Pneumatization of the maxillary sinus secondary to posterior maxillary tooth loss is an extremely common finding. Significant atrophy of the maxilla prevents implant placement in this region. For several decades, sinus augmentation has been used to develop these sites for dental implant placement. The main techniques for increasing the vertical bone height of the posterior maxilla are the transalveolar and lateral antrostomy approaches. The clinical and radiographic examinations dictate the appropriate method for each clinical situation. Both techniques have been shown to have high success rates. However, practitioners must be aware of potential complications and how to address them.
Key points
- •
Atrophy of the posterior maxillary alveolar bone is commonly encountered after tooth loss.
- •
There are 2 main approaches to sinus augmentation in preparation for implant placement: transalveolar and lateral antrostomy.
- •
Knowledge of the complications associated with this procedure is essential for successful treatment.
History
The presence of the maxillary sinuses mystified scientists for several hundreds of years. Galen is credited as one of the first people to recognize the existence of the paranasal sinuses. He noted porosities in the bone that he thought made the head less heavy.
Little scientific progress was made during the middle ages. During the Renaissance, Leonardo da Vinci and Andreas Vesalius both described the paranasal sinuses, including the maxillary sinus, in great detail. Fallopius recognized the enlargement of the sinuses with age. In the seventeenth century, Nathaniel Highmore recorded a case of odontogenic, purulent sinusitis.
The American George Caldwell and the Frenchman Henry Luc separately described a procedure to access the maxillary sinus using a lateral window in 1893. The procedure was used to treat disorders of the antrum.
In the 1970s, Tatum and colleagues used the sinus cavity to increase available bone using graft material, which allowed greater implant-to-bone contact area once the bone graft matured.
History
The presence of the maxillary sinuses mystified scientists for several hundreds of years. Galen is credited as one of the first people to recognize the existence of the paranasal sinuses. He noted porosities in the bone that he thought made the head less heavy.
Little scientific progress was made during the middle ages. During the Renaissance, Leonardo da Vinci and Andreas Vesalius both described the paranasal sinuses, including the maxillary sinus, in great detail. Fallopius recognized the enlargement of the sinuses with age. In the seventeenth century, Nathaniel Highmore recorded a case of odontogenic, purulent sinusitis.
The American George Caldwell and the Frenchman Henry Luc separately described a procedure to access the maxillary sinus using a lateral window in 1893. The procedure was used to treat disorders of the antrum.
In the 1970s, Tatum and colleagues used the sinus cavity to increase available bone using graft material, which allowed greater implant-to-bone contact area once the bone graft matured.
Pneumatization of the sinus
There has been a downward trend in rates of tooth loss in the United States. However, because of the growing elderly population, the absolute number of lost teeth is increasing. The department of health and human services (HHS) reported in the national health and nutrition examination survey (NHANES) study that 62% of Americans aged 35 to 44 years reported tooth loss caused by caries or periodontal disease. The prevalence of edentulism among seniors (aged 65 years and older) was 27%. The American Academy of Implant Dentistry reports that 3 million people in the United States have dental implants. This number is expected to grow yearly by 500,000.
Because of the presence of the maxillary sinuses, posterior maxillary alveolar bone loss creates a unique problem for implant placement after tooth extraction. The cause of this issue is increased pneumatization of the maxillary sinus ( Fig. 1 ). Increased osteoclastic activity within the periosteum of the schneiderian membrane results in expansion of the maxillary sinuses. Also, increased positive pressure is thought to contribute to alveolar bone atrophy. The soft, type IV bone in the posterior maxilla has low resistance to these processes. The end result is a decrease in vertical bone height (VBH) of the alveolus in the edentulous areas.
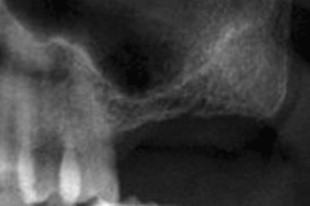
In a radiographic study, Sharan and Madjar found that “sinus expansion was considerably larger in cases of extractions of teeth enveloped by a superiorly curving sinus floor… Sinus expansion was larger in cases of second molar extractions (in comparison to first molars) and in cases of extraction of 2 or more adjacent posterior teeth.”
Davarpanah and colleagues classified posterior maxillary bone loss into several categories:
- •
Vertical bone loss from within the sinus: a reduced distance from the floor of the sinus to the alveolar ridge crest. However, no loss of interocclusal distance.
- •
Vertical bone loss of the alveolar ridge: loss of alveolar ridge below the sinus. There is an increase in interocclusal distance.
- •
Horizontal bone loss of the alveolar ridge: a loss in buccopalatal width of alveolar bone.
- •
Combination subsinus loss: both vertical and horizontal bone loss.
Other grafting techniques such as block grafting or guided bone regeneration are required to treat the different atrophy patterns. This article focuses on sinus augmentation to increase the VBH available for implant placement.
Anatomy
Osteology
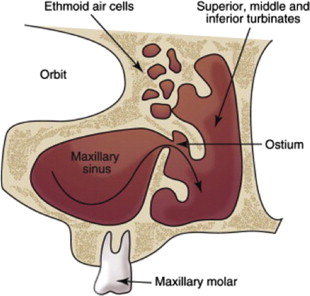
The largest of the paranasal sinuses, the maxillary sinuses are pyramidal in shape. The base of the pyramid is the lateral nasal wall with the apex pointing toward the zygomatic process of the maxillary bone. The average dimensions of the adult maxillary sinuses are 25 to 35 mm in width, 36 to 45 mm in height, and 38 to 45 mm in length. The inferior portion of the sinus is typically 1 cm below the nasal floor. The average volume of the maxillary sinus is approximately 15 mL. This volume tends to increase with partial and full edentulism.
The anterior wall of the sinus extends from the inferior orbital rim to the maxillary alveolar process. It is composed of thin bone and serves as the surgical site for the Caldwell-Luc (lateral antrostomy) approach. The superior wall is the floor of the orbit. The posterior wall separates the maxillary sinus from the infratemporal fossa. The medial wall is also the lateral wall of the nasal cavity. The medial wall houses the primary ostium, which serves as the main conduit for drainage of secretions. The primary ostium exits along the superomedial aspect of the medial wall. The superior positioning of the ostium allows placement of graft material without hindering drainage. It drains into the ethmoidal infundibulum, then into the middle meatus of the nasal cavity at the hiatus semilunaris ( Fig. 2 ). Accessory ostia are found in approximately 15% to 40% of patients. They typically drain superior to the inferior turbinate, superior and posterior to the uncinate process.
Vasculature and Innervation
The infraorbital and posterior superior alveolar arteries, both branches of the internal maxillary artery, supply the lateral aspect of the maxillary sinus. Traxler and colleagues found that branches of these two vessels formed endosseous anastomoses in all specimens. In 44% of specimens there were also extraosseous anastomoses forming a double arterial arcade. The infraorbital artery, along with the nerve, runs along the superior wall of the antrum within the sinus mucosa. The artery gives off the middle and anterior superior alveolar arteries before exiting the skull. The infraorbital foramen is located on the anterior wall of the antrum. The medial aspect of the sinus receives blood supply from the posterior lateral nasal artery, a branch of the sphenopalatine artery. The high vascularity of this region results in a more favorable environment for graft integration.
Innervation is supplied by branches of the second division of the trigeminal nerve, which include the infraorbital, superior alveolar, and palatine nerves.
Schneiderian Membrane
The schneiderian membrane is composed of 3 layers. The first layer is periosteum, which covers the bone of the antrum. A layer of highly vascular connective tissue covers the periosteum. The last layer is pseudostratified columnar epithelium (respiratory epithelium) and is exposed to the sinus cavity. The schneiderian membrane is continuous with the nasal mucosa as they connect at the ostia. The membrane is approximately 0.8 mm thick in the antrum.
Septa
Review of maxillary sinus anatomy cannot be complete without evaluation of septa. They can be divided into 2 groups: congenital and acquired. Congenital septa can be found anywhere in the maxillary sinus and develop as the midface grows. Acquired septa occur in areas where there is differential resorption of the maxillary alveolar bone along the sinus floor leading to bony crests. These septa are a result of tooth loss and eventual bone resportion.
Relationship to Dentition
The maxillary premolars and molars have an intimate relationship with the inferior aspect of the maxillary sinus. As shown by oral-antral communications during tooth extraction, the bone separating the apices from the sinus cavity is often extremely thin. Eberhardt and colleagues found that the mesiobuccal root apex of the second molar was closest to the sinus wall, with an average distance of 0.83 mm. The lingual root apex of the first premolar was the furthest from the sinus wall. In general, the molar roots were closer to the maxillary sinus than premolar roots.
Preoperative evaluation
Medical Evaluation
A thorough history and physical examination is required before the initiation of treatment. The patient’s current medications as well as allergies should be reviewed. The patient evaluation may necessitate consultation with a primary care physician or specialist. Appropriate laboratory tests should be ordered as needed.
Dental Evaluation
A comprehensive dental evaluation determines whether the patient is an appropriate candidate for implant placement with sinus augmentation. Diagnostic models can be used to evaluate the proposed surgical site. The patient’s occlusal scheme should be evaluated. In addition to horizontal measurements, the vertical dimension of the surgical site should be evaluated. An inadequate or excessive interarch distance can compromise the stability or esthetic outcome of the implants. In addition, the transverse relationship of the maxilla and mandible should be evaluated.
Radiographic Evaluation
Panoramic imaging is useful for a preliminary evaluation of the maxillary sinuses. The amount of VBH at the proposed surgical site can be evaluated. Furthermore, the antra can be evaluated for any disorder.
The panoramic radiograph is limited because it is two-dimensional, often distorted, and is prone to ghost images or artifacts. As a result, measurements can be inaccurate or disorders can be hidden. With cone-beam computed tomography (CT) technology becoming more prevalent in dental offices, CT scanning is becoming the standard for evaluation of the sinuses. Accurate measurements can be made in 3 dimensions and the contents of the sinus can be evaluated accurately. A survey found that 58.7% of otolaryngologists in New York State recommended CT evaluation to rule out disorders before sinus lift procedures.
Indications
The major indication for sinus augmentation is the atrophic posterior maxillary alveolus with loss of VBH. Pneumatization of the sinus results in insufficient bone to house an implant with adequate stability. There are 2 main approaches to sinus augmentation: transalveolar approach and lateral antrostomy (LA).
The decision as to which approach to use is largely based on the amount of residual maxillary alveolar bone remaining. Rosen and colleagues found that implant survival decreases with the transalveolar technique when 4 mm or less of residual bone height is present: “When presurgical bone height beneath the sinus is compared to implant survival, the data demonstrate that in sites of 4mm or less, there was a survival rate of 85.7%, which improved to 96% in locations with more than 4 mm of initial bone height.” Another study found that the transalveolar approach is indicated when greater than 6 mm of residual bone is present and 3 to 4 mm of bone height gain is planned. The LA approach was recommended for cases with less residual bone or if more bone height is needed.
If the LA approach is used, the practitioner can opt to place implants immediately or to delay placement after graft maturation. This decision is based on several factors. The quality of the bone (ie, its density) should be assessed. The amount of residual alveolar bone should also be evaluated. Immediate placement can be considered if the clinician can achieve primary stability of the implant. Reports have been published showing implant success with as little as 3 mm of VBH before sinus augmentation. However, it can be difficult to stabilize the implant with less than 3 mm of residual bone height. It is recommended that a minimum of 4 to 5 mm of residual bone height be present for immediate implant placement when using the LA technique ( Table 1 ).
| 4 mm of residual bone height or less | Lateral antrostomy with delayed implant placement |
| 4–5 mm of residual bone height | Lateral antrostomy, immediate implant placement if adequate stability can be achieved |
| 6 mm of residual bone height or greater | Transalveolar technique |
Contraindications
Several factors can increase the risk of implant failure and other adverse sequelae. Implant placement in bone of poor quality should be avoided because of the decrease in primary stability. Local or systemic causes can compromise bone quality ( Box 1 ).
-
Active sinus infection
-
Recurrent chronic sinusitis
-
Recurrent fungal sinusitis
-
Uncontrolled diabetes
-
Cystic fibrosis
-
Maxillary sinus hypoplasia
-
Neoplasms of the sinus
-
History of radiation therapy to maxilla
Before augmentation, the sinus should be evaluated for disorder. Contraindications include active sinus infection, recurrent chronic sinusitis, recurrent fungal sinusitis, uncontrolled diabetes, cystic fibrosis, maxillary sinus hypoplasia, neoplasms, and history of radiation therapy to the site. Any findings of the previously described conditions require consultation with a specialist. Smoking has been linked to an increased risk of complications associated with implant integration and sinus augmentation. However, it is a relative contraindication because failure rates were only slightly higher compared with nonsmokers.
Techniques
Transalveolar
The transalveolar sinus lift technique is more conservative than the LA approach. The sinus membrane is not directly instrumented. Also, the sinus cavity is not directly visualized and membrane perforations are more difficult to determine.
There are several options for incision design. The midcrestal incision along the alveolar ridge in a mesiodistal direction can be used. Vertical releasing incisions can be made along the lateral aspect of the maxilla if necessary to gain more exposure. The alveolar bone is exposed using a full-thickness mucoperiosteal flap.
A round bur is used to mark the surgical site along the alveolar ridge. A pilot drill with a diameter 1 to 1.5 mm less than the final implant diameter is then used. The pilot hole is made to a depth approximately 2 mm from the sinus floor. Creation of a pilot hole is not necessary if 5 mm or less of VBH is remaining.
Next, a mallet is used to drive successively larger osteotomes gradually to the final implant depth. Gradually increasing the depth decreases the potential for membrane tears. The smallest (first) osteotome fractures the sinus floor. The area of fracture increases as larger osteotomes are used. Single-site preparation is more prone to sinus perforation compared with multiple adjacent sites. The final osteotome should have a diameter approximately 0.5 mm less than the planned implant diameter.
Before implant placement, some investigators have proposed the introduction of bone graft into the osteotomy site. The rationale is to increase the amount of bone between the apex of the implant and the sinus floor. Si and colleagues found similar implant survival rates and no advantage in grafted sites versus nongrafted sites.
Lateral Antrostomy
A midcrestal or palatally positioned incision is made in a mesiodistal direction, and vertically releasing incisions are made. A full-thickness mucoperiosteal flap is elevated exposing the lateral wall of the maxillary sinus.
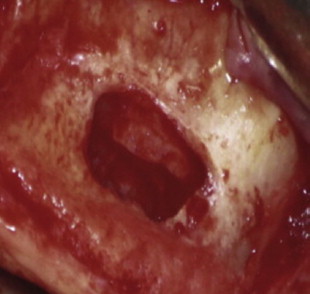
The superoinferior and anteroposterior borders of the lateral window are determined by evaluating the CT radiograph. The inferior border of the window should be 2 to 5 mm superior to the sinus floor to prevent difficultly during infracturing. The anterior border is determined by the mesial extent of the sinus, whereas the distal border is in the area of the first molar. The window is created with a low-speed drill with a diamond bur or a piezoelectric instrument. The window is prepared until a bluish hue is visible along the outline of the preparation. This indicates proximity to the schneiderian membrane. The corners should be rounded to prevent sharp edges, which can potentially perforate the membrane ( Fig. 3 ).