Chapter 4 Maxillary Sinus Grafting
Background, General Principles, and Techniques
Bone availability is the key to successful placement of endosseous implants 10 mm or longer in the posterior maxilla. When the thickness of the bone between the maxillary sinus and the alveolar crest is less than 10 mm, increasing the thickness of the alveolar sinus floor by bone grafting is one option that will support implants and prosthetic restoration. The graft material chosen must provide adequate viable bone to stabilize the implant initially and encourage osseointegration. Materials used for sinus floor grafting include autogenous bone, allogeneic bone, xenograft anorganic bone preparations, and alloplastic materials. Autogenous bone fulfills the criteria for an ideal graft.1
Long-term assessment of the amount of bone remaining around the implants has not been included in initial reports.2–24 However, a more recent report examined the use of tomography to assess the bone level (relative to the apical portion of the implant) and the height of alveolar ridge.25 This report indicated that after 5 to 10 years of function, bone formed in autogenous bone–grafted sinuses and was retained.25–33 The population in this study had simultaneous placement of hydroxylapatite (HA)–coated implants (e.g., cylinders, screw shapes) with autogenous bone grafts. After 5 to 10 years of function, bone was still present around the implants. Of the implants studied, 90% had bone covering the apical portion of the implant. This study supports the use of autogenous bone for sinus grafting. The techniques described in this chapter are similar to those mentioned in the long-term tomography study.25
In the tomography study, no attempt was made to differentiate prosthesis design, length and diameter of implants, or small variations in surgical technique (e.g., antibiotic coverage, flap design, type of implants used). Nevertheless, failure of the implants and grafts was rare. The prostheses fabricated for these patients followed well-known techniques. However, the effects of specific prostheses on graft maintenance and implant survival were not evaluated.25
The differences among types of grafts indicate that the addition of demineralized, freeze-dried bone (DFDB) to the iliac grafts slightly lowered the eventual bone level. Although this difference was statistically significant, the clinical difference was small, because the implants were still covered with bone. In some clinical situations, the amount of bone harvested from the donor site is less than ideal. In these cases, DFDB is added to increase the volume of the graft. Interestingly, the addition of DFDB does not increase the eventual graft volume on a long-term basis.
The autogenous cancellous bone graft contains endosteal osteoblasts that can survive the transplantation process when handled appropriately, and this graft subsequently forms bone.34–37 A corticocancellous block graft provides transplanted osteoblasts and growth factors, as well as structural rigidity, which frequently is required when implants are placed simultaneously.38 However, the cortical portion of the graft is slow to revascularize. The structural rigidity of the graft allows accurate implant placement, independent of the thickness of the sinus floor. The healing of these bone grafts follows a course that starts with basic wound healing and proceeds with bone remodeling.39–42
What alternatives might be used instead of autogenous bone and demineralized bone? Evidence is mounting that bovine bone (a xenograft) combined with autogenous bone or used by itself can induce bone formation within the graft and support implants.43–45 The use of fibrin glue creates cohesion of the composite particles, which limits their migration after placement of the graft in the sinus. Another alternative for the primary graft material is bone morphogenetic protein (BMP).46,47 BMP can be used to form bone within the sinus without the use of other materials. However, at this time, BMP combined with allografts do not have evidence-based clinical data on the incidence of bone formation in the sinus. It is expected that other combinations of materials that promote bone formation with the use of a scaffold will prove effective at solving the problem of vertical height deficiency in the future.
Presurgical Screening
Exclusion criteria that should be considered include the following:
Preoperative Radiographic Screening
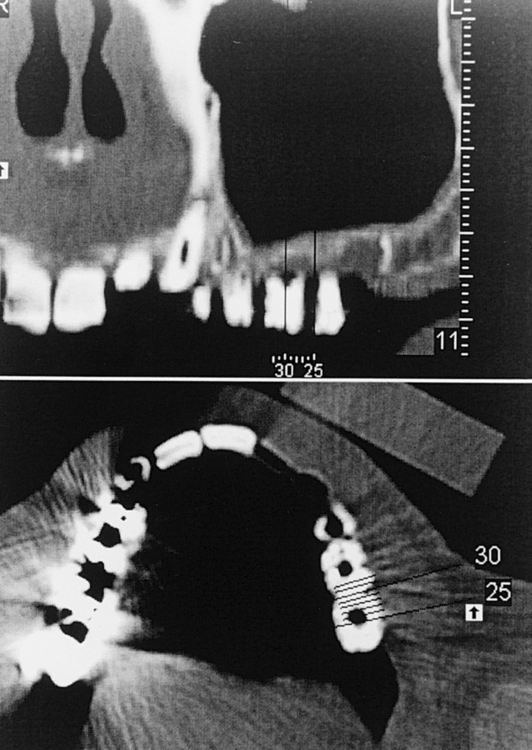
The preoperative radiographic examination begins with a panoramic radiograph. The clarity of the maxillary sinus, the presence of septa in the proposed surgical site, and an approximation of the thickness of the alveolar bone are visualized. Periapical radiographs do not usually contribute to the screening of the patient for sinus grafts. However, the panoramic radiograph has approximately 20% magnification error; also, detail is lacking on the facial-palatal thickness, morphologic structure of the alveolar bone and sinus floor, and status of the sinus membrane. Therefore, a reformatted computed tomography (CT) scan may be indicated for selected patients when more detail is desired (Figure 4-1, A-B).

• FIGURE 4-1 B, Reformatted cross section of the maxilla shown in Figure 4-1, A, showing the location of the cross section by number as it relates to the proposed implant location. The crosshatches at the bottom represent 1-mm increments, which allow thickness measurements of the bone. The proposed implant axial emergence is clearly evident in the stent.
CT scans are especially recommended for patients in whom the surgeon suspects multiple sinus septa or a pathologic condition in the sinus. The scans can document the thickness of the alveolar crest at the surgical sites and the thickness of the membrane. Before a CT scan is taken, all presurgical prosthetic planning should be complete, and a radiopaque stent indicating the positions of the planned restoration should be made. The scan is used to identify the specific locations of the planned implant sites and to provide the surgeon with an accurate understanding of the anatomy in the surgical location (see Figure 4-1).
Surgical Technique
The surgical procedure involves the removal or medial rotation of a window of cortical bone over the lateral aspect of the maxilla without perforation of the sinus membrane. Incisions should be made so as to allow adequate exposure of the surgical site and to avoid the placement of the incisions over the sinus window. After the lateral wall of the maxilla has been exposed, four linear ostectomies are performed to outline the window. The inferior horizontal ostectomy should be made as close to the floor of the sinus as possible to facilitate membrane dissection. The vertical ostectomies should be made close to the maxillary buttress and lateral nasal wall, again to facilitate membrane elevation. The superior horizontal cut should be made at the level of the planned augmentation height, which should allow placement of implants 15 mm long (DVD Figure 4-1, A). After the window has been created, the lateral bone still adherent to the sinus membrane can be either rotated medially (DVD Figure 4-1, B) or removed.
After the periosteum has been reflected superiorly, exposing the lateral wall of the maxilla, the planned ostectomy is visualized to start at the level of the maxillary sinus floor. The vertical osteotomies are parallel to both the lateral nasal wall and the anterior border of the maxillary tuberosity, where the maxilla curves posteriorly. The superior horizontal ostectomy is located where the vertical position of the augmentation is planned. A fiber-optic light source can be placed in the nose or against the palate to illuminate the sinus, allowing the surgeon to visualize the specific landmarks (e.g., floor of the sinus) and to perform an accurate ostectomy.
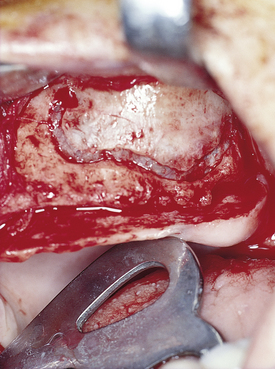
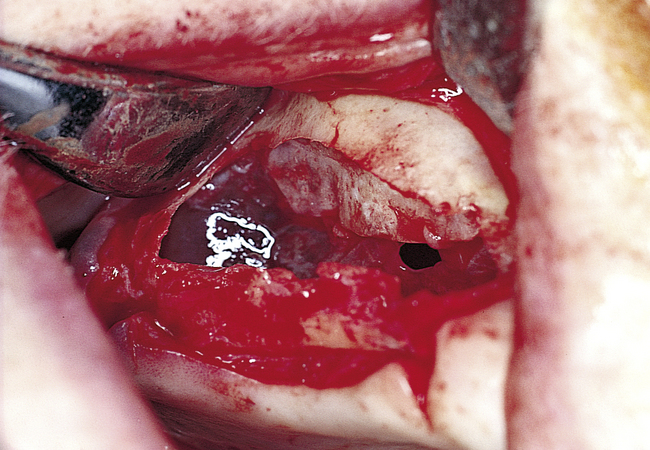
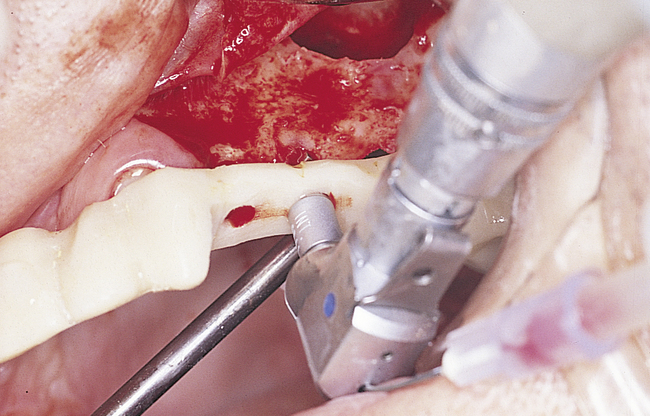
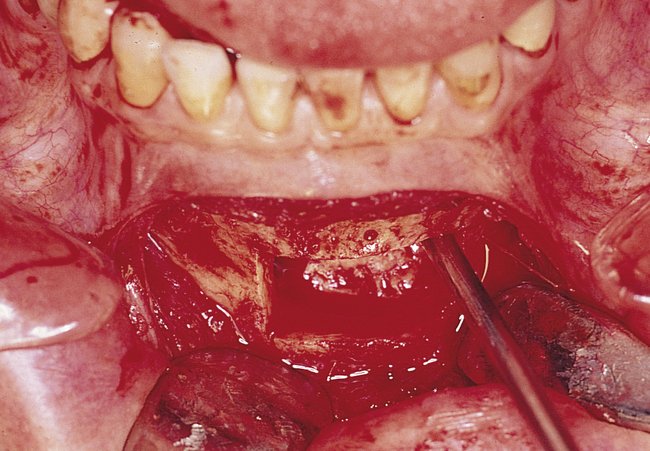
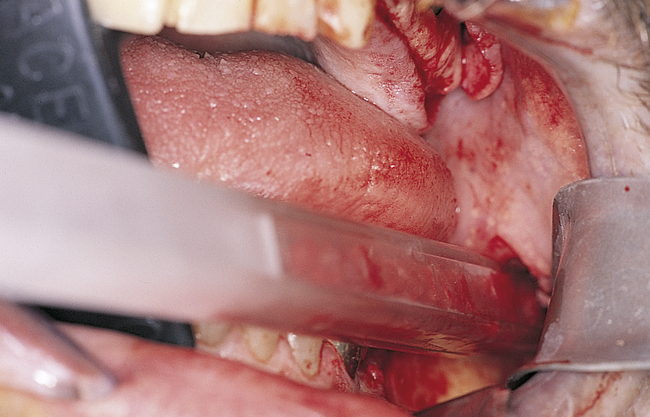
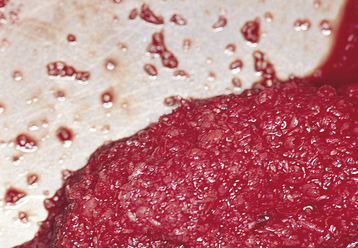
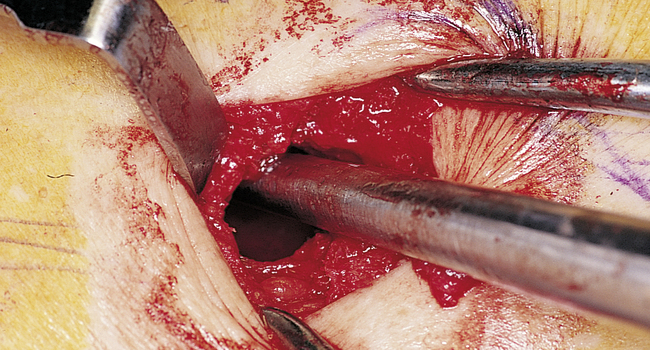
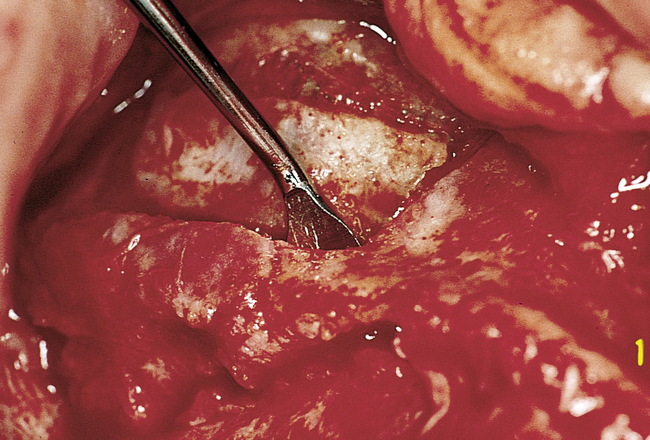
A round bur with irrigation is used to remove cortical bone and expose the gray, glistening sinus membrane (Figure 4-2, A). The lateral maxillary wall can be left intact and rotated inward as the new floor of the maxillary sinus, or it can be removed, depending on the clinician’s preference. A smooth, relatively new elevator is used to peel the sinus membrane from the floor of the maxillary sinus and lateral nasal wall (Figure 4-2, B). The membrane is elevated to the height of the desired augmentation. The edges of the sinus membrane are elevated initially, gradually increasing the distance of membrane elevation. Excessive elevation of one isolated portion of the membrane is avoided, because this would result in tension on the nonelevated membrane. The membrane must be sufficiently elevated to avoid excessive pressure when the sinus graft material is placed.
• FIGURE 4-2 B, Small Woodson elevator is used to elevate the thin sinus membrane from the inner aspect of the maxillary sinus.
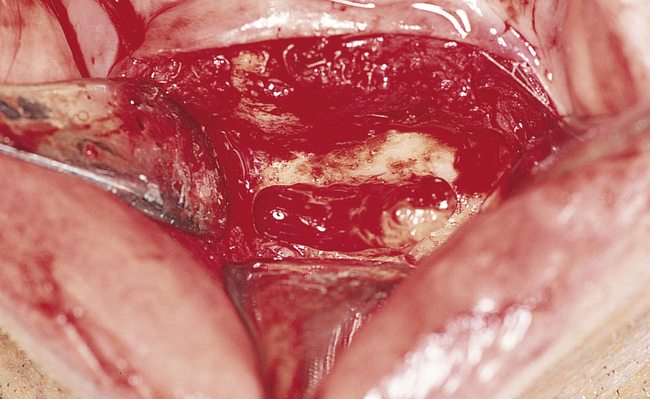
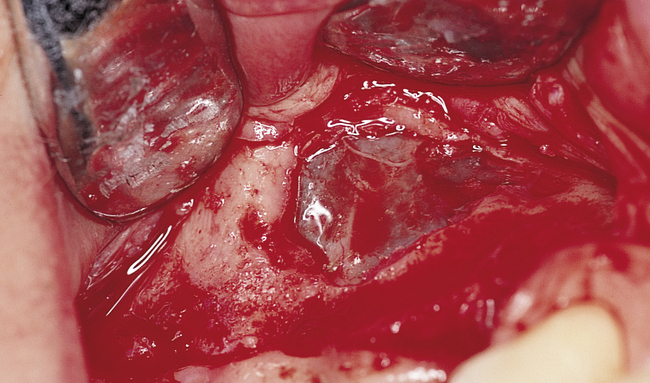
Perforations of the sinus membrane may occur, depending on the experience of the operator, location of the horizontal ostectomy, presence of septa, and thickness of the sinus membrane (Figure 4-2, C). Small perforations are left untreated. If large perforations are present, the procedure is aborted and attempted at a minimum of 4 months later. Use of a patch, such as a collagen membrane or other resorbable membrane, is at the discretion of the operator, with the understanding that the addition of such materials may increase the chances of postoperative infection. If solid blocks of bone are to be used, an intact sinus membrane may be less important. After the membrane has been elevated, the bone harvest procedure is performed.
Bone-Harvesting Techniques
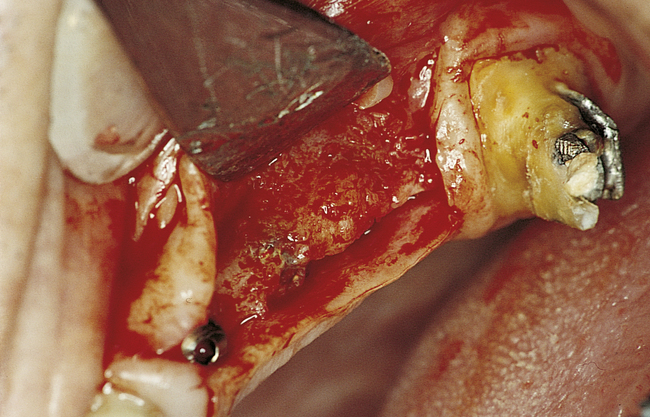
Jawbone Grafts
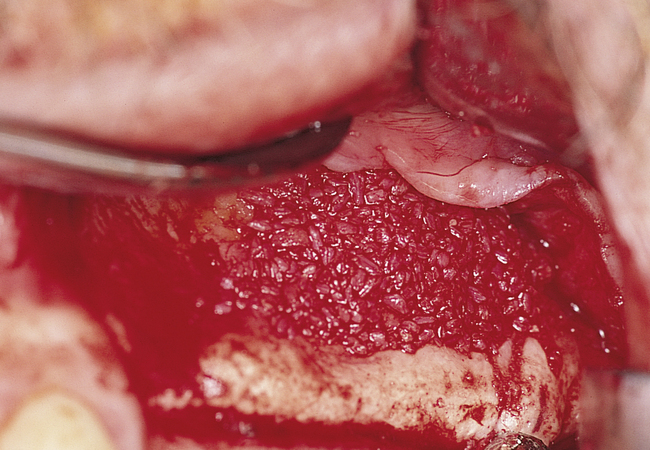
For the patient undergoing unilateral sinus graft surgery, the surgeon usually can harvest bone from the posterior maxilla, the mandibular third molar site, or the chin to obtain sufficient autogenous bone, mixed with an equal amount of DFDB, to augment one sinus (Figure 4-3, A-H). A scraping device can be used on the mandibular third molar sites to harvest cortical bone and a small amount of cancellous bone (Figure 4-4, A-H). The cortical portion of the mandible has very few viable osteoblasts. To gain additional bone, the surgeon also can use the chin as a harvest site. The chin cortex is removed with a round bur, and a sieve collection device is placed in the suction line. The round bur then is used within the confines of the cortical bone to harvest cancellous bone, which should contain viable osteoblasts.
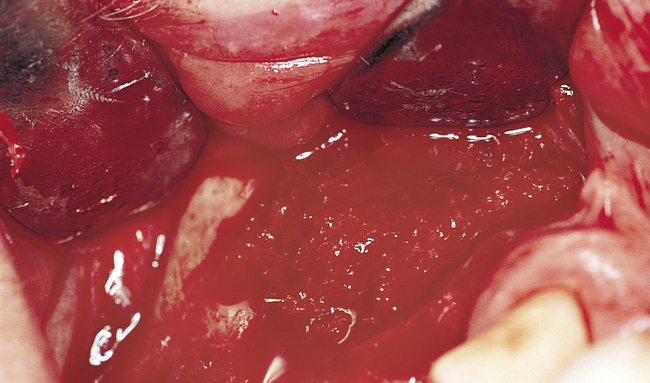
• FIGURE 4-3 F, After 6 months, the implants are exposed through a crestal incision. The implants are covered with bone.
When bone from the jaws is used, the volume of the graft usually must be augmented with either an allograft or a xenograft, depending on the clinician’s preference. Future use of alloplasts in various forms or recombinant proteins may affect the need for harvesting cancellous marrow.
Tibia Bone Grafts
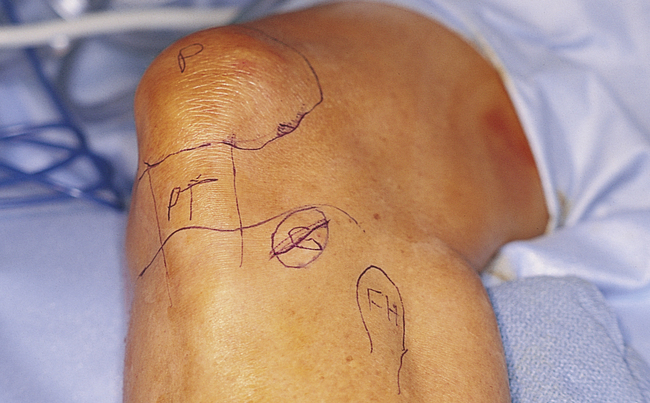
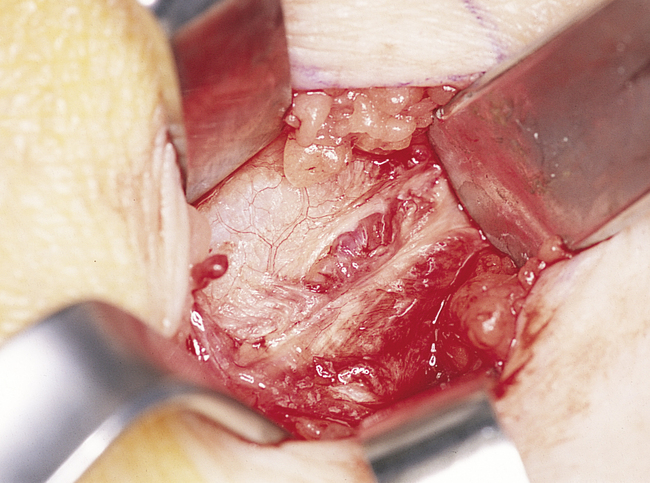
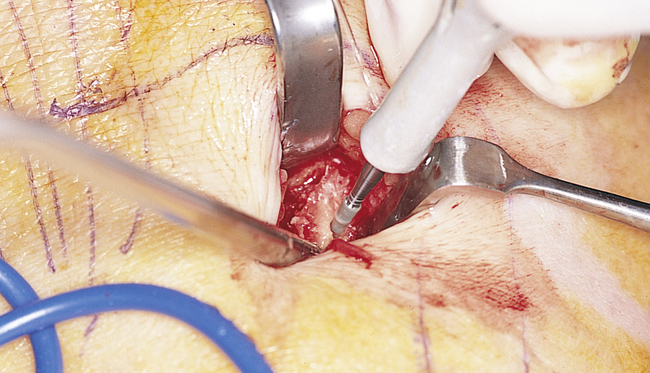
The harvesting of tibial bone involves identifying Gerdy’s tubercle, after which a sharp dissection to the periosteum overlying the tibial cortex is performed (Figure 4-5, A-I). Two techniques can be used to harvest tibial cancellous bone: (1) a periosteal osteocortical flap can be elevated, based on intact periosteum along the superior aspect of the cortical window, or (2) a small cortical window can be created, which is covered with periosteum after the bone has been harvested.

• FIGURE 4-5 G, Up to 22 ml of cancellous bone can be harvested from one tibia, which is sufficient to graft bilateral sinuses.
Periosteal osteocortical flap
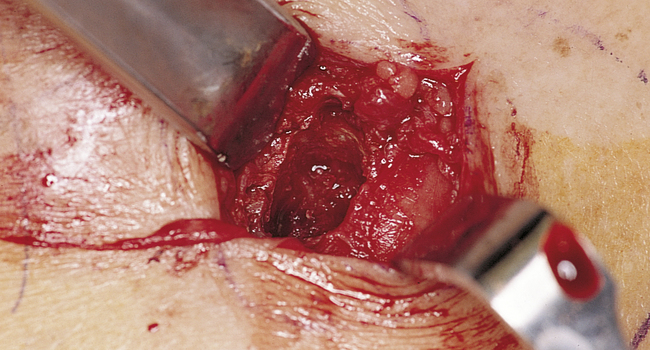
After the periosteum has been identified, a scalpel is used to score it along two vertical lines, each approximately 10 mm long, with a horizontal line at the inferior aspect of the vertical lines. A thin fissure bur is used to create a corticotomy through the three lines, leaving the superior aspect intact. The tibial cortex is elevated by performing a greenstick fracture of the cortex, exposing the cancellous bone within the tibia. The marrow is removed from the cancellous space along the level of the window—inferiorly, not superiorly. After the marrow has been harvested, the area is irrigated thoroughly and closed in layers. The periosteum is sutured to reapproximate the cortical window and close the cortical defect. The subcutaneous tissues are closed, and the skin is closed with a subcuticular suture, with or without the addition of skin sutures as necessary.
Postoperative management
For either technique, the patient is instructed to avoid impact loading of the leg for at least 6 to 8 weeks. The leg should be elevated, and ice should be applied to the surgical site for 24 hours. The patient is warned to avoid soaking the leg in a bath for at least 10 days. The patient is examined the next day so that the dressing can be cleaned and questions addressed. Antibiotics to cover gram-positive cocci and pain medication are prescribed for postoperative management.
Iliac Crest Grafts
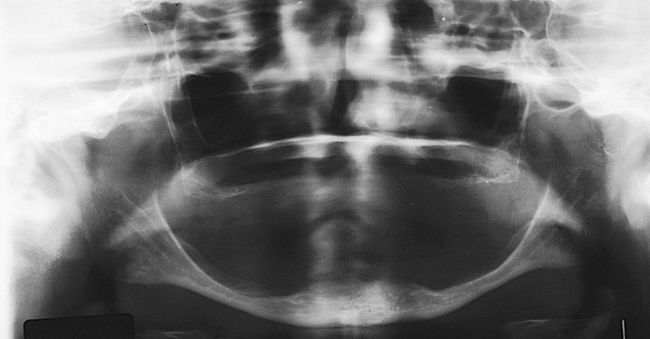
In addition to the tibia, the iliac crest can serve as the source of large amounts (more than 20 ml) of cancellous marrow. The technique for harvesting iliac crest cancellous marrow involves elevation of the iliac cortical crest and curettage of the marrow. The cortical plates are replaced and sutured back into position.
Multiple approaches can be used to reach and harvest bone from the iliac crest. For sinus grafting, the anterior approach usually is performed, because it does not require turning the patient after the sinus elevation has been completed. In addition, a satisfactory amount of bone usually can be harvested from the anterior approach. To limit blood loss and minimize gait disturbances, the technique most often used involves a relatively avascular approach, with great care taken to avoid the sensory nerves that traverse the iliac crest region. After a sterile preparation and draping of the anterior iliac crest, a local anesthetic is administered. Blunt dissection with hemostatic control using electrocautery is used to approach the anterior iliac crest. The approach should be performed from the lateral anterior aspect to prevent reflection of the insertion of the tensor fasciae latae muscle, which will minimize long-term gait disturbances. The muscles are separated rather than incised, with the dissection medial to the gluteus medius muscle and lateral to the iliacus muscle. In the area of the iliac tubercle, fibers from the external oblique and other muscles may need to be elevated when large pieces of bone are harvested, but these fibers should be left intact if possible. The sensory nerves usually pass over the anterior and posterior spines and are encountered in fewer than 2% of patients. Usually they can be retracted, and sensory loss thus is a rare complication from iliac crest bone harvest.48
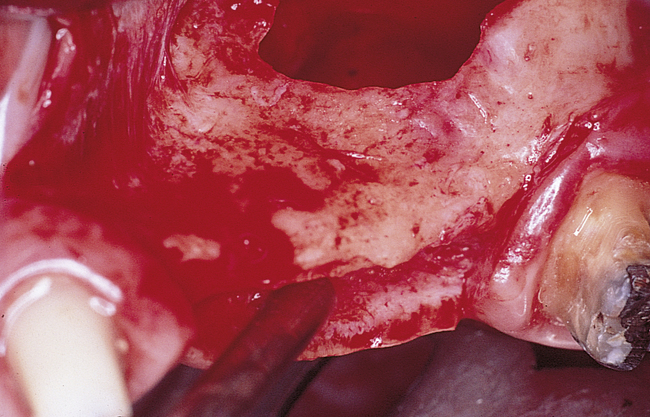
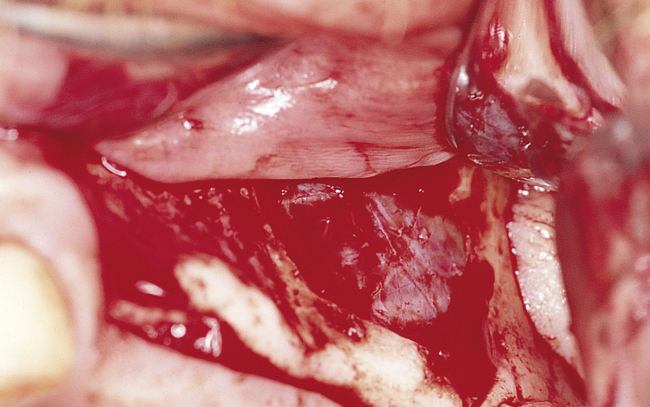
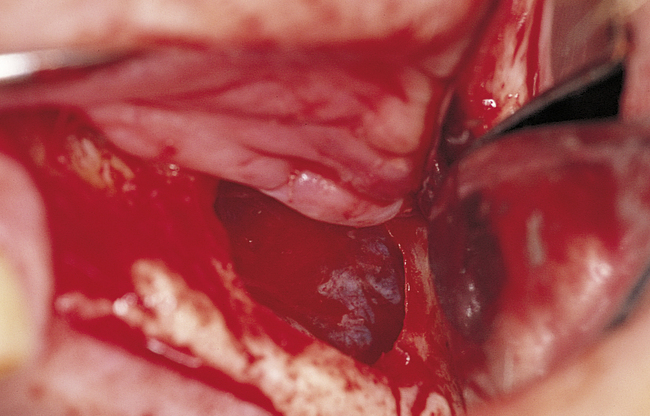
For the harvesting of blocks of corticocancellous bone, either the lateral or the medial cortical plates of the iliac bone are stripped of periosteum (Figures 4-6, A-E, and 4-7, A-M). A saw with copious irrigation or sharp osteotomes are used to outline and remove a piece of bone. Additional cancellous bone can then be collected, after which the wound is closed in layers.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses