CPAP therapy for patients with OSA with ischemic heart disease has been shown to lessen the severity of ST-segment depression. Despite growing evidence of nocturnal cardiac ischemia in patients with OSA, a small study of patients with coronary artery disease with moderate or severe OSA did not show detectable myocardial injury by cardiac troponin T assay. Another study also mentioned that cardiac troponin assay remained unchanged; however, CRP served as a useful cardiac biomarker. CRP correlated with improved systolic and diastolic cardiac function and overall cardiovascular remodeling in patients with OSA on CPAP therapy.
Cardiac Arrhythmias
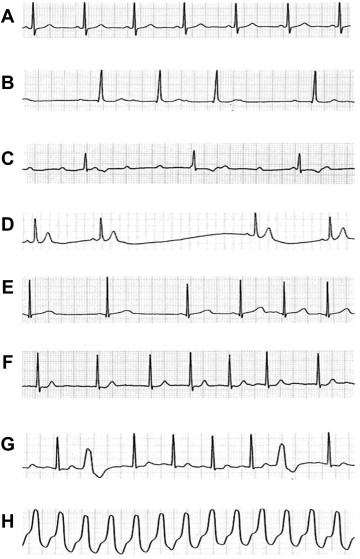
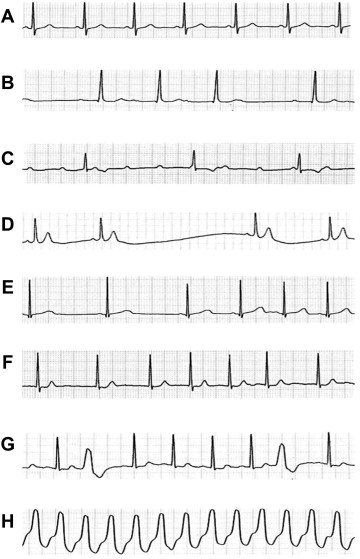
Some cardiac arrhythmias can occur during sleep in healthy individuals, including premature atrial contractions, premature ventricular contractions, and sinus pauses. Patients with OSA have been shown to have premature ventricular contractions, nonsustained ventricular tachycardia, bradyarrhythmias, sinus arrest, and second-degree atrioventricular block. Fig. 2 shows examples of various electrocardiographic (ECG) rhythms during sleep.
Patients with OSA can have more arrhythmias that cause adverse health consequences than patients who do not have OSA. Atrial fibrillation (AF) has a higher incidence in patients with OSA. AF has a very high risk of recurrence after cardioversion unless the patient is on adequate OSA therapy. Even after catheter ablation of AF, there is a 25% greater risk of recurring AF in patients with OSA than in those with no OSA.
Pulmonary Hypertension
Pulmonary hypertension in subjects with OSA is likely attributable to hyper-reactivity to hypoxia, pulmonary arteriole remodeling, and impaired left ventricular diastolic function and enlarged left atria. Although there are multiple pulmonary artery pressure elevations with OSA events, daytime sustained pulmonary hypertension as a result of sleep apnea has been less clearly linked. Patients with pulmonary hypertension and OSA tend to have more profound nocturnal hypoxemia, but may also have daytime hypoxemia as well, such as in obesity-hypoventilation syndrome or in patients who also have chronic obstructive pulmonary disease (COPD). Those patients with OSA with more predominant hypoxemia are at greater risk, as hypoxemia induces pulmonary artery pressure elevation. Despite controversy as to whether OSA is a primary cause of persistent pulmonary artery hypertension, CPAP has been shown to lower pulmonary artery pressure.
Cardiovascular
Systemic Hypertension
Important information to understand the link between systemic hypertension and patients with sleep apnea has been evident in several studies. The Wisconsin Sleep Cohort Study showed a dose-response relationship between OSA and blood pressure elevations independent of age, sex, BMI, and other factors. It is interesting to note that the Sleep Heart Health Study did not show a statistical difference once BMI was factored out, with the implication that the development of hypertension was more related to obesity itself rather than purely OSA. There were enough differences in study design, for example, using a different score for apnea-hypopnea index (AHI), so as not to discount a link with systemic hypertension; however, there are likely other associated factors. Nonetheless, the seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure stated the importance of OSA as a risk factor for systemic hypertension.
Intermittent nocturnal hypoxia not only sets off oxidative stress and other factors introduced earlier, but also activates the renin-angiotensin system. This then increases endothelin-l, an amino acid peptide produced by vascular endothelial cells and an important vasoconstrictor in the pathway leading to systemic hypertension. Angiotensin II, a bioactive product of the renin-angiotensin system, is a potent arteriole vasoconstrictor and triggers release of aldosterone that can lead to fluid accumulation and further airway resistance.
Continuous positive airway pressure (CPAP) has been shown to improve blood pressure control in hypertensive patients. A recent small study revealed that CPAP therapy in a small group of hypertensive subjects reduced sympathetic activity during the daytime and reduced vascular resistance. Another larger prospective controlled study showed data to suggest that OSA is associated with increased arterial stiffness that was independent of age, gender, BMI, antihypertensive medications, and hypertension and that CPAP therapy significantly reduced arterial stiffness. If a patient with elevated blood pressure cannot tolerate CPAP, oral appliances have also recently been shown to improve hypertension in small studies.
Myocardial Ischemia and Infarction
There is evidence of a greater prevalence of OSA in patients with coronary artery disease than those who do not have coronary artery disease. As mentioned earlier, intermittent hypoxia as a result of sleep apnea in the face of a reduction of stroke volume in combination with cardiac transmural pressure elevation in susceptible patients with coronary artery disease can lead to increased risk of myocardial infarction and sudden death. Other factors include blood pressure surges with the sympathetic activation and intrathoracic pressure swings, systemic inflammation, and endothelial dysfunction. Table 1 lists the process from pathophysiology to subsequent disease.
| Underlying Pathophysiology | Signs and Symptoms | Disease Progression |
|---|---|---|
| Profound intermittent hypoxia Sympathetic vasoconstriction Cellular level acidosis Blood pressure elevation Endothelial dysfunction Systemic inflammation ↑Cardiac transmural pressure |
Nocturnal angina (symptoms of chest discomfort) Nocturnal ST depression on electrocardiogram |
Coronary artery disease Ventricular arrhythmias Myocardial ischemia Myocardial infarction Sudden cardiac death a |
a Sudden cardiac death timing is traditionally between the hours of 6 and 11 am ; however, in those with OSA, this shifts over to traditional sleeping periods, most pronounced between 12 midnight and 6 am .
When patients with OSA were compared with control subjects, there were more episodes of cardiac arrhythmias and nocturnal ST-segment depression. Peker and colleagues reported, on a study of 182 men with and without OSA over 7 years, an increased risk of developing cardiovascular disease that was independent of age, BMI, blood pressure, and smoking. A larger study of participants followed over a 10-year period showed a significant increase in both fatal and nonfatal cardiovascular events in patients with severe OSA who were on no therapy compared with healthy controls. CPAP therapy for patients with OSA with ischemic heart disease has been shown to lessen the severity of ST-segment depression. Despite growing evidence of nocturnal cardiac ischemia in patients with OSA, a small study of patients with coronary artery disease with moderate or severe OSA did not show detectable myocardial injury by cardiac troponin T assay. Another study also mentioned that cardiac troponin assay remained unchanged; however, CRP served as a useful cardiac biomarker. CRP correlated with improved systolic and diastolic cardiac function and overall cardiovascular remodeling in patients with OSA on CPAP therapy.
Cardiac Arrhythmias
Some cardiac arrhythmias can occur during sleep in healthy individuals, including premature atrial contractions, premature ventricular contractions, and sinus pauses. Patients with OSA have been shown to have premature ventricular contractions, nonsustained ventricular tachycardia, bradyarrhythmias, sinus arrest, and second-degree atrioventricular block. Fig. 2 shows examples of various electrocardiographic (ECG) rhythms during sleep.
Patients with OSA can have more arrhythmias that cause adverse health consequences than patients who do not have OSA. Atrial fibrillation (AF) has a higher incidence in patients with OSA. AF has a very high risk of recurrence after cardioversion unless the patient is on adequate OSA therapy. Even after catheter ablation of AF, there is a 25% greater risk of recurring AF in patients with OSA than in those with no OSA.
Pulmonary Hypertension
Pulmonary hypertension in subjects with OSA is likely attributable to hyper-reactivity to hypoxia, pulmonary arteriole remodeling, and impaired left ventricular diastolic function and enlarged left atria. Although there are multiple pulmonary artery pressure elevations with OSA events, daytime sustained pulmonary hypertension as a result of sleep apnea has been less clearly linked. Patients with pulmonary hypertension and OSA tend to have more profound nocturnal hypoxemia, but may also have daytime hypoxemia as well, such as in obesity-hypoventilation syndrome or in patients who also have chronic obstructive pulmonary disease (COPD). Those patients with OSA with more predominant hypoxemia are at greater risk, as hypoxemia induces pulmonary artery pressure elevation. Despite controversy as to whether OSA is a primary cause of persistent pulmonary artery hypertension, CPAP has been shown to lower pulmonary artery pressure.
Stroke
Stroke is a condition of acute injury to central nervous system tissue arising either from ischemia, which is more common, or hemorrhage. Transient ischemic attack (TIA) is a transient neurologic dysfunction secondary to focal ischemia but without infarction; however, it does increase the risk for stroke. Stroke is a major health care problem in the United States, leading to many deaths, as well as functional impairment in survivors. Both snoring and OSA have been linked to an increased incidence of stroke, and the risk for developing stroke increases with increased severity of sleep apnea at baseline. The increased incidence is most likely secondary to interplay of various factors (see Fig. 1 ). OSA is known to contribute to increased risk for hypertension, cardiac arrhythmia, increased platelet adhesions, and dysfunction of vascular endothelium. In fact, heavy snoring and OSA have been associated with increased risk for carotid atherosclerosis and arterial intima-media thickening. Interestingly, stroke and TIA are risk factors for developing obstructive and central apneas as well. About half of patients who had an acute stroke have sleep apnea, and improvement is expected, more with central than obstructive apnea events, in only about half of patients in subsequent months. Studies suggest that presence of moderate to severe OSA after stroke may lead to worse functional outcome and increase the risk for early death. There are limited and conflicting data on outcome of positive airway pressure therapy for sleep apnea following stroke.
Diabetes mellitus
There is a growing body of evidence from numerous human and animal studies that suggests an association between OSA and insulin resistance, glucose intolerance, and type 2 diabetes mellitus (DM2). Deficient insulin action lies at the heart of the problem in diabetes mellitus, which leads to hyperglycemia as a result of inadequate insulin secretion or diminished action on peripheral tissues, or both. The American Diabetes Association has established criteria to properly diagnose DM2 based on plasma glucose or hemoglobin A1C levels ( Box 1 ). An intermediate category is also recognized that puts an individual at risk for developing diabetes in the future. Prediabetes is the term often used to describe a clinical scenario where glucose levels are higher than normal but less than that used for diagnosing diabetes. Impaired fasting glucose and impaired glucose tolerance fall under this category ( Box 2 ).



