The term maxillary deficiency can be applied to deficiencies or hypoplasias of the maxilla in the transverse, anteroposterior (AP), and vertical dimensions. These deficiencies rarely occur in isolation and often present in some combination with each other and/or other skeletal abnormalities. For example, a patient could have a vertical maxillary hyperplasia, or excess, and nonetheless have a transverse deficiency. For sake of discussion in this chapter, we will focus on the discrepancies individually, with the understanding that their treatments may be combined with each other or other treatments.
When looking at the hierarchy of stability, the treatments of many maxillary deficiencies fall lower on the hierarchy of stability, specifically with regard to downgrafting of the maxilla and treatment of transverse discrepancy. Various techniques can be employed in an effort to mitigate this inherent instability. In this chapter, we will discuss surgically assisted rapid palatal expansion (SARPE), segmental Le Fort osteotomy, maxillary downgrafting with autogenous or bone alloplasts and donor bone (with the choice of material being open to personal preference), geometric osteotomies for downward movement without need for downgrafting, as well as straightforward maxillary advancement. The management of cleft patients and the use of distraction osteogenesis are covered elsewhere in this book.
Etiopathogenesis/Causative Factors
As with most skeletofacial deformities, maxillary deficiency is multifactorial. It can be congenital (syndromic), developmental (from variations in magnitude, direction, and timing of facial growth or as a result of a habit such as thumb sucking), traumatic (either in the absolute deformity or growth disturbance as a result of trauma), or iatrogenic in nature (such as secondary to cleft repair). Though the typical complaint of a Class III patient is that their “lower jaw is too big,” some degree of maxillary skeletal deficiency, without mandibular prognathism or excess, is present in as many as 75% of patients with Class III malocclusions. Transverse deficiency often is seen with maxillary AP deficiency. It has also been reported that 30% of all adult patients seeking orthodontic treatment for a dentofacial deformity have a component of transverse maxillary deficiency.
Pathologic Anatomy
The most significant issue regarding pathologic anatomy in patients with maxillary deficiencies is the quality and quantity of the bone of the maxilla. It is a frequent finding for the bone of the anterior maxillary wall to be extremely thin in AP deficiency, in particular, and apertognathia may be present, though that is not the topic of this chapter. In both AP and transverse deficiency, there is typically crowding of the maxillary dentition, which often results in flaring of the maxillary incisors. This compensation can camouflage the appearance of the degree of the underlying skeletal deformity.
Pathologic Anatomy
The most significant issue regarding pathologic anatomy in patients with maxillary deficiencies is the quality and quantity of the bone of the maxilla. It is a frequent finding for the bone of the anterior maxillary wall to be extremely thin in AP deficiency, in particular, and apertognathia may be present, though that is not the topic of this chapter. In both AP and transverse deficiency, there is typically crowding of the maxillary dentition, which often results in flaring of the maxillary incisors. This compensation can camouflage the appearance of the degree of the underlying skeletal deformity.
Diagnostic Studies
An important “diagnostic study” in the treatment of dentofacial deformities is consultation with an orthodontist. Typically, at the time of evaluation by the surgeon, a patient has had an initial consultation with an orthodontist, because patients usually seek out orthodontic consultation first, and the orthodontist refers them for surgical evaluation. Once evaluations have been completed by both professionals, they must confer to align treatment goals, establish estimated timelines, sequence, and phases of treatment.
For evaluation and treatment planning, routine panoramic radiographs as well as cephalometric radiographs and tracings are necessary. Panoramic radiographs are evaluated for presence or absence of teeth, impacted teeth, periodontal status, root relationships, bone pathology, or osseous temporomandibular joint pathology. Multitudes of cephalometric analyses exist. To evaluate maxillary deficiency, the cephalometric measurements that can be used include measurements to assess (1) AP position (sella-nasion-A-point [SNA], Pt A to Na perpendicular, Co-Pt), (2) vertical position (nasion to anterior nasal spine [ANS], ANS to Me, upper facial height [UFH]/lower anterior facial height [LAFH] ratio, AFH, posterior facial height [PFH], PFH/AFH ratio, U1-ANS), and (3) intermaxillary relationships (A point nasion B point [ANB] and Wits). The Wits analysis is used to establish the apical base relationship between the maxillary and the mandibular arches as measured along the occlusal plane. The Wits measurement is established by drawing a line from A point and B point, which proceeds perpendicular to the occlusal plane. If the B point line intersects the occlusal plane posterior to the A point line the Wits measurement is positive. If the B point line intersects the occlusal plane anterior to the A point line the Wits measurement is negative. The millimeter distance between the lines is the Wits measurement. Zero to plus one millimeter Wits is considered ideal.
Clinical database measurements, mounted models/model surgery, and clinical photographs are also used in this stage of treatment planning. Computerized tomography may be helpful in evaluation and planning but is not routinely performed at this time.
Treatment/Reconstructive Goals
The goal of any orthognathic surgery is to establish proper function and esthetics through establishment (and maintenance) of the appropriate form and position of the jaws, a Class I occlusion with appropriate buccal-lingual relationship and appropriate overlap and overjet with aesthetic vertical and soft tissue relationships. As stated earlier, the surgical correction of vertical and transverse maxillary deficiencies, in particular, are less stable procedures and therefore a major treatment goal includes mitigation of this inherent instability.
Specific Treatments and Techniques
Anterior Repositioning
The basic technique for Le Fort I osteotomy is as follows.
Local anesthetic with vasoconstrictor is injected into the maxillary mucobuccal fold prior to preparing and draping the patient. This allows time for the vasoconstrictor to take effect during scrubbing, preparation, and draping and prevents wasting time under general anesthesia without progress being made. A circumvestibular incision is made by incising horizontally through the buccolabial mucoperiosteum above the attached gingiva at the level of the maxillary teeth apices.
The incision extends from first molar to first molar. The parotid papilla must be identified and protected. As the cut is carried deeper, an effort must be made to remain inferiorly. The incision is made higher posteriorly and lowers anteriorly to avoid perforation into the nasal cavity.
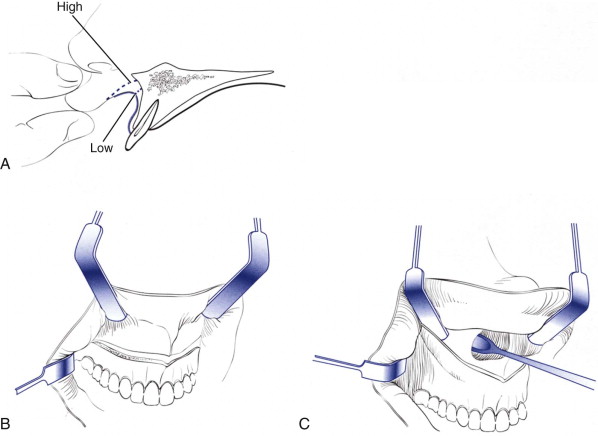
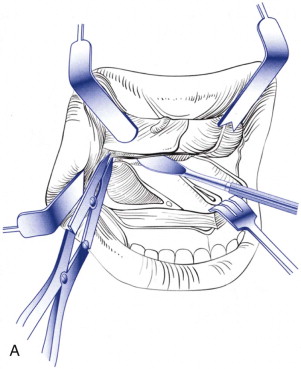
Usually the incision is made as a hemivestibular incision with subperiosteal dissection and exposure of each side individually. Subperiosteal dissection begins at the piriform rim and is carried superiorly and laterally along the anterior maxilla, exposing the infraorbital nerve as it exits the foramen. Posterior dissection, as it is carried behind the zygomatic buttress, must be tunneled inferiorly toward the mucogingival junction with maintenance of the subperiosteal plane, as it is carried back toward the pterygomaxillary fissure, to avoid vascular structures or exposure of the buccal fat pad. A toe-out retractor is placed behind the buttress and does not usually require being held. Dissection inside the piriform rim is started with a Woodson elevator and must be carried posteriorly with a Freer or periosteal elevator, including along the nasal floor ( Fig. 76-1, A to C ). Adequate elevation of this tissue is critical to prevent damage to it during the remainder of the procedure. Reference marks are made with a fissure bur for the purpose of vertical measurement.
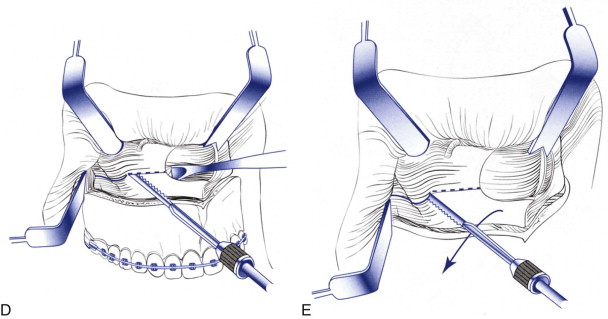
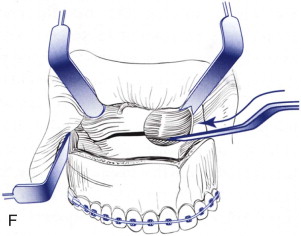
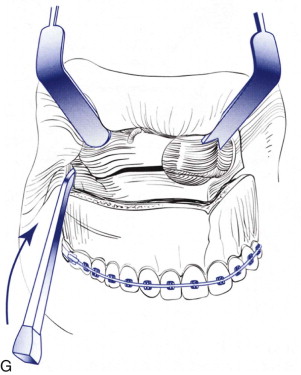
A reciprocating saw is used to make a horizontal osteotomy from the maxillary buttress to the piriform rim in the area above the apices of the teeth. The saw is turned around and an inside out cut is made behind the buttress ( Fig. 76-1, D and E ). Exactly the same procedure is carried out on the opposite side. A guarded osteotome is driven along the lateral nasal wall to a depth of approximately 20 mm to stop short of the descending palatine arteries. The nasal septum is separated from the nasal crest of the maxilla using a septal osteotome ( Fig. 76-1, F ). As it is driven posteriorly, care must be taken to direct it slightly inferiorly and maintain it in the midline. As the osteotome reaches the vomer, it will have a tendency to ride superiorly. The pterygoid plates are separated with a small, sharp osteotome ( Fig. 76-1, G ). This will sharply separate the pterygomaxillary junction in a controlled manner, rather than use of a broader more blunt osteotome, which can cause fracture. This osteotome, as well as spatula osteotomes used later, is sharpened before every procedure. The osteotome is directed as anteriorly, inferiorly, and medially as possible, with a finger placed palatally for palpation of complete separation.
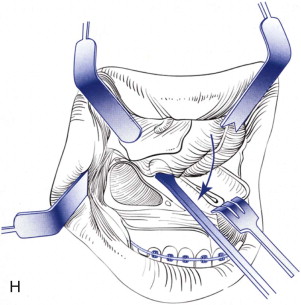
Once the completeness of these osteotomies is ensured, the maxilla is downfractured with moderate pressure on the anterior maxilla with the sharp end of a Senn retractor. As the maxilla is downfractured, the nasal mucoperiosteum is elevated posteriorly to the posterior edge of the hard palate ( Fig. 76-1, H ).
Often, the key feature in anterior repositioning of the maxilla is adequate mobilization. After downfracturing, the author routinely performs ligation and division of the descending palatine arteries (DPA). The blood flow to the distal segment of the maxilla has been shown to have no significant difference before and after ligation of the arteries. Ligation of the arteries decreases blood loss, allows removal of areas of potential bony interferences, frees a potential point of tethering mobility, and eliminates unintended or unrecognized damage of the DPA. He has not experienced an ischemic event as a result of dividing the DPA, even in segmental surgery. Prior to ligation, bony irregularities in the perpendicular plate of the palatine bone around the neurovascular bundle are carefully removed with a rongeur and a Woodson elevator ( Fig. 76-2, A ).
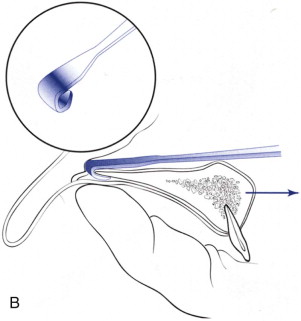
Mobilization of the maxilla can be performed in numerous ways. My preference is to either place a J stripper through the osteotomy and around the posterior hard palate and place traction, or place a Seldon retractor or Tessier retromaxillary levers behind the buttresses on either side and place forward pressure ( Fig. 76-2, B ). To ensure that the maxilla is adequately mobilized, the oral surgical splint is placed on the mandible, and the maxilla is demonstrated to be able to easily reach its necessary position in the splint and, in fact, exceed its necessary position in the splint, with traction on the arch wire with an Adson forceps. It is not possible to place heavy force for anterior traction with the Adson forceps, and therefore, if the appropriate position can be reached with this technique, the maxilla is well mobilized.
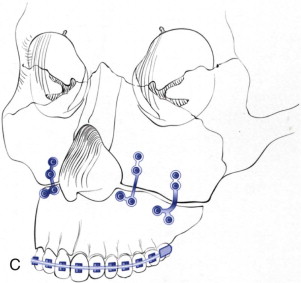
The maxilla is wired to the mandible using the prefabricated oral surgical split. The maxillomandibular complex is rotated, with care taken to seat the condyles. Bony interferences are removed until the desired vertical position is reached. The maxilla is secured in place using plates in the piriform and buttress regions bilaterally. Typically, 2.0- or 1.5-mm plates and screws are used ( Fig. 76-2, C ). The plates must be bent so that they are passive before placement of screws. The intermaxillary fixation is released and the occlusion is checked.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


