Introduction
The aim of this prospective study was to analyze the postexpansion positional changes of the maxillary halves and their initial stability after transpalatal distraction with a bone-borne distractor and standard corticotomies of the anterior, lateral, and median bony supports of the maxilla without pterygomaxillary disjunction.
Methods
The sample consisted of 21 patients (15 female, 6 male; mean age, 26 years 5 months). Measurements on the maxillary study casts and the posteroanterior cephalograms were obtained before surgery, at the end of palatal expansion, and 10 weeks later. No orthodontic treatment was initiated during the examination period.
Results
After palatal expansion, significantly wider measurements were noted in the canine (35.5%), premolar (26.3%), and molar (17.8%) regions. Angulation changes in the premolar (−7°) and molar (−8°) segments were observed. No significant changes were seen between the end of palatal expansion and 10 weeks later. Arch perimeter increased by 9.16% between presurgery and 10 weeks after the end of expansion.
Conclusions
The results indicated that more expansion was achieved anteriorly, and that there was buccal tipping of the split maxillary halves. Bone-borne surgically assisted rapid palatal expansion can provide significant expansion of the maxilla with an increase in arch perimeter, and it shows initial stability.
Highlights
- •
The effect of bone-borne transpalatal distraction on the maxilla was investigated prospectively.
- •
Measurements were performed on study casts and posteroanterior cephalograms.
- •
Nonparallel expansion was observed, with more expansion anteriorly.
- •
The maxillary halves tipped slightly buccally.
- •
Arch perimeter increased upon transpalatal distraction.
An adequate transverse maxillary dimension is a critical component of a stable and functional occlusion. A maxilla that is too narrow often creates problems such as tooth crowding, unesthetic buccal corridors, crossbite, and mouth breathing. Rapid palatal expansion is often used for these patients. The aim is to maximize the skeletal effects and minimize the dental effects.
Nonsurgical rapid palatal expansion is based on the idea of opening the midpalatal suture with a jackscrew. The devices are tooth-borne. The increase of the transverse dimension of the maxillary arch is achieved by separation of the 2 halves (orthopedic effect) and buccal movement of the posterior teeth and alveolar processes (orthodontic effect). It is important to start expansion before or during the growth spurt because facial suture lines become significantly more interdigitated and become either partially or totally fused with age. This procedure is indicated for children and young adolescents. Because the points of application of the transverse force are positioned much lower than the centers of resistance of the maxillary halves, there will be segmental buccal tipping of the maxillary halves. The same is true for the anchorage teeth because the point of force application is positioned lower than the center of resistance of the anchorage teeth.
In adults or patients who have passed their growth spurt, surgically assisted rapid palatal expansion (SARPE) is indicated. The expansion device can be tooth borne or bone borne. With the tooth-borne appliance, periodontal problems and problems relating to the orthodontic expansion—eg, tipping and extrusion of the anchorage teeth absorbing the forces—might occur. With a bone-borne appliance, the points of force application are closer to the centers of resistance of the maxillary halves. No forces need to be applied to individual teeth, and the buccal dentition maintains its original position in the bony segments. Therefore, most of the maxillary expansion is orthopedic and at a mechanically more desired level. Since the teeth are not involved in the appliance, it can be combined with orthodontic treatment.
Only a few prospective studies have reported on postdistraction changes and stability.
The objectives of this study were to analyze the postexpansion positional changes of the maxillary halves and to investigate the initial stability of their positions 10 weeks after inserting the blocking screw into the distractor.
The null hypotheses were the following: (1) there is no difference in the position of the maxillary halves before and immediately after transpalatal distraction, (2) there is no difference in the position of the maxillary halves immediately after distraction and 10 weeks later, and (3) there is no difference in the position of the maxillary halves before transpalatal distraction and 10 weeks after distraction.
Material and methods
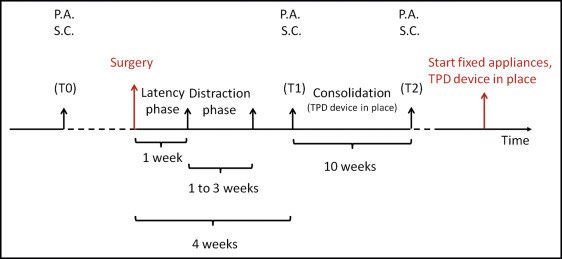
Twenty-one consecutive patients whose treatment plan involved transpalatal distraction were studied prospectively. Maxillary study casts and posteroanterior cephalograms were collected before surgery (T0), at the end of maxillary expansion (T1), and 10 weeks later (T2). Orthodontic alignment of the dental arches was started after the study period. Both dental and skeletal widths were evaluated, as well as buccal tipping. The study design is shown in Figure 1 .
The clinical trial was carried out at the Department of Maxillofacial Surgery of St John’s Hospital, Genk, Belgium, and included the normal follow-up of patients who received transpalatal distraction, but at standardized time points. Ethical approval from the university was obtained (reference number 2002/109). After we explained the purpose and duration of the study, all subjects signed a written consent form before participating in the study. The inclusion criteria for the patients were (1) need for skeletal bilateral transverse expansion of the maxilla; (2) female patients older than 15 years, and male patients older than 17 years; (3) permanent dentition; (4) no craniofacial congenital anomalies; and (5) no orthodontic appliances used during the study.
Over a period of 2 years, 21 patients met the inclusion criteria and volunteered to participate in the study. They ranged in age from 15 years 1 month to 44 years 6 months, with an average age of 26 years 5 months. There were 15 female and 6 male patients.
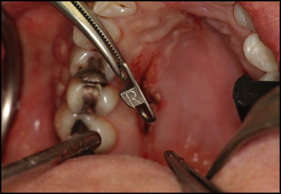
Surgery was performed by the same person for all patients under general anesthesia and nasoendotracheal intubation. The distractor used in this study was a transpalatal distractor (Surgi-Tec, Bruges, Belgium), a bone-borne device for surgically assisted rapid maxillary expansion. It was first introduced in 1999 by Mommaerts. Standard corticotomies were performed of the anterior, lateral, and median bony supports of the maxilla without pterygomaxillary disjunction. Midpalatal suture separation included loosening and disengagement of the anterior nasal spine and opening of the midpalatal suture between the maxillary central incisors. For mechanical advantage and patient comfort, the transpalatal distractor was placed as high as possible in the palatal vault. Abutment plates were inserted, left and right, between the roots of the second premolar and the first molar ( Fig 2 ). The distraction module was slightly activated to put the abutment plates in the correct positions against the palatal bone, after which they were fixated with titanium miniscrews. Activation was immediately performed until a diastema of 1 mm occurred between the central incisors ( Fig 3 ).

After surgery, the expansion screw was locked passively for 1 week. This latency period is the period from bone division to the onset of traction and is standard procedure. It is the time allowed for reparative callus formation. The bony segments at both ends of the gap were then progressively distracted over several days, ranging from 8 to 22 days (distraction phase). The expansion module has a color code (3 colors), and patients were instructed to turn it once a day by 120° until the next color appeared, starting 1 week after surgery. One activation of the screw opened the distraction module by 0.33 mm, so the distraction occurred at a rate of 1 mm in 3 days. When distraction is too fast, the collagen fibers might lose contact, and there is no ingrowth of new bone, causing nonunion or malunion. If distraction is too slow, premature consolidation can occur, and the required elongation cannot be obtained. Mean expansion time was 18 days, thus producing a mean expansion of the device of 6 mm. This procedure was continued until both arches were coordinated before surgical correction of the Class II and Class III malocclusions. Once the necessary expansion was achieved, the distractor was turned into a fixed retainer by inserting a blocking screw. The maxilla was not overexpanded, because movements of the bony halves should be stable when the distractor is left in situ passively during the consolidation phase. The distraction module was left in place for a mean retention period of 6 months (minimum, 4 months; maximum, 18 months). No distraction module was removed before the records were taken at T2. Fixed appliance therapy was started after T2 while the distraction device was still in situ. Expansion often creates space for the tongue to take a position in the palatal vault and thus prevent relapse. In the studies of Matteini and Mommaerts and Zahl and Gerlach, it was suggested that overcorrection is not necessary. Satisfactory results and long-term stability after surgically assisted rapid maxillary expansion depend on the orthodontist’s ability to obtain a functional and stable occlusion.
Casts were made for all patients at T0, T1, and T2. To prevent distortion of the impression, the distraction modules were blocked out with wax before the impressions were taken. Every cast was trimmed with the base parallel to the occlusal plane. Points from which measurements were to be taken were marked with a fine lead pencil to facilitate identification. Once marked, the casts were photographed from an occlusal view with a digital reflex dual CCD camera (Minolta, Osaka, Japan). A camera stand was used to support the casts and hold the camera at a fixed focal length from the occlusal plane of the casts. To provide a scale of distance, a millimeter rule was fixed at the heel of each cast at the level of the occlusal plane. After this procedure, the study casts were reduced on a model trimmer perpendicular to the occlusal plane: first from the front to the cusp tips of the first premolars and then from the back to the level of the mesial cusps of the first molars. These teeth were chosen because they are the anchor teeth in conventional SARPE procedures. Digital photographs were taken again using the standardized protocol as described above. The digital measurements on the photographs of the maxillary models were done with the software package Onyx Ceph (version 2.6.24, release 2.6.52; Image Instruments, Chemnitz, Germany) on a Pentium IV notebook (I power 5000; Packard Bell, Nijmegen, The Netherlands). Metric resolution of the software was 0.17 mm per pixel.
The landmarks were marked on the maxillary dental models as described by Adkins et al, and the following variables were measured.
- 1.
In the occlusal plane (linear measurements in millimeters) ( Figs 4 and 5 ): intercanine width ( Fig 4 ); interpremolar width ( Fig 4 ); intermolar width ( Fig 4 ); and arch perimeter, the sum of the lengths of the segments connecting the contact points on the mesial surfaces of the first molars, the contact points on the mesial surfaces of the first premolars, and the contact points on the distal surfaces of the central incisors ( Fig 5 ).
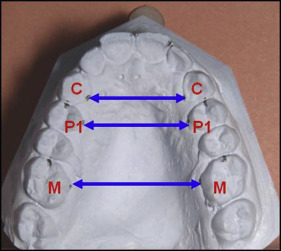
Fig 4 Linear measurements of interdental width on the study casts: C , Most lingual point at the gingival margin of the maxillary canine; P1 , most lingual point at the gingival margin of the maxillary first premolar; M , most lingual point at the gingival margin of the maxillary first molar.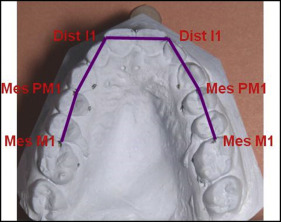
Fig 5 Arch perimeter measurement: Dist I1 , Distal surface of the maxillary central incisor; Mes PM1 , mesial surface of the maxillary first premolar; Mes M1 , mesial surface of the maxillary first molar. - 2.
In the frontal plane (angular measurements in degrees) ( Fig 6 ): premolar inclination and molar inclination.
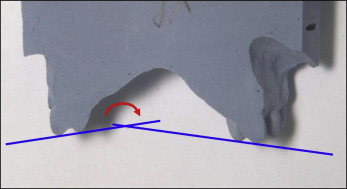
Fig 6 Construction of tangents and angular measurements. Tangents were constructed through the highest points of the mesial and palatal cusps of the first premolars and the mesiobuccal and mesiopalatal cusps of the first molars.
Posteroanterior cephalograms were taken of all patients at T0, T1, and T2. All cephalograms were taken at St John’s Hospital with the same roentgen equipment and magnification factor. All cephalograms were scanned (cobrascan CX-312T, large-format 12-bit x-ray digitizer; Radiographic Digital Imaging, Torrance, Calif; www.cobrascan.com ) and digitized with an XScan32 software package (Radiographic Digital Imaging). After digitizing, all cephalograms were analyzed using the Onyx Ceph cephalometric software package on the Pentium IV notebook.
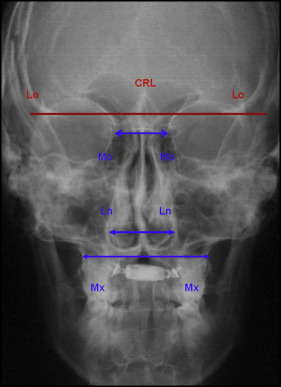
The following variables were measured parallel to the cranial base reference line, drawn according to the method of Mossaz-Joëlson and Mossaz ( Fig 7 ): medio-orbital width, nasal cavity width, and maxillary width.
Statistical analysis
To evaluate possible errors in landmark identification, photographic magnification, and digitization of the measurements by the investigator (E.G.), 10 randomly chosen maxillary study casts were photographed and digitized at 1 time. The same 10 study casts were photographed and digitized again after 1 week by the same investigator. Measurements were performed on both sets by the same investigator. On the first set, measurements were also made by a second investigator (B.V.V.). Pearson correlation coefficients were determined for every variable measured on the maxillary casts. The same procedure was used for the posteroanterior cephalograms.
Statistical calculations were performed with a software package (SPSS for Windows, version 14.0; SPSS, Chicago, Ill). Significance for all statistical tests was predetermined at P <0.05.
Descriptive statistics were determined for each variable at all 3 time points. A longitudinal study was considered with repeated measurements, in which each variable was observed at 3 time points: T0, T1, and T2 (within-subject factors). Statistical comparisons were made to calculate the changes over time for each variable and test them for statistically significant differences. Statistically significant differences were tested with the parametric 1-way repeated measures analysis of variance test for normal distributions.
Results
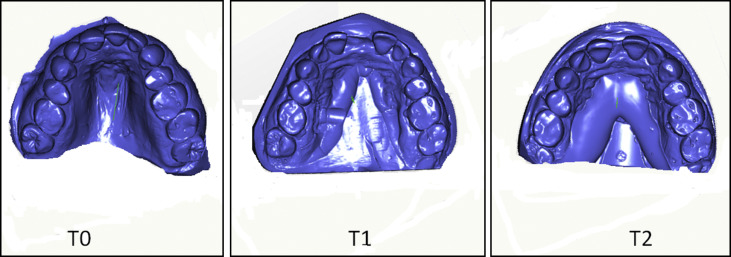
For each patient, the required amount of expansion on the basis of the treatment plans was achieved. No clinical complications were encountered during the observation period. Figure 8 depicts consecutive models of 1 patient at T0, T1, and T2.
All variables at all time points were tested for normal distribution with the Kolmogorov-Smirnov 1-sample test. All variables showed a normal distribution; therefore, parametric tests could be used.
For all variables of 10 randomly chosen maxillary casts and posteroanterior cephalograms, intraexaminer repeatability with a Pearson correlation coefficient higher than 0.9 and interexaminer repeatability with a Pearson correlation coefficient higher than 0.8 were found. These strong correlations between the first and second measurements made by the investigators (E.G. and B.V.V) indicated that the digitizing process, the identification of the landmarks on the maxillary casts and the posteroanterior cephalograms, and the measurements were done in a reproducible way.
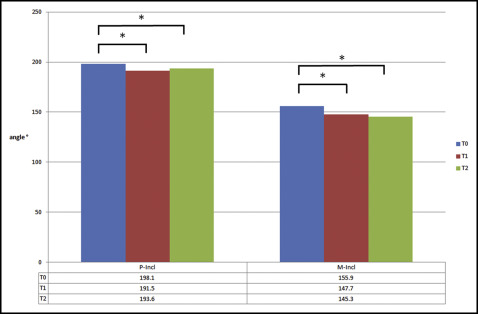
Figure 9 shows the differences between the time points of the linear measurements. Figure 10 shows the differences between time points of the angular measurements.
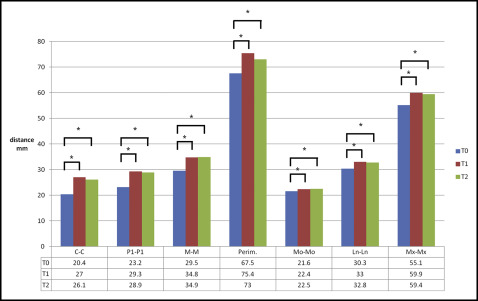
The results of the descriptive statistics are given in Table I .
| Variable | Time | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| C-C (mm) | T0 | 20.4 | 2.71 | 13 | 27 |
| T1 | 27.0 | 2.77 | 21 | 32 | |
| T2 | 26.1 | 2.99 | 20 | 33 | |
| P1-P1 (mm) | T0 | 23.2 | 2.52 | 18 | 28 |
| T1 | 29.3 | 2.79 | 24 | 34 | |
| T2 | 28.9 | 3.45 | 24 | 38 | |
| M-M (mm) | T0 | 29.5 | 3.88 | 19 | 36 |
| T1 | 34.8 | 3.69 | 27 | 43 | |
| T2 | 34.9 | 4.01 | 26 | 42 | |
| Perimeter (mm) | T0 | 67.5 | 6.73 | 51.2 | 78.5 |
| T1 | 75.4 | 6.27 | 61.7 | 83.9 | |
| T2 | 73.0 | 6.56 | 59.6 | 82.3 | |
| P-Incl (°) | T0 | 198.1 | 12.80 | 180.0 | 226.0 |
| T1 | 191.5 | 14.68 | 167.3 | 220.4 | |
| T2 | 193.6 | 15.24 | 162.4 | 219.6 | |
| M-Incl (°) | T0 | 155.9 | 15.79 | 120.0 | 182.0 |
| T1 | 147.7 | 16.51 | 104.3 | 173.8 | |
| T2 | 145.3 | 17.26 | 109.8 | 171.8 | |
| Mo-Mo (mm) | T0 | 21.6 | 1.61 | 18.4 | 24.5 |
| T1 | 22.4 | 1.45 | 19.5 | 24.6 | |
| T2 | 22.5 | 1.58 | 19.5 | 24.5 | |
| Ln-Ln (mm) | T0 | 30.3 | 2.08 | 26.3 | 33.4 |
| T1 | 33.0 | 2.55 | 27.0 | 37.5 | |
| T2 | 32.8 | 2.66 | 26.3 | 37 | |
| Mx-Mx (mm) | T0 | 55.1 | 3.93 | 45.0 | 60.1 |
| T1 | 59.9 | 4.14 | 47.2 | 66.5 | |
| T2 | 59.4 | 3.74 | 48.2 | 63.3 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


