Modern orthognathic surgery has gone through different paradigm shifts since its origins. Research and technologic advances have influenced diagnosis, planning, and treatment, which has allowed surgical orthodontics to advance from a skeletal and functional paradigm to a soft tissue and facial esthetics paradigm in the 1990s. The latest shift is toward increased efficiency, decreased operating time, and ambulatory procedures that allow lower cost while keeping the highest standards regarding skeletal, functional, and soft tissue esthetic outcomes.
Increased efficiency, patient access to care, and affordability can be achieved by avoiding unnecessarily complex surgeries. This, in combination with constant communication between the members of the interdisciplinary team and the use of simple and effective procedures in office surgical suites or ambulatory surgery centers, will allow us to reduce costly operating room time and minimize the need for prolonged postoperative admission.
Discrepancies in the transverse plane are commonly diagnosed as isolated problems or as part of complex dentofacial deformities with a prevalence ranging from 10% to 15% in adolescents and up to 30% in adults. The most common transverse problems complicating the treatment of patients with dentofacial deformities are transverse maxillary deficiency and transverse mandibular excess. Transverse maxillary excess and transverse mandibular deficiency, though reported, are less frequent.
Correction of transverse problems in non-growing patients is a somewhat controversial subject in both the orthodontic and surgical literature. In patients with maxillary transverse deficiency, conventional orthodontic expansion is limited by the buccal cortical bone of the maxilla and by the lingual bone of the mandible. The orthodontist can compensate in some of these patients by using buccal crown torque in the maxillary posterior dentition or lingual crown torque in the mandible. Frequently, this type of compensation is unstable and may create functional interference. Oral and maxillofacial surgeons, in contrast, have traditionally been managing transverse problems with surgery on the maxilla via either surgically assisted rapid palatal expansion (SARPE) or segmental Le Fort I osteotomy. Use of a midline osteotomy for mandibular constriction has more recently been suggested for patients with wide mandibular arches who are undergoing concomitant bilateral ramus osteotomies. Although research on the results achieved with these surgical procedures has consistently shown acceptable stability on long-term follow-up, most studies are limited by either the number of patients studied or the length of follow-up (or by both).
This chapter emphasizes the diagnosis, indications, biologic foundation, limitations, stability, effects on facial esthetics, and postoperative care of each treatment alternative for discrepancies in the transverse plane.
Etiopathogenesis
The etiology of transverse maxillary and mandibular problems has been related to genetic factors, environmental influences, or a combination of these factors. The most common transverse problems are maxillary deficiency, mandibular excess, or a combination of both.
In children, maxillary constriction is manifested as a narrow palatal vault and unilateral or bilateral posterior crossbite. Appropriate orthodontic correction of this transverse skeletal discrepancy requires orthopedic maxillary expansion, which is possible only in patients who are still growing. The younger the child, the more effective the skeletal expansion; dental tipping is minimized and sutural distraction histogenesis is maximized. For this reason, orthopedic maxillary expansion is usually accomplished as part of a phase I treatment before puberty. At this stage, maxillary expansion removes the premature contacts that induce lateral functional shifts caused by the transverse discrepancy. When left untreated, these functional shifts can result in progressive and permanent mandibular skeletal asymmetry.
Rapid palatal expansion with a jackscrew appliance has been used reliably for more than 125 years in skeletally immature individuals. Even in the current practice of orthodontics, the most commonly used fixed expansion orthopedic appliances are tooth borne. Therefore, unwanted dentoalveolar movement should be expected to represent about 50% of the total expansion. This leads to a long-term loss of about 30% of the total arch expansion even after appropriate retention, thus confirming the need for overexpansion.
Multiple studies have reported on the age and process of closure of the mid-palatal suture. Most authors agree that mid-palatal suture growth continues until at least the age of 16 to 18, with a great deal of variation found among individuals. However, difficulty separating the maxillas in postpubertal individuals is not due just to complete fusion of the mid-palatal suture but also to the numerous mechanical interlocking that takes place in the circum-maxillary suture system once the patient stops growing and the sutures become non-functional. Because of these changes in adolescent and older patients, orthopedic expansion results in more dentoalveolar than skeletal movement, thereby increasing the risk for excessive dental tipping in the posterior segments, gingival recession, reduced alveolar bone height on the buccal root surfaces, lack of occlusal stability, and eventually relapse. Therefore, in mature patients undergoing orthodontic consultation for transverse discrepancies, diagnosis and treatment should be undertaken jointly by the orthodontist and surgeon.
Anatomy
Unilateral and bilateral crossbites, proclined and crowded teeth, narrow and tapered arches with the maxillary alveolar processes tipped outward, arch-length discrepancy, noticeable buccal corridors, and a deep palate are clinical hallmarks of skeletal transverse maxillary deficiency ( Fig. 77-1 ). Although excessive buccal corridors or negative space, defined as the space between the commissure and the buccal surfaces of the maxillary dentition during a full smile, may be due to a narrow maxilla, it can also be affected by the anteroposterior (AP) and vertical position of the maxilla relative to the lip drape. Crossbites with a wide palatal vault and maxillary alveolar processes tipped inward are commonly seen in patients with dental maxillary deficiency. Posterior crossbites with a three-dimensionally well-positioned maxilla, adequate upper incisor display, and the absence of buccal corridors and dental crowding are usually diagnosed as mandibular transverse excess. This is frequently seen in patients with mandibular AP deficiency and confirmed when models are positioned in class I occlusion.


Anatomy
Unilateral and bilateral crossbites, proclined and crowded teeth, narrow and tapered arches with the maxillary alveolar processes tipped outward, arch-length discrepancy, noticeable buccal corridors, and a deep palate are clinical hallmarks of skeletal transverse maxillary deficiency ( Fig. 77-1 ). Although excessive buccal corridors or negative space, defined as the space between the commissure and the buccal surfaces of the maxillary dentition during a full smile, may be due to a narrow maxilla, it can also be affected by the anteroposterior (AP) and vertical position of the maxilla relative to the lip drape. Crossbites with a wide palatal vault and maxillary alveolar processes tipped inward are commonly seen in patients with dental maxillary deficiency. Posterior crossbites with a three-dimensionally well-positioned maxilla, adequate upper incisor display, and the absence of buccal corridors and dental crowding are usually diagnosed as mandibular transverse excess. This is frequently seen in patients with mandibular AP deficiency and confirmed when models are positioned in class I occlusion.


Diagnostic Studies
Diagnostic studies use standard orthodontic records, which include cephalograms, models, orthodontic setups, and cephalometric analysis. The use of three-dimensional (3D) measurements with cone beam computed tomography (CBCT) is becoming more common and is of specific interest in the diagnosis and treatment planning of patients with transverse discrepancies and facial asymmetry.
To make an accurate diagnosis of a transverse discrepancy, the dental and skeletal components of the discrepancy need to be delineated. Models and orthodontic setups have commonly been used to evaluate these discrepancies. The first step includes leveling and alignment of the dentition over the basal bone to determine whether the discrepancy is an isolated dental problem. This is followed by analysis of models placed in class I canine occlusion to determine whether the transverse problem is absolute or whether it is a relative transverse deficiency or excess secondary to an AP discrepancy.
At this point, the presence and severity of the transverse discrepancy at the canine and molar levels must be determined. This is extremely important in establishing which orthodontic or surgical procedure (or both) will be indicated based on the pattern of expansion needed.
Ricketts proposed analysis with a transverse plane PA cephalogram to determine the presence of transverse skeletal dysplasia. The clinical application of earlier two-dimensional analyses was made difficult by imaging limitations such as the superimposition of anatomic structures, magnification, and the lack of reproducible measurements on PA cephalograms as a result of major changes induced by head positioning, even when standardized techniques were used.
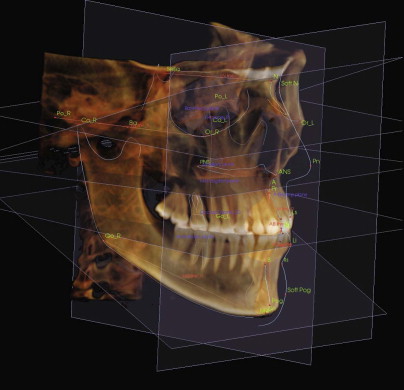
Adaptation of these and other analyses to the more readily available CBCT will allow greater accuracy in the diagnosis of these deformities. The third dimension missing from the cephalometric radiograph is the transverse plane or x-axis in the 3D coordinate system. The advent of CBCT and 3D software has made it possible for the orthodontist and surgeon to visualize, evaluate, and simulate hard and soft tissue changes in all three dimensions of the craniofacial structure ( Fig. 77-2 ).
Treatment/Reconstructive Goals
- •
An adequate transverse relationship improves dentofacial esthetics and periodontal health and increases long-term orthodontic stability. Transverse skeletal dysplasia is a risk factor for maxillary buccal gingival recession and periodontal disease.
- •
Improved smile esthetics is the main soft tissue effect of transverse skeletal correction.
Specific Treatment and Techniques
Le Fort I Segmental Osteotomy
Background
In 1972, Steinhauser reported a one-stage surgical procedure for expansion of the maxilla. The midline split could be performed on the posterior maxilla, anterior maxilla, or total maxilla. He thought widening the total maxilla to be technically difficult, however, because of the need to bone-graft the midline gap. To facilitate the procedure, palatal incisions were added to the buccal approach. Intermaxillary fixation was maintained for 4 to 6 weeks, and a retention plate was worn for 6 months to assist in stabilization of the transverse repositioning and to aid in consolidation of the bone graft. West and Epker described the application of Schuchardt’s two-stage (1959) and Kufner’s single-stage (1970) posterior maxillary osteotomies for correction of unilateral and bilateral posterior crossbite in patients whose mid-palatal suture was closed. With this technique, maxillary expansion became a one-stage osteotomy that separated the alveolus from the palate. Bell and Turvey reported the results of segmental maxillary surgery performed on 10 patients with a posterior crossbite. Segments were mobilized and positioned into a preoperatively determined occlusal relationship with a surgical splint and stabilized with wire fixation and intermaxillary fixation for 6 to 8 weeks. In 1985 in a series of 104 patients undergoing maxillary osteotomy, Turvey pointed out that transverse maxillary deficiency is seldom the only maxillary deformity, and he therefore recommended that a multisegment maxilla be created to correct the hypoplastic maxilla in all three planes of space.
Technique
Before surgery, orthodontic decompensation, leveling, and alignment should be achieved. Sufficient room between the dental roots should exist at the planned interdental osteotomy sites to minimize any damage to periodontal tissue.
Fabrication of two surgical splints, a palatal splint and an occlusal splint, minimizes intraoperative time. Maxillary segmentation for correction of the transverse deficiency is done on completion of the total maxillary osteotomy and down-fracture. Para-midline sagittal or horseshoe osteotomies are ideal when no changes in the maxillary occlusal plane are needed for the following reasons:
- •
It allows two separate areas of soft tissue expansion in the posterior maxilla to minimize tension, which can prevent expansion or induce relapse.
- •
The lateral palatal soft tissues are thicker, which minimizes the possibility of perforation or rupture of tissue. It improves the anatomy since most of these patients have a deep and narrow palatal vault preoperatively, and the palate will not only be wider but will also become less deep by lowering the central portion.
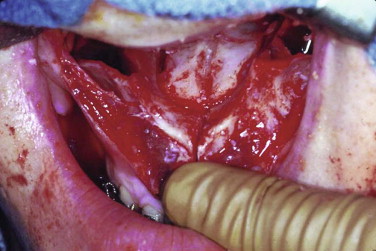
The lateral para-midline osteotomy and interdental cuts can be made with a small side-cutting bur or with a saw. Fine spatula osteotomes are also sometimes used to finish the cuts. In all cases a finger is placed on the palate to decrease the chance of soft tissue damage, as well as to ensure that the osteotomy is completed. Minimal soft tissue dissection at the interdental osteotomy sites is of upmost importance to preserve the blood supply to the dentoalveolar structures ( Fig. 77-3 ). The segments are mobilized with finger pressure, and a palatal splint without occlusal coverage is inserted. This palatal splint, which is held in place with wires or ball clasps, is constructed with acrylic and abuts the palatal surfaces of the upper teeth. The splint will stabilize the transverse change intraoperatively, and postoperatively it will be maintained for a period of 6 to 10 weeks, at which point it can be replaced by an orthodontic transpalatal appliance. Lack of occlusal coverage allows placement of an occlusal splint for AP and vertical repositioning of the maxilla. The occlusal splint is removed before the patient leaves the operating room to facilitate oral hygiene and avoid the discomfort that occurs with wiring the classic occlusal splint to the upper dentition. Grafting with autogenous bone, allogeneic bone, or hydroxyapatite, as well as plate and screw fixation across the palatal osteotomy gap, has been described, but there are no adequate data on long-term stability in support of one technique over the other.
Finally, the maxilla is put into its normal relationship with the mandible and placed in intermaxillary fixation. The maxilla is passively repositioned and secured with bone plates and screws, after which the intermaxillary fixation is removed and the occlusion confirmed. The soft tissue is closed carefully to minimize shortening of the lip, which often requires the use of an alar base cinch and V-Y closure to maximize paranasal and upper lip esthetics.
Pattern of Expansion
The multisegment Le Fort I osteotomy allows repositioning of the maxilla in all three dimensions, and correction of the transverse problem can be performed simultaneously with maxillary AP and vertical repositioning. When a maxilla is widened with the osteotomy made between the central incisors, the segments rotate outward with one or two axes of rotation at the incisal level, and the greatest surgical change occurs at the level of the second molars, which allows more intermolar than intercanine expansion.
Soft Tissue Esthetics
Soft tissue changes associated with Le Fort I osteotomies include upturning of the nose, increased exposure of the nares, increased width of the alar cartilage, shortening of the columella, shortening of the upper lip, and possibly loss of exposed vermilion and upper lip curl. These changes may be positive or negative, depending on the presurgical facial esthetic characteristics of the patient. In most patients with maxillary hypoplasia, the Le Fort I osteotomy with advancement and inferior repositioning of the maxilla will result in positive changes by improving the acute nasolabial angle and providing support for the paranasal soft tissues. However, its effects on the facial esthetics of patients with a short upper lip, thin vermilion border, and upturned nasal tip can be disastrous, even when soft tissue closure such as the alar cinch and V-Y closure are used to minimize these potential negative effects.
Stability
Segmental osteotomy for maxillary expansion is at the bottom of the hierarchy of stability as reported by Phillips and co-authors, with a relapse rate of 49% at the second molars and a more clinically significant 29% incidence of crossbite at the end of orthodontic treatment. Studies on maxillary expansion using rigid fixation give us a better idea of the stability of this procedure at the present time. To improve transverse stability, it is recommended that expansions greater than 10 mm be avoided and that overexpansion be built into the occlusal splint, which is maintained for 6 to 10 weeks and replaced with a transpalatal arch or any other orthodontic appliance to assist in maintenance of intermolar width during healing and postsurgical orthodontic treatment.
Surgically Assisted Rapid Palatal Expansion
Background
Kole in 1959 was the first to discuss corticotomy for the treatment of adults with maxillary constriction; the lateral maxillary wall was cut 1 cm above the apices, and a palatal incision was used to make a horizontal cut into the maxillary antrum. This was followed by the insertion of a dental-borne expansion device 8 weeks later. In the same year, Converse and Horowitz described three different surgical-orthodontic techniques.
- 1
Osteotomy through the entire mandibular or maxillary bone thickness
- 2
Dentoalveolar osteotomy in which the body is left intact but the teeth and their supporting structures are moved segmentally into a planned position
- 3
Cortical osteotomy or corticotomy to achieve displacement of the dentoalveolar segments more rapidly than with orthodontics alone, especially for maxillary expansion
Lines reintroduced corticotomy for adult rapid maxillary expansion in 1975. He reported making lateral incisions at the depth of the vestibule from the canine to the tuberosity and cutting the cortical plate from the piriform aperture to the zygomatic buttress. A palatal incision is made from behind the incisive papilla to the end of the hard palate with a burr. The expansion device is cemented 2 to 3 weeks postoperatively to allow healing and revascularization. This author extended the midline interdental bony cut to the piriform rim instead of using the interdental corticotomy described by Kole. Lines also suggested that because of the short duration and uneventful postoperative course, this procedure can be performed in an outpatient visit with local anesthesia and premedication. From this report two different groups of procedures have developed: SARPE originally and surgically facilitated orthodontic treatment (SFOT) more recently. The latter involves three different techniques that can be used alone or in combination, depending on the correction needed: a corticotomy-facilitated technique (with or without bone grafting), dentoalveolar distraction osteogenesis, and skeletal anchorage devices. SFOT is primarily indicated for dental movement, closure of extraction sites, and opening of implant sites, but it is also used for arch development and correction of dentoalveolar transverse discrepancies. Bell and Epker (1976) reported 15 patients who underwent SARPE under local anesthesia. Lateral maxillary bone cuts, pterygomaxillary disjunction, and interdental midline osteotomy were performed in all patients. Parasagittal palatal osteotomies were performed only in those with unilateral posterior crossbite. In the same year Kennedy and colleagues showed in their animal study that lateral maxillary osteotomies are key in achieving maxillary expansion.
Key factors to be considered in maxillary expansion include the extent of the arch length discrepancy, arch form, magnitude of the arch deficiency, smile esthetics, and vertical as well as AP position of the maxilla.
To determine the target expansion, it is advantageous to decompensate the lower arch by removing the curve of Wilson before proceeding with maxillary expansion or by doing a pretreatment orthodontic setup.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


